 |
Glob Reg Health Technol Assess 2025; 12: 80-88 ISSN 2283-5733 | DOI: 10.33393/grhta.2025.3365 ORIGINAL RESEARCH ARTICLE |
 |
Assessing the economic burden of Waldenström’s Macroglobulinemia (WM), Marginal Zone Lymphoma (MZL), and Chronic Lymphocytic Leukemia (CLL)
ABSTRACT
Introduction: In Italy, Non-Hodgkin Lymphomas (NHL), including Waldenström’s Macroglobulinemia (WM), Marginal Zone Lymphoma (MZL), and Chronic Lymphocytic Leukemia (CLL), are among the most common hematologic cancers. These conditions mainly affect the elderly, who often have multiple comorbidities, complicating management and imposing significant burdens on patient quality of life and healthcare systems.
Objective: This study aimed to estimate the economic burden of selected B-cell lymphomas in Italy, providing insights for decision-makers to improve patient management and resource allocation.
Method: Data from the Italian Hospital Discharges Records (SDO) and the National Institute for Social Security were analyzed to estimate direct healthcare costs and social security costs from 2016 to 2019.
Results: A total of 93,712 hospital discharges were recorded, with MZL being the most common diagnosis, followed by CLL and WM. Most patients were male, and the 70–79 age group was most prevalent. MZL had the highest costs, followed by CLL and WM. Adverse events notably increased total expenditures, with variations across different pathologies. Direct healthcare costs totaled 533.6 million euros, while social security costs amounted to 240.9 million euros.
Conclusion: This study highlights the significant economic burden of selected B-cell lymphomas in Italy. Effective management strategies are crucial for reducing costs and optimizing resource allocation in the healthcare system.
Keywords: Direct costs, Economic Burden, Waldenström’s Macroglobulinemia (WM), Marginal Zone Lymphoma (MZL), Chronic Lymphocytic Leukemia (CLL), Indirect costs, Italy, Real-World Evidence.
Received: October 30, 2024
Accepted: February 5, 2025
Published online: March 11, 2025
Corresponding author:
Matteo Scortichini
email: matteo.scortichini@uniroma2.it
Global & Regional Health Technology Assessment - ISSN 2283-5733 - www.aboutscience.eu/grhta
© 2025 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
B-cell malignancies are the most common types of blood cancer and encompass over 40 different diseases caused by the uncontrolled proliferation of B cells (1). They not only represent the most diagnosed hematologic cancers worldwide, with 544,000 cases of non-Hodgkin lymphoma in 2020, but also contribute significantly to morbidity, with 260,000 deaths reported globally in the same year (2). Among NHL ‘, which in Italy represent the fifth most common cancer in men and the sixth in women (3), WM, MZL, and CLL represent frequently occurring diseases which normally run an indolent clinical course and which witnessed important therapeutic advances.
Waldenström’s Macroglobulinemia (WM) is a relatively rare type of NHL with an average age of 70 years at diagnosis (4). According to estimates in a European standard population, the annual incidence rates are 0.7 per 100,000 in males and 0.4 per 100,000 in females (5).
CLL accounts for approximately one-third of new leukemia cases worldwide and primarily affects individuals with an average age of 70 years. In Italy, the incidence is estimated at between 5.0 and 5.5 cases per 100,000 men and between 3.5 and 4.0 cases every 100,000 women (3).
MZL is a group of infrequent, slow-progressing B-cell NHL that arise in the marginal zones of the lymphatic tissue. It is diagnosed in older individuals, with an average age ranging from 60 to 70 years. In Europe, the incidence of MZL is estimated to be between 2–3 per 100,000 annually (6).
Together, these subtypes represent a considerable portion of all B-cell malignancies; they are commonly characterized by prolonged survival, marked by repeated treatment cycles due to frequent relapses (6).
These conditions, with their chronic nature, predominantly affect the elderly population and frequently coincide with multiple comorbidities (7,8). This complexity leads to intricate management and significant implications for both patient quality of life and the national healthcare system (9). According to available studies, the economic burden of NHL is higher than that of other types of cancer; a significant portion of the costs is related to hospital inpatient services and office-based visits (10,11).
When patients are asymptomatic, clinicians may defer treatment until symptomatic manifestations of the disease emerge with its advancement (1,5,12). However, delaying treatment can result in heterogeneous clinical outcomes (12,13). This challenge can be mitigated by early detection and the implementation of effective disease management protocols (5,12). Therefore, it is crucial to collect population-level data on the disease and conduct economic evaluations to inform healthcare policies.
In this regard, this study aimed to estimate the economic burden of these conditions within the context of the Italian healthcare system, providing relevant information for decision-makers toward better patient management and appropriate resource allocation.
Materials and methods
Data sources
This study was conducted using two different data sources to estimate separately direct health care costs and social security costs.
Italian Hospital Discharges Records (SDO)
The analysis of direct health care costs was carried out using the Hospital Discharges Records (SDO) for Italy as a whole (60 million inhabitants); data were available from 2016 to 2019. The Italian SDO records all hospital discharges (HD), both ordinary and day-hospital (DH), from public and accredited hospitals. Each record contains, together with a patient-specific anonymous code, the patient’s demographic (age, sex, residence) and clinical information (primary and up to five secondary diagnoses and procedures, Diagnosis-Related Group – DRG) (14).
National Institute for Social Security
The database of the National Social Security System (INPS) collects all applications related to both welfare benefits for the whole population, and social security benefits for workers only (15). Regarding welfare benefits, all applications resulting in the recognition of the Attendance Allowance (AA) were considered. The AA is a financial benefit for individuals who are severely disabled or totally incapacitated, necessitating permanent assistance for walking or carrying out daily life activities. This benefit is irrespective of age and income status but requires a total disability (100%) to be recognized, leading to the need for constant care. Data were available for the period 2016–2019 and only for adult subjects. In the context of social security benefits, the Social Security System (SSS) provides financial support to workers dealing with disabilities or chronic physical and/or mental impairments, with this support primarily funded by the workers’ own contributions. Specifically, individuals in any employment category registered with the INPS are eligible to apply for one of two available social security benefits in the event of an accident or illness: the Disability Benefit (DB), designated for those whose capacity to work is diminished to less than one-third (indicating a disability between 67% and 99%); and the Incapacity Pension (IP), awarded to individuals who are determined to be absolutely and permanently unable to perform any work activity, equating to a 100% disability rating.
Methods
Direct health care costs
Patients suffering from selected forms of B-cell lymphomas (CLL, MZL, and WM) were identified based on considering all the subjects aged 40 years or over, with at least one HD with a primary or secondary diagnosis, including one of the ICD9CM codes reported in Table 1.
| Disease | ICD9CM code | Description |
|---|---|---|
| CLL | 204.1 | Chronic lymphoid leukemia |
| MZL | 202.80 | Other malignant lymphomas unspecified site |
| 202.81 | Other malignant lymphomas involving lymph nodes of head face and neck | |
| 202.83 | Other malignant lymphomas involving intra-abdominal lymph nodes | |
| 202.84 | Other malignant lymphomas involving lymph nodes of axilla and upper limb | |
| 202.85 | Other malignant lymphomas involving lymph nodes of inguinal region and lower limb | |
| 202.86 | Other malignant lymphomas involving intrapelvic lymph nodes | |
| 202.87 | Other malignant lymphomas involving spleen | |
| 202.88 | Other malignant lymphomas involving lymph nodes of multiple sites | |
| WM | 273.3 | Macroglobulinemia |
Descriptive analysis was conducted to report the distribution of patients by sex, age group (40–49, 50–59, 60–69, 70–79, 80+), and pathology. Then, using a cross-sectional approach, the expenditure incurred by the National Health Service (NHS) for hospitalizations was estimated. Costs were stratified by cause of admission, considering separately the admissions strictly related to the pathology (all admissions reporting a primary or secondary diagnosis among those listed in Table 1) and those related to adverse events. Hospitalizations for adverse events were identified through the presence of pathology-specific DRG codes. These codes are listed in Table S1 (Supplementary material). If a hospitalization included both the diagnosis related to the pathology and a DRG for an adverse event, the cost was attributed to the adverse event.
Finally, a longitudinal analysis was conducted on patients discharged during the year 2016. For each of these patients, the first pathology-specific hospital admission was selected in chronological order (index event). From this date, a 3-year follow-up was initiated to estimate the expenditure associated with the pathology (including the one related to the index event). Admissions related to pathology and those for adverse events were selected according to the previously stated criteria. Patients exited the follow-up before the end of the 3-year observation period only in the case of in-hospital death. Only patients discharged alive after the index event were included in the analysis.
Social security costs
The analysis of social security costs was restricted to patients with MZL and CLL (data on WM not available). In this case, the distribution of the number of subjects that were granted a social benefit during the 4-year period from 2016 to 2019 was also reported. The data were stratified by age group (same categories as above), sex, and pathology. Following a method described elsewhere (16), social security beneficiaries and related costs were estimated through a probabilistic model with a Monte Carlo simulation, as to obtain the number of prevalent cases from the incident ones. Costs were estimated by year of calendar and type of social security benefit (DB, IP, or AA).
Results
Direct health care costs
During the study period, 93,712 HD were observed; none of these reported two or more ICD9CM codes related to more than one studied pathology (Table 2). The highest frequency was observed for MZL (55,826 HD), followed by CLL (35,023) and WM (2,863). Three out of five patients were men, with a constant gender ratio regardless of the pathology. The most represented age group was “70–79” (30.7%), followed by “80+” (24.1%) and “60–69” (23.9%), while the least numerous was “40–49” (6.7%). In this case, as well, the distribution is comparable between CLL and WM, while for MZL, a generally younger population was observed, with a lower number of admissions than average in the “80+” (16.2%) and “70–79” (28.3%) categories, in favor of the others.
Patients with a diagnosis of MZL in the study period were 31,546, followed by CLL (20,482) and WM (1,972, Table 3). Costs related to MZL were equal to over 340.6 million euros, while CLL and WM accounted for 177.7 and 15.2 million euros, respectively. The impact of adverse events on total expenditure was found to be highly heterogeneous across the pathologies, with values ranging from 21.6% for CLL to 60.2% for WM. A strong, negative trend in the number of both patients and HD was found across all pathologies, with the lowest reduction observed for CLL (−14.9% of patients, −16.2% of HD) and the highest in MZL (−23.6% patients, −23.3% HD).
On average, a patient with CLL incurred costs of €10,412 by the end of the 3-year follow-up (Fig. 1). Of these, €8,092 (77.8%) were related to the pathology, and €2,320 (22.2%) to adverse events. In the first month of follow-up, the expenditure had already exceeded €5,000, this mainly due to the index event, and then increased with a relatively steady path. Of the 7,184 patients admitted in 2016, only 6,743 contributed to the longitudinal analysis, highlighting an in-hospital mortality rate at the index admission of 6.1%, to which another 1,393 deaths were added during the follow-up.
Costs were slightly higher in patients with MZL, reaching €12,719 during the last month of follow-up (Fig. 2), with adverse events accounting for 27.1% of it. Expenditure rose rapidly during the first 12 months of follow-up, after which its growth rate slowed down in the subsequent two years. In-hospital mortality at index event was equal to 6.0%, with other 1,806 deaths observed along the follow-up.
| Group | Disease | |||
|---|---|---|---|---|
| CLL | MZL | WM | Overall | |
| Overall | 35,023 (100.0%) | 55,826 (100.0%) | 2,863 (100.0%) | 93,712 (100.0%) |
| Sex | ||||
| Males | 21,306 (60.8%) | 32,027 (57.4%) | 1,745 (61.0%) | 55,078 (58.8%) |
| Females | 13,717 (39.2%) | 23,799 (42.6%) | 1,118 (39.0%) | 38,634 (41.2%) |
| Age group | ||||
| 40–49 | 1,032 (2.9%) | 5,164 (9.3%) | 63 (2.2%) | 6,259 (6.7%) |
| 50–59 | 3,010 (8.6%) | 10,485 (18.8%) | 254 (8.9%) | 13,749 (14.7%) |
| 60–69 | 6,562 (18.7%) | 15,314 (27.4%) | 516 (18.0%) | 22,392 (23.9%) |
| 70–79 | 11,911 (34.0%) | 15,801 (28.3%) | 1,031 (36.0%) | 28,743 (30.7%) |
| 80+ | 12,508 (35.7%) | 9,062 (16.2%) | 999 (34.9%) | 22,569 (24.1%) |
CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma; WM: Waldenström’s macroglobulinemia.
| Disease | Year | Patients | HD | |||||
|---|---|---|---|---|---|---|---|---|
| Disease specific | Adverse events | Total | ||||||
| N | Cost | N | Cost | N | Cost | |||
| CLL | 2016 | 7,184 | 9,589 | 38,988,782 € | 3,043 | 10,047,316 € | 12,632 | 49,036,098 € |
| 2017 | 6,735 | 8,909 | 34,598,500 € | 2,988 | 9,571,661 € | 11,897 | 44,170,161 € | |
| 2018 | 6,447 | 8,421 | 33,585,519 € | 2,992 | 9,539,732 € | 11,413 | 43,125,251 € | |
| 2019 | 6,117 | 7,806 | 32,059,982 € | 2,781 | 9,260,309 € | 10,587 | 41,320,291 € | |
| Total | 20,482 | 34,725 | 139,232,783 € | 11,804 | 38,419,018 € | 46,529 | 177,651,801 € | |
| MZL | 2016 | 11,017 | 11,163 | 72,369,878 € | 9,504 | 24,843,153 € | 20,667 | 97,213,031 € |
| 2017 | 9,702 | 9,534 | 65,207,676 € | 9,066 | 22,600,121 € | 18,600 | 87,807,797 € | |
| 2018 | 8,688 | 8,258 | 58,070,267 € | 8,038 | 20,481,599 € | 16,296 | 78,551,866 € | |
| 2019 | 8,415 | 8,424 | 57,627,223 € | 7,425 | 19,417,072 € | 15,849 | 77,044,295 € | |
| Total | 31,546 | 37,379 | 253,275,044 € | 34,033 | 87,341,945 € | 71,412 | 340,616,989 € | |
| WM | 2016 | 652 | 431 | 1,574,899 € | 642 | 2,638,029 € | 1,073 | 4,212,928 € |
| 2017 | 618 | 456 | 1,753,828 € | 546 | 2,368,272 € | 1,002 | 4,122,100 € | |
| 2018 | 526 | 370 | 1,276,664 € | 484 | 2,146,379 € | 854 | 3,423,043 € | |
| 2019 | 519 | 380 | 1,478,727 € | 478 | 2,056,732 € | 858 | 3,535,459 € | |
| Total | 1,972 | 1,637 | 6,084,118 € | 2,150 | 9,209,412 € | 3,787 | 15,293,530 € | |
CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma; WM: Waldenström’s macroglobulinemia.
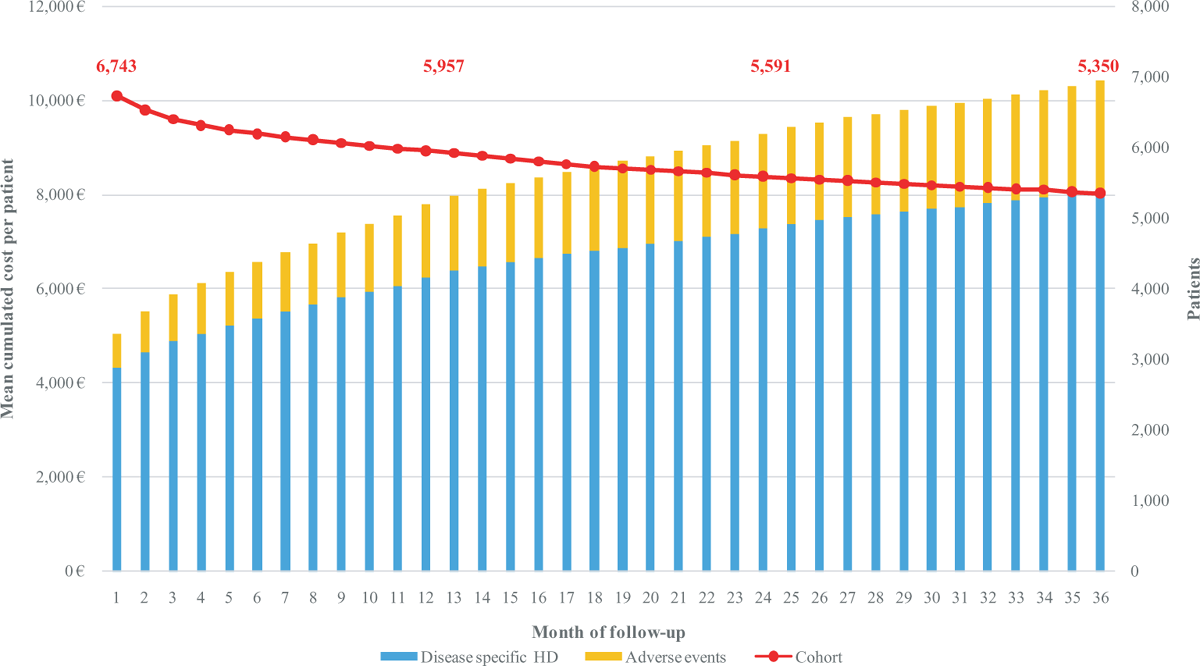
FIGURE 1 - Mean monthly cumulated cost per patient with CLL.
CLL: chronic lymphocytic leukemia
The expenditure per patient with WM was significantly lower, reaching €8,928 at the end of the follow-up. As a result of the cross-sectional analysis, in this cohort, the burden of adverse events was higher than that of HD related to the pathology (64.0%). This was already observed in the first month of follow-up, with the expenditure for adverse events representing 52.2% of the total (Fig. 3). In-hospital mortality during the index event was equal to 6.9%, while deaths during the follow-up were 113.
Social security costs
Overall, 1,266 social security benefits related to CLL and 4,279 for MZL were observed during 2016–2019; for a total of 5,545 (Table 4). Males represented 55.1% of overall applicants, the most represented age group was “80+”, followed by “70–79” (23.2%) and “60–69” (22.7%), while only 9.1% of applicants belonged to the “40–49” group. Most of the applications were recognized as AA (75.5%), followed by DB (22.3%) and IP (2.3%). Distribution by sex and age was consistent across pathologies, while a difference was observed in the type of recognition, with a higher weight of DB (38.9%) and a lower weight of AA (58.4%) with respect to the average in the CLL population.
Estimated annual prevalent beneficiaries of social security benefits for CLL were 2,015; of these, 1,031 (51.2%) were acknowledged as DB, 110 (5.5%) as IP and 875 (43.4%) as AA. A slight increase in the number of DB and a modest reduction in AA was observed (Fig. 4). Beneficiaries with MZL were 5,898, with AA being the most frequent type of recognition (68.9%), followed by DB (26.4%) and IP (4.8%); no significant trends were observed.
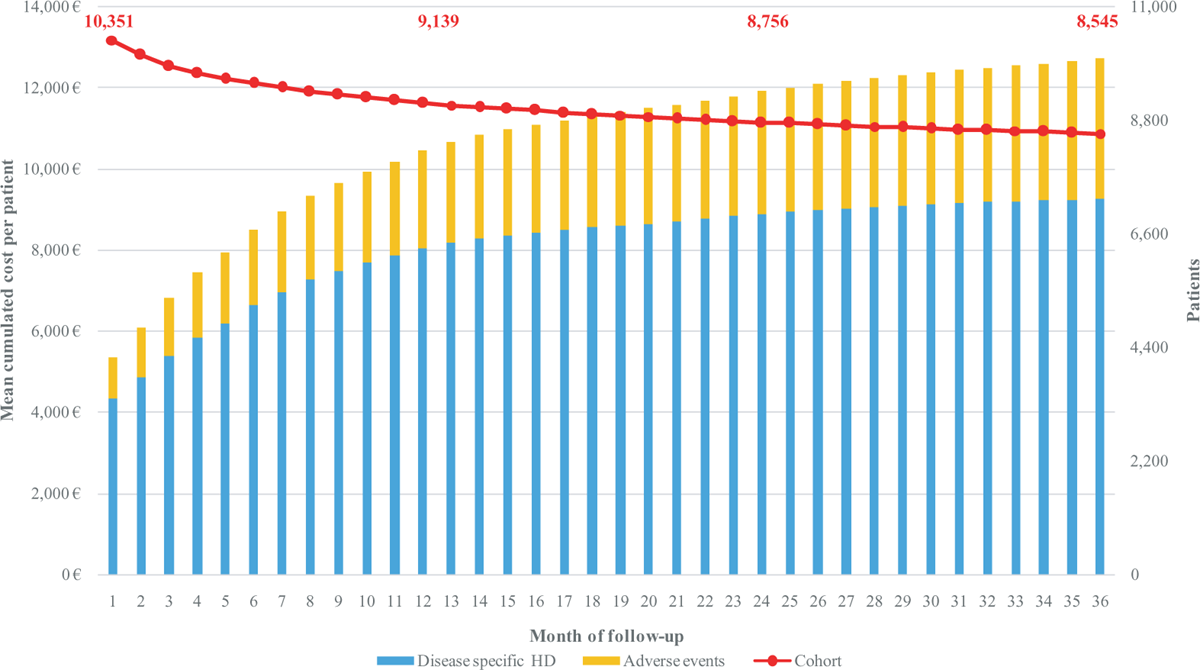
FIGURE 2 - Mean monthly cumulated cost per patient with MZL.
MZL: marginal zone lymphoma
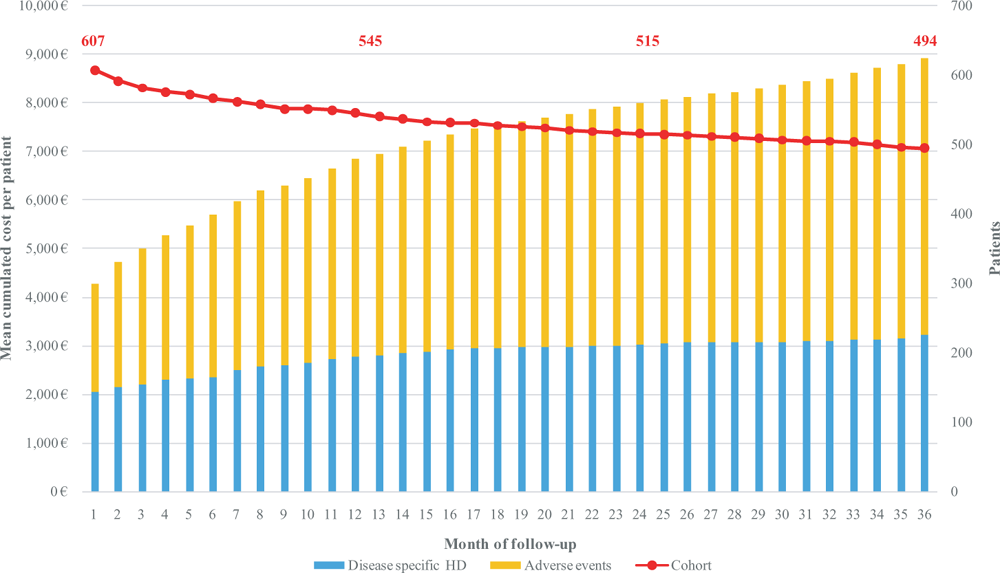
FIGURE 3 - Mean monthly cumulated cost per patient with WM.
WM: Waldenström’s macroglobulinemia
On average, during the study period, an expenditure equal to over €240.9 million was estimated (€ 60.2 million each year, Table 5). Of these, €174.4 million were related to MZL and €66.5 million to CLL. Annual trends were equal to the ones described for the number of beneficiaries (each recognition provides equal compensation for every beneficiary, regardless of income).
Discussion
To our knowledge, no other studies have evaluated the economic impact of NHL in Italy. Such evaluation assumes particular significance considering the peculiarities of this cancer type, which, despite affording patients a good survival rate, requires frequent monitoring and may be characterized by recurrent relapses. Thus, it is essential to evaluate not only direct healthcare expenditures but also indirect costs to comprehensively understand the economic implications of these pathologies.
In our study, the characteristics related to age and gender of the patients, with a predominance of males (2/3 of hospitalizations) in the age group of 70–79 (except for patients with MZL, who are on average younger), reflect findings consistent with those of other national and international studies (1-4).
| Group | Disease | ||
|---|---|---|---|
| CLL | MZL | Overall | |
| Overall | 1,266 (100.0%) | 4,279 (100.0%) | 5,545 (100.0%) |
| Sex | |||
| Males | 744 (58.8%) | 2,314 (54.1%) | 3,058 (55.1%) |
| Females | 522 (41.2%) | 1,965 (45.9%) | 2,487 (44.9%) |
| Age group | |||
| 40–49 | 97 (7.7%) | 408 (9.5%) | 505 (9.1%) |
| 50–59 | 304 (24.0%) | 884 (20.7%) | 1,188 (21.4%) |
| 60–69 | 279 (22.0%) | 978 (22.9%) | 1,257 (22.7%) |
| 70–79 | 208 (16.4%) | 1,080 (25.2%) | 1,288 (23.2%) |
| 80+ | 378 (29.9%) | 929 (21.7%) | 1,307 (23.6%) |
| Type of recognition | |||
| DB | 492 (38.9%) | 743 (17.4%) | 1,235 (22.3%) |
| IP | 35 (2.8%) | 90 (2.1%) | 125 (2.3%) |
| AA | 739 (58.4%) | 3,446 (80.5%) | 4,185 (75.5%) |
CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma; DB: Disability benefit; IP: Incapacity pension; AA: Attendance allowance.
The number of patients affected by MZL was found to be higher than expected and reported in the literature. (3,12,17) For example, the annual incidence of MZL in Italy has been estimated at 2.7 per 100,000 individuals according to the Italian Association of Medical Oncology (3), which aligns with general European data (2–3 per 100,000) reported in ESMO guidelines (12). However, other studies, such as those included in the EUROCARE-5 database (18), report slightly lower incidences for comparable European countries, such as France and Spain, where the incidence is closer to 2 per 100,000. These variations may reflect differences in diagnostic criteria, healthcare access, and registry reporting practices.
Our findings, which show a higher-than-expected number of patients, could be influenced by factors such as improved diagnostic sensitivity, broader access to healthcare services, or demographic differences specific to the Italian population.
For all three pathologies under consideration, there was a decrease observed in both hospitalizations and the number of patients, consistent with findings reported in other national and international studies (3,19). This downward trend appears to be linked to a higher frequency of early diagnoses, the availability of effective treatments (20,21).
From our study, it emerged that patients with a higher number of hospitalizations were those affected by MZL, followed by patients diagnosed with CLL and WM. For all three conditions, and particularly for WM, a significant percentage of hospitalizations due to adverse events and acute situations has been noted. Other studies have previously reported a significant number of acute hospitalizations for these patients, particularly in the year following diagnosis (22,23). The authors of these studies have suggested that this could be due to the nature of the diseases, which pose an increased risk of infections both from the diseases themselves and from anti-cancer treatments (24-26). Additionally, they propose that improving a multidisciplinary approach may help better address the additional health issues these patients may face.
The direct cost associated with the three pathologies amounted to 533.6 million euros over the study period. Patients with MZL exhibited the highest associated costs, amounting to €340,616,989, followed by CLL patients (177.7 million euros) and WM patients (15.3 million euros). Adverse event management accounted for approximately a quarter of the total cost for MZL and CLL (22.1% for MZL and 27.1% for CLL), whereas adverse events had a significant impact, representing 64% of the overall cost for WM patients (€9,209,412).
The significant percentage of adverse events is consistent with findings reported in previous literature (27-29). Notably, in the case of WM disease, the study from Sarosiek underscores the importance of customizing treatment based on individual patient characteristics to reduce the increased risk of adverse events associated with both the pathology and pharmacological interventions (29).
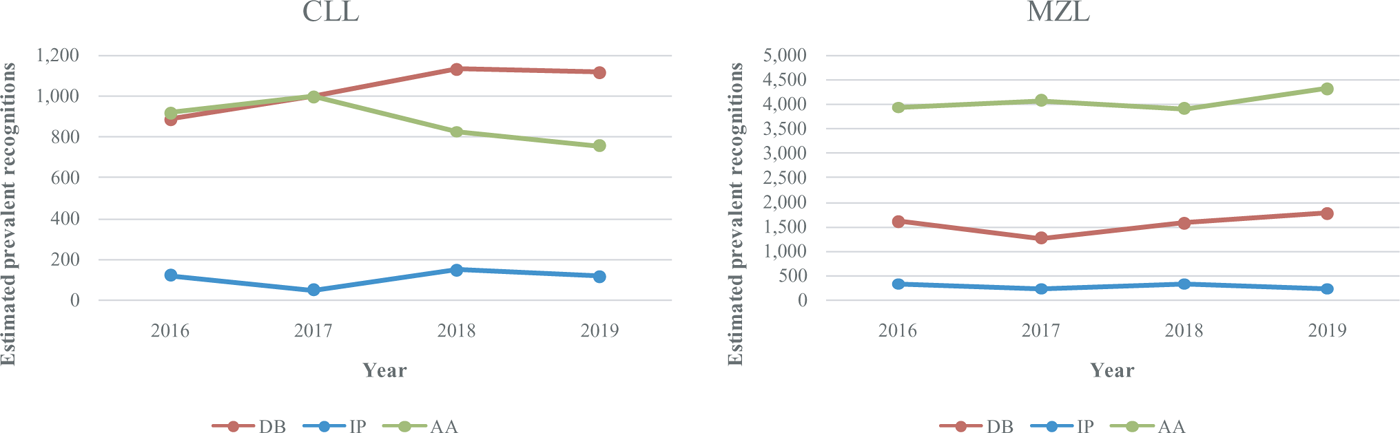
FIGURE 4 - Annual trend of estimated prevalent beneficiaries of social security benefits, by type of recognition and pathology
CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma
| Disease | Type of cost | Year | Total | |||
|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | |||
| CLL | DB | 8,240,354 € | 9,298,049 € | 10,662,539 € | 10,700,335 € | 38,901,276 € |
| IP | 1,647,112 € | 673,811 € | 2,030,948 € | 1,582,294 € | 5,934,165 € | |
| AA | 5,639,726 € | 6,174,023 € | 5,124,085 € | 4,701,243 € | 21,639,076 € | |
| Total social costs | 15,527,191 € | 16,145,883 € | 17,817,571 € | 16,983,872 € | 66,474,517 € | |
| MZL | DB | 14,995,959 € | 11,876,500 € | 14,800,240 € | 16,970,062 € | 58,642,761 € |
| IP | 4,447,202 € | 3,200,603 € | 4,400,386 € | 3,164,588 € | 15,212,780 € | |
| AA | 24,182,908 € | 25,215,687 € | 24,246,366 € | 26,884,353 € | 100,529,315 € | |
| Total social costs | 43,626,069 € | 40,292,790 € | 43,446,993 € | 47,019,004 € | 174,384,856 € | |
| Total | DB | 23,236,313 € | 21,174,549 € | 25,462,779 € | 27,670,397 € | 97,544,038 € |
| IP | 6,094,314 € | 3,874,415 € | 6,431,334 € | 4,746,882 € | 21,146,945 € | |
| AA | 29,822,634 € | 31,389,710 € | 29,370,451 € | 31,585,596 € | 122,168,391 € | |
| Total social costs | 59,153,261 € | 56,438,674 € | 61,264,564 € | 64,002,875 € | 240,859,374 € | |
CLL: chronic lymphocytic leukemia; MZL: marginal zone lymphoma; DB: Disability benefit; IP: Incapacity pension; AA: Attendance allowance.
Our study is the first to investigate the overall social costs induced by CLL, MZL and WM in Italy. While this represents a novel contribution in the Italian context, other studies have explored the economic burden of these diseases in different countries. For example, Pfeil et al. analyzed the economic impact of CLL in the UK, estimating an annual per-patient cost of £18,000, primarily driven by treatment expenses and hospitalizations, and underscored significant productivity losses due to disability and absenteeism (23). Similarly, Chanan-Khan et al. examined the real-world economic burden and healthcare disparities for CLL, MZL, and WM in the United States, reporting average annual healthcare costs of $69,000 for CLL patients and $85,000 for WM patients, including substantial expenditures on managing adverse events and prolonged hospital stays (26). Furthermore, Lutz et al. investigated the economic implications of adverse events in patients with indolent lymphomas, including MZL and CLL, in Germany. Their study highlighted that infections and hospitalizations contributed to a significant portion of the costs, with per-patient annual expenditures estimated at €30,000–€40,000, emphasizing the impact of disease-related complications on the healthcare system (24). These international studies provide valuable insights into the global economic burden of these diseases, illustrating common challenges such as frequent relapses, adverse events, and prolonged care requirements. However, their scope often focuses primarily on direct healthcare costs. In contrast, our study advances this field by integrating both direct healthcare costs (€533.6 million over four years) and comprehensive social costs (€240.9 million), including disability benefits and attendance allowances. This broader perspective on the economic impact of CLL, MZL, and WM offers a more holistic understanding of the financial challenges posed by these malignancies and underscores the necessity of comprehensive healthcare and social support strategies.
The care and assistance of cancer patients do not end with therapeutic treatments. The condition of fragility resulting from the disease entails specific social and economic requirements, which is why legal protections and economic benefits are provided for under the law.
The cost of these interventions contributes significantly to the economic impact of the pathology. Therefore, we believe that an added value of our work has been to include in the analysis the assessment of the cost to the SSS of the considered pathologies, despite being able to obtain data for only two out of the three forms of NHL.
Our study represents the first investigation into the collective social costs incurred by CLL, MZL, and WM in Italy. It underscores that the care and support for cancer patients extend beyond therapeutic interventions. The inherent fragility resulting from the disease necessitates specific social and economic provisions, as enshrined in legal protections and economic benefits.
The cost of these interventions significantly contributes to the overall economic impact of the pathology. Therefore, we posit that a key contribution of our work lies in assessing the SSS’s financial burden associated with these pathologies, even though data could only be obtained for two out of the three forms of NHL.
On average, the study period witnessed an expenditure related to social security benefits exceeding €240.9 million. Most applications were granted an AA (75.5%). This data underscores and corroborates the substantial impact these pathologies exert on patients, particularly evident in cases of MZL, where the recognition of an AA stood at 68.9%, signifying a considerable reliance on support from the SSS.
Thus, through our analysis of hospitalization and social security costs, this study provides valuable insights into the burden imposed by CLL, MZL, and WM in Italy, shedding light on crucial aspects of these diseases from two significant perspectives. Additionally, our findings underscore the considerable economic implications of social security costs, often overlooked in similar analyses.
It is important to acknowledge certain limitations of this study. The study relied on administrative healthcare databases, which may have limitations in terms of data accuracy and completeness. Administrative data sources are designed for accounting and billing purposes. Therefore, both datasets only include data considered relevant for accounting purposes, while information relevant to our scope could be missing. However, to date there are no specific epidemiological registries for measuring clinical outcomes and costs of patients with NHL; thus, administrative sources remain the best possible alternative for estimating costs related to hospital admissions and social security benefits within the Italian setting. Secondly, due to the lack of a specific ICD-9-CM code for MZL, the number of hospitalizations and the prevalence of beneficiaries of social security benefits could be overestimated. Unfortunately, no algorithm was found in the literature to identify MZL within the ICD9CM setting; to try to mitigate the bias, the analysis protocol and the selection criteria were revised and approved by a team of expert clinicians.
Disclosures
Conflicts of Interest: The authors have no relevant financial or non-financial interests to disclose.
Financial support: This study was funded by Beigene. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author contributions: All authors contributed to the study conception and developed the study design. MS and MP conducted the statistical analysis and derived the analytical results. The first draft of the manuscript was written by MS and AR. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1. Thandra KC, Barsouk A, Saginala K, et al. Epidemiology of Non-Hodgkin’s Lymphoma. Vol. 9, Medical sciences (Basel, Switzerland). 2021. CrossRef
- 2. Mafra A, Laversanne M, Gospodarowicz M, et al. Global patterns of non-Hodgkin lymphoma in 2020. Int J Cancer. 2022;151(9):1474–1481. CrossRef PubMed
- 3. AIOM AIRTUM. I numeri del cancro in Italia 2023. Online (Accessed October 2024)
- 4. Castillo JJ, Olszewski AJ, Cronin AM, et al. Survival trends in Waldenström macroglobulinemia: an analysis of the Surveillance, Epidemiology and End Results database. Blood. 2014;123(25):3999–4000. CrossRef PubMed
- 5. Buske C, Leblond V, Dimopoulos M, Kimby E, Jäger U, Dreyling M. Waldenström’s macroglobulinaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2013;24(SUPPL.6). CrossRef
- 6. Smith A, Crouch S, Lax S, et al. Lymphoma incidence, survival and prevalence 2004-2014: sub-type analyses from the UK’s Haematological Malignancy Research Network. Br J Cancer. 2015;112(9):1575–1584. CrossRef PubMed
- 7. Li S, Liu J, Bowers C, et al. Febrile neutropenia-related care and associated costs in elderly patients with breast cancer, lung cancer, or non-Hodgkin lymphoma. Support Care Cancer. 2020;28(1):113–122. CrossRef PubMed
- 8. Kenzik KM, Mehta A, Richman JS, et al. Congestive heart failure in older adults diagnosed with follicular lymphoma: A population-based study. Cancer. 2018;124(21):4221–4230. CrossRef PubMed
- 9. Kenzik KM, Williams GR, Bhakta N, et al. Healthcare utilization and spending among older patients diagnosed with Non-Hodgkin lymphoma. J Geriatr Oncol. 2021;12(8):1225–1232. CrossRef PubMed
- 10. Zakeri M, Li J, Sansgiry SS, et al. Incremental health care expenditures for non-Hodgkin lymphoma in comparison with other cancers: analysis of national survey data. J Manag Care Spec Pharm. 2023;29(5):480–489. CrossRef PubMed
- 11. Mounie M, Costa N, Conte C, et al. Costs of Hodgkin and Non-Hodgkin Lymphoma in France: Results on the Basis of the French National Health Insurance Database. Value Health. 2018;21:S25. CrossRef
- 12. Zucca E, Arcaini L, Buske C, et al; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Marginal zone lymphomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(1):17-29. CrossRef PubMed
- 13. Ardeshna KM, Smith P, Norton A, et al; British National Lymphoma Investigation. Long-term effect of a watch and wait policy versus immediate systemic treatment for asymptomatic advanced-stage non-Hodgkin lymphoma: a randomised controlled trial. Lancet. 2003;362(9383):516–522. CrossRef PubMed
- 14. Ministero della Salute. Il flusso informativo SDO. Online (Accessed October 2024)
- 15. INPS. Osservatorio sulle pensioni erogate dall’INPS. Online (Accessed October 2024)
- 16. Russo S, Mariani TT, Migliorini R, et al. The economic burden of musculoskeletal disorders on the Italian social security pension system estimated by a Monte Carlo simulation. Reumatismo. 2015;67(2):45–56. CrossRef PubMed
- 17. Cerhan JR, Habermann TM. Epidemiology of marginal zone lymphoma. Ann Lymphoma. 2021;5:5. CrossRef PubMed
- 18. Sant M, Minicozzi P, Mounier M, et al; EUROCARE-5 Working Group. Survival for haematological malignancies in Europe between 1997 and 2008 by region and age: results of EUROCARE-5, a population-based study. Lancet Oncol. 2014;15(9):931–942. CrossRef PubMed
- 19. Darbà J, Marsà A. Burden of Hodgkin and non-Hodgkin lymphoma in Spain over a 10-year period: productivity losses due to premature mortality. Expert Rev Pharmacoecon Outcomes Res. 2021;21(1):87–92. CrossRef PubMed
- 20. Cai W, Zeng Q, Zhang X, et al. Trends Analysis of Non-Hodgkin Lymphoma at the National, Regional, and Global Level, 1990–2019: Results From the Global Burden of Disease Study 2019. Front Med (Lausanne). 2021;8:738693. CrossRef PubMed
- 21. Miranda-Filho A, Piñeros M, Znaor A,et al. Global patterns and trends in the incidence of non-Hodgkin lymphoma. Cancer Causes Control. 2019;30(5):489–499. CrossRef PubMed
- 22. Rotbain EC, Rostgaard K, Andersen MA, et al. Healthcare Utilization and Comorbidity in Chronic Lymphocytic Leukemia. Clin Epidemiol. 2021;13:1155–1165. CrossRef PubMed
- 23. Pfeil AM, Imfeld P, Pettengell R, et al. Trends in incidence and medical resource utilisation in patients with chronic lymphocytic leukaemia: insights from the UK Clinical Practice Research Datalink (CPRD). Ann Hematol. 2015;94(3):421–429. CrossRef PubMed
- 24. Lutz C, Feiten S, Chakupurakal G, et al. Patients with indolent lymphomas are at high risk of infections: experience from a German outpatient clinic. BMC Immunol. 2023;24(1):2. CrossRef PubMed
- 25. Johnson PC, Yi A, Horick N, et al. Clinical Outcomes, Treatment Toxicity, and Health Care Utilization in Older Adults with Aggressive Non-Hodgkin Lymphoma. Oncologist. 2021;26(11):965–973. CrossRef PubMed
- 26. Chanan-Khan A, Yang K, Liu S, et al. Real-World Disease Burden, Costs and Resource Utilization of Hospital-Based Care Among Mantle Cell Lymphoma, Waldenström Macroglobulinemia, Marginal Zone Lymphoma and Chronic Lymphocytic Leukemia: Disparities and Risk Factors. Blood. 2021;138(Supplement 1). CrossRef
- 27. Kabadi SM, Goyal RK, Nagar SP, et al. Treatment patterns, adverse events, and economic burden in a privately insured population of patients with chronic lymphocytic leukemia in the United States. Cancer Med. 2019;8(8):3803–3810. CrossRef PubMed
- 28. Rosand CB, Valla K, Flowers CR, et al. Effective management strategies for patients with marginal zone lymphoma. Future Oncol. 2018;14(12):1213–1222. CrossRef PubMed
- 29. Sarosiek S, Treon SP, Castillo JJ. Reducing treatment toxicity in Waldenström macroglobulinemia. Expert Opin Drug Saf. 2021;20(6):669–676. CrossRef PubMed