 |
Glob Reg Health Technol Assess 2025; 12: 34-42 ISSN 2283-5733 | DOI: 10.33393/grhta.2025.3243 ORIGINAL RESEARCH ARTICLE |
 |
Cost of illness of Heart Valve Diseases (HVDs): A real-world analysis in Italy
ABSTRACT
Introduction: Heart valve diseases constitute a significant public health challenge with substantial clinical and economic implications. The ageing population, coupled with advancements in surgical techniques, has led to increased hospitalizations for cardiac valve interventions over the past decade. Despite progress, the economic burden of heart valve diseases remains underexplored, particularly in the context of the Italian healthcare system. This study aims to comprehensively assess the economic burden of heart valve diseases in Italy through a real-world analysis.
Methods: Using data from the national Italian Hospital Discharge Records (SDO), we identified the number of adult patients undergoing interventions on the aortic, mitral, and tricuspid valves, along with the associated costs borne by the National Health System. Additionally, we estimated indirect costs by analyzing social security benefit applications related to valve diseases from 2016 to 2019.
Results: A notable rise in hospitalizations for cardiac valve interventions, particularly for the aortic (+53.3%) and mitral valves (+29.5%) was revealed through the study period. In-hospital mortality rates declined, reflecting advancements in perioperative care. The economic burden of heart valve diseases in Italy was substantial, with hospitalization costs reaching €808 million in 2018. Social security benefit applications also increased, adding an annual cost of €29 million.
Conclusions: Heart valve diseases represent a growing clinical and socio-economic challenge in Italy. This study underscores the imperative for a multidisciplinary approach to effectively manage these conditions. Emphasizing prevention, early diagnosis, and timely interventions is crucial to mitigate the economic impact and enhance the quality of life for patients.
Keywords: Direct costs, Economic burden, Heart Valve Diseases (HVD), Indirect costs, Italy, Real-world evidence
Received: August 2, 2024
Accepted: January 14, 2025
Published online: February 19, 2025
Global & Regional Health Technology Assessment - ISSN 2283-5733 - www.aboutscience.eu/grhta
© 2025 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Diseases of the heart valves can be present from birth (congenital valve diseases) or develop throughout life as a result of various pathologies (1). These conditions involve a malfunction in controlling blood flow due to either damage or a defect in one of the four heart valves (mitral, aortic, pulmonary, and tricuspid) (2). The narrowing of heart valves leads to stenosis, while imperfect valve closure causes blood to flow back (regurgitation), resulting in insufficiency (2). Stenosis and insufficiency can occur individually or together and may affect one or more valves simultaneously (combined valve diseases) (1). The mitral and aortic valves, being subjected to higher pressure load, are more commonly affected than the tricuspid valve, which is rarely involved and typically refers to congenital anomalies (1). Symptoms caused by valve diseases can be managed with medications, but in cases of significant valve defects, reparative or replacement surgery for malfunctioning valves may be necessary (2).
Among valve diseases, aortic stenosis is the most common (3,4), with a prevalence of 2% in subjects over 65 years old (5) and a 12-month mortality rate exceeding 30% in treated symptomatic patients across in the western world (6). Mitral valve regurgitation also has a high prevalence, estimated at around 20 million cases worldwide, with 34,000 associated deaths in 2019 (6,7). A high heterogeneity in the prevalence rates of aortic valve regurgitation has been reported, ranging from 1.6% in a study conducted on the English population over 65 (8), to nearly 5.0% in an American cohort (9). Tricuspid valve regurgitation is the rarest disorder but is associated with a high mortality rate, estimated at 42% at 3 years, according to one study (10).
An Italian study found a prevalence of approximately 30% for mild to moderate valve diseases in the population over 65, a significantly higher figure than previous estimates. The study was based on newly diagnosed patients, often characterized by silent symptoms (11).
Few studies have estimated the direct costs of valve diseases. In the United States, annual direct costs were approximately $13,000 for symptomatic patients with aortic valve diseases and $5,000 for those with mitral valve diseases (12). An analysis of a cohort of patients affected by mitral valve regurgitation estimated an average annual cost of around €12,000 (13). Another study estimated direct costs for severe aortic stenosis patients undergoing valve replacement surgery at around €22,000 for Surgical Aortic Valve Replacement (SAVR) and €20,000 for Transcatheter Aortic Valve Implantation (TAVI) along a 2-year follow-up (14). The direct costs related to tricuspid valve diseases were estimated in another American study, quantifying the annual burden per patient ranging from $17,000 in patients who had not experienced heart failure or valve regurgitation to over $42,000 for patients with both outcomes (15).
In Italy, a study comparing the direct costs during a one-year follow-up for patients undergoing TAVI or SAVR estimated mean costs ranging from €2,000 to €3,000, with an additional €30,000 related to the intervention (16). Another Italian study comparing TAVI and Sutureless Aortic Valve Replacement (SU-AVR) estimated, over a 1,310-day follow-up, expenses between €20,000 and €24,000 (17).
Few studies have assessed the indirect costs of valve diseases. European data indicate a productivity loss cost of approximately €11,000 for patients and over €2,000 for caregivers following acute coronary syndrome or heart attack (18).
In Italy, indirect costs related to cardiovascular diseases are estimated to be around €4.5 billion annually, with an increasing trend over time (19).
While previous studies have explored the clinical and economic burden of Heart Valve Diseases (HVDs) in various contexts, there is a lack of comprehensive analyses that integrate both direct healthcare costs and indirect social security expenditures, particularly within the Italian healthcare system.
The aim of this study is to estimate the economic burden of HVDs in Italy through a real-world data analysis.
Data and methods
Data
This study was conducted using the Hospital Discharge Records (SDO) for Italy (60 million inhabitants), data were available from 2010 to 2018.
The Italian SDO records all Hospital Discharges (HD), both ordinary and Day-Hospital (DH), from public and accredited hospitals. Each record contains, together with a patient-specific anonymous code, the patient’s demographic (age, sex, residence) and clinical information (primary and up to five secondary diagnoses and procedures, Diagnosis-Related Group – DRG).
The National Institute for Social Security (INPS) database collects all applications related to welfare benefits; for this study, only applications resulting in the recognition of the Attendance Allowance (AA) were considered. The AA is a financial benefit for individuals who are severely disabled or totally incapacitated, necessitating permanent assistance for walking or carrying out daily life activities. This benefit is irrespective of age and income status but requires a total disability (100%) to be recognized, leading to the need for constant care. Data were available for the period 2016-2019 and only for adult subjects.
Both sources used in this analysis are administrative databases. SDO is used for regional reimbursement. Therefore, information collected in SDO is routinely controlled and certified by regional offices, in terms of accuracy and validity. The Ministry of Health in Italy has defined, in partnership with the Regions, the methodology for the assessment of the entire SDO database. The data collected represent a database of references that meet the monitoring and control requirements of the National Health Service with appropriate levels of accuracy, reliability, and timeliness. The INPS database of social security benefits is a highly reliable source for analyzing the accounting of social assistance measures in Italy. It is managed by the INPS, which ensures rigorous data collection, standardization, and validation processes.
Methods
The study population included all adult subjects undergoing interventions on the aortic, mitral, and tricuspid valves.
The sample was identified by selecting all acute hospital admissions in ordinary regimen with date of discharge between the 1st of January 2010 and the 31st of December 2018, and a principal or secondary procedure of valvuloplasty or aortic (ICD9CM code 35.11, 35.20, 35.21, 35.22, 35.33), mitral (35.12, 35.23, 35.24) or tricuspid valve replacement (35.14, 35.27, 35.28). We also included acute hospital admissions in ordinary regimen with principal or secondary procedures on the chordae tendineae (35.32) and annuloplasty (35.33), but only if a primary diagnosis of aortic valve (424.1 or 395.x), mitral valve (424.0 or 394.x), or tricuspid valve (424.2 or 397.0) diseases was present.
For the selected population, the distribution of subjects and hospitalizations was calculated by year of discharge. Distribution by sex and age of patients undergoing cardiac valve interventions was estimated, as well as intra-hospital mortality by year of discharge. Resource consumption was estimated by calculating the total number of hospitalization days and the economic value of the selected hospital admissions, assuming that in each region, hospitalizations were remunerated according to the values of the national reference rates (DM 18/10/2012). All analyses were stratified by type of valve (aortic, mitral, or tricuspid). The distribution of hospitalizations by year of discharge was also stratified by age group (18-59, 60-69, 70-79, 80+) and Charlson Comorbidity Index (CCI). CCI was estimated for each subject by considering all comorbidities identified in hospitalizations recorded before the first event of intervention related to valves.
To estimate the beneficiaries and costs related to social security benefits for individuals affected by valve diseases, all new applications submitted during the period 2016-2019, with a prevalent diagnosis of diseases and disorders of the aortic, mitral, or tricuspid valve and recognition of AA were selected. The ICD9CM codes listed previously were used to identify applications for valve diseases. Following a method described elsewhere (20), social security beneficiaries and related costs were estimated through a probabilistic model with a Monte Carlo simulation, to obtain the number of prevalent cases from the incident ones. In summary, the proportion of incident recognitions for valve diseases over the total incident recognitions for AA was calculated. This proportion was then applied to the yearly total of prevalent benefits to estimate those associated with valve diseases. It was assumed that all recipients received the social benefit throughout the entire year, as no data was available on potential benefit revocations. To address potential bias from this assumption, a Monte Carlo simulation was performed. Specifically, gamma distributions were assigned to the benefits provided and annual values, while beta distributions were applied to the percentages.
Total expenditure was determined by multiplying the number of AA beneficiaries by the annual amount granted per recipient, based on the 2018 rate (€6,180). In both analyses—direct and social security costs—nominal values were used, without adjustments for inflation.
Results
During the period 2010-2018, there was a consistent increase in hospitalizations involving cardiac valve interventions, rising from 24,174 in 2010 to 33,739 (+39.6%, Fig. 1). The rise in hospitalizations affected all valves, with the aortic valve (+53.3%) and mitral valve (+29.5%) experiencing more pronounced increases (Fig. 2).
The increase in the number of hospitalizations during the study period was higher in the elderly patients: the percent change was equal to +12.8% in patients aged 18-59, +14.4% in the age group 60-69, +32.3% in the age group 70-79 and +153.3% in patients over 79 years of age (Fig. 3). No change was observed when restricting the analysis to patients with 0 comorbidities (0.0%), while an increase was observed in patients with CCI equal to 1 (+62.2%), in those with CCI between 2 and 3 (+143.4%) and in those with an index higher than 3 (+460.4%). The same trend was confirmed by looking at the yearly distribution of hospitalizations by CCI within age groups (Fig. S1), with the highest increase observed in patients over 79 years of age and with CCI index higher than 3 (+871.9%). The number of hospitalizations by CCI and age group is reported in Table S1.
In 2018, most hospitalizations involved single interventions on the aortic valve (62.1%), followed by those on the mitral valve (25.5%), while single interventions on the tricuspid valve represented only 1.0% of the selected cases. The remaining 11.4% of hospitalizations involved interventions on two or more valves, with 50.5% of these being combined interventions on the aortic and mitral valves (Fig. S2).
Most patients undergoing intervention on the aortic or mitral valve were males (58.4% and 59.5%, respectively), while for the tricuspid valve, the proportion of females was higher (56.9%). The overall mean age of patients for the selected hospitalizations was 70 years, yet with significant differences based on the valve interest: 73 years for the aortic valve, 65 for the mitral valve, and 56 for the tricuspid valve (Fig. 4).
In 2018, hospitalizations for cardiac valve interventions were 33,739, resulting in a total of 504,312 hospitalization days and an economic value of €808 million. The average length of stay was 14.9 days (14.0 for aortic valve interventions, 14.9 for mitral valve, and 21.0 for tricuspid valve interventions). The average estimated cost per hospitalization was €23,949 (€23,817 for aortic, €23,886 for mitral, and €25,423 for tricuspid valve interventions). Over time, there was an observed increase in the average annual cost per patient (+4.3%, Table 1).
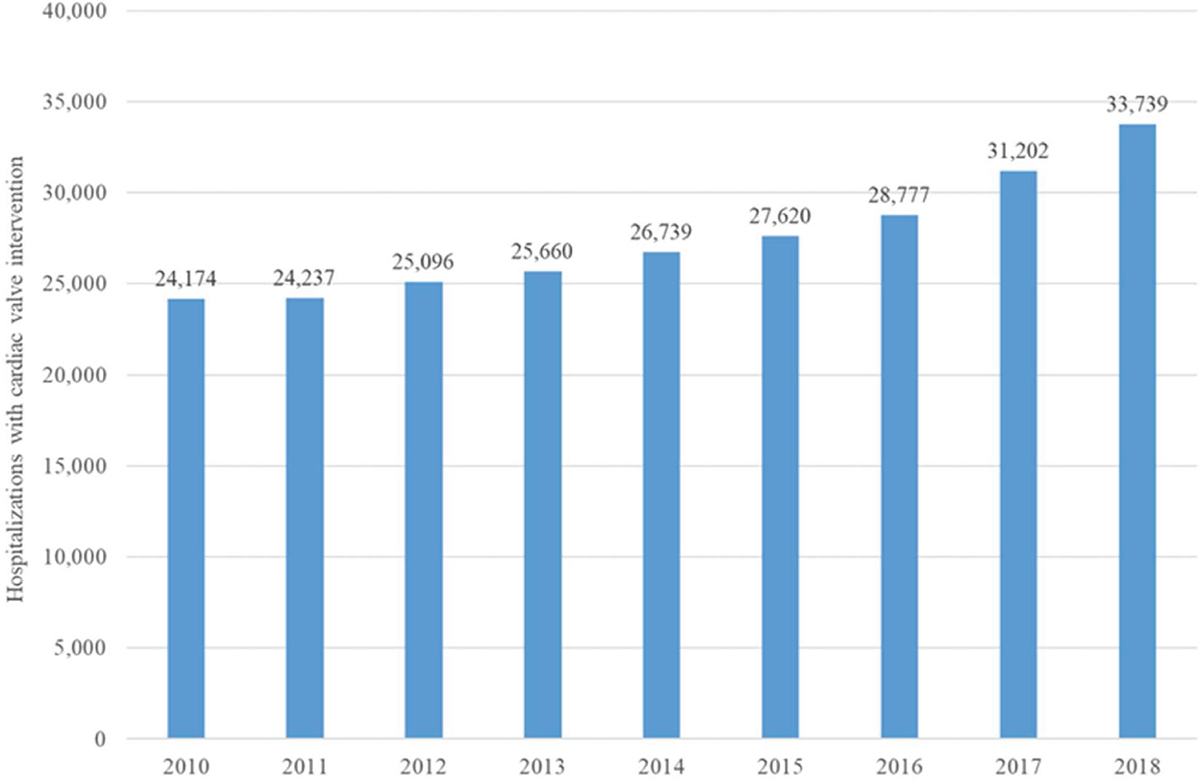
FIGURE 1 - Number of hospitalizations with cardiac valve intervention per year of discharge.
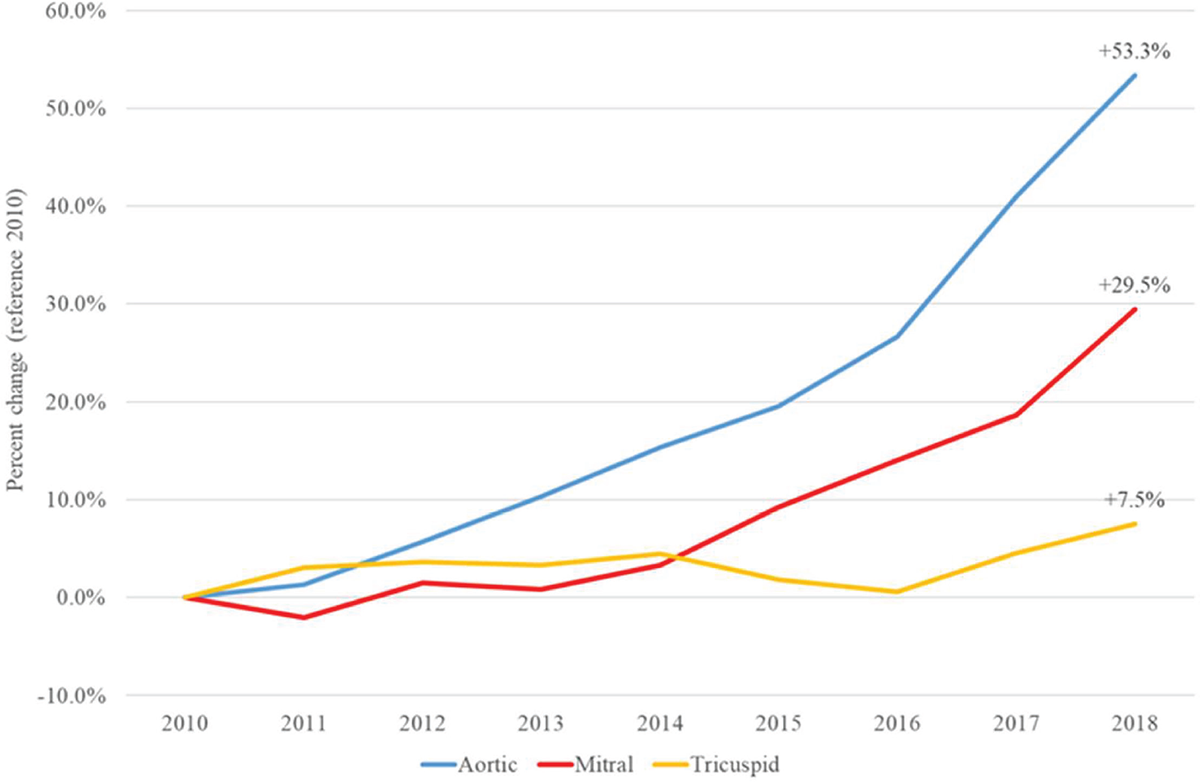
FIGURE 2 - Percentage Change (%) in the number of hospitalizations with interventions on the cardiac valves by type and year of discharge (reference year 2010).
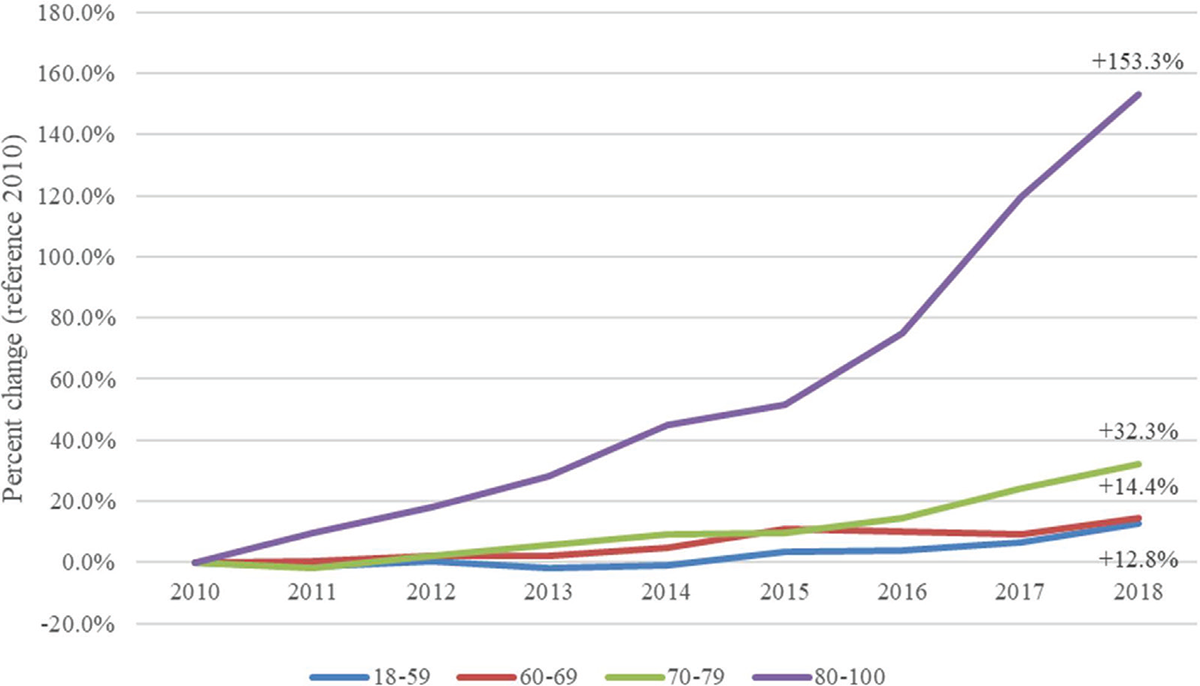
FIGURE 3 - Percent change (%) in the number of hospitalizations with interventions on the cardiac valves by age category and year of discharge (reference year 2010).
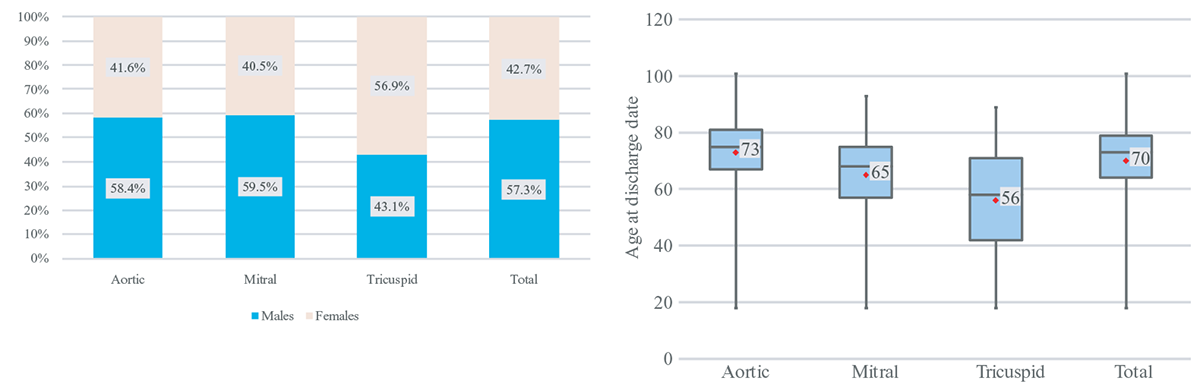
FIGURE 4 - Distribution by gender and age of patients undergoing cardiac valve interventions.
| Procedure | Mean length of stay | Mean cost |
|---|---|---|
| Aortic | 14.0 | 23,817 € |
| Mitral | 14.9 | 23,886 € |
| Tricuspid | 21.0 | 25,423 € |
| Combinations | 19.5 | 24,691 € |
| TOTAL | 14.9 | 23,949 € |
During the study period, in-hospital mortality has consistently decreased for the aortic valve (4.5% in 2010 to 3.1% in 2018) and mitral valve (5.3% in 2010 to 3.2% in 2018). The trend for tricuspid valve mortality, although decreasing, has been less regular due to the low number of cases (9.1% in 2010 to 6.4% in 2018, Fig. 5).
Between 2016 and 2019, a total of 12,406 applications for social security benefits were submitted with diagnoses of diseases or disorders of the heart valves. Requests related to the aortic valve accounted for 53.6% of the total, those for diseases or disorders of the mitral valve for 41.0%, while only 5.4% reported a diagnosis related to the tricuspid valve. There was a significant increase in the number of requests during the study period, with the greatest increment observed for the aortic valve (+39.4%), followed by the tricuspid valve (+32.7%), and the mitral valve (+25.6%, Fig. 6).
Two percent of the requests were rejected, regardless of the affected valve. While 37% of the requests related to the aortic valve resulted in partial disability recognition, for the mitral and tricuspid valves, this applied to half of the submitted requests. Consequently, a higher prevalence of total disability recognitions (25% compared to 21% for mitral and tricuspid) and recognition of total disability with AA (36% compared to 27% and 28%, respectively) was estimated for the aortic valve (Fig. 7).
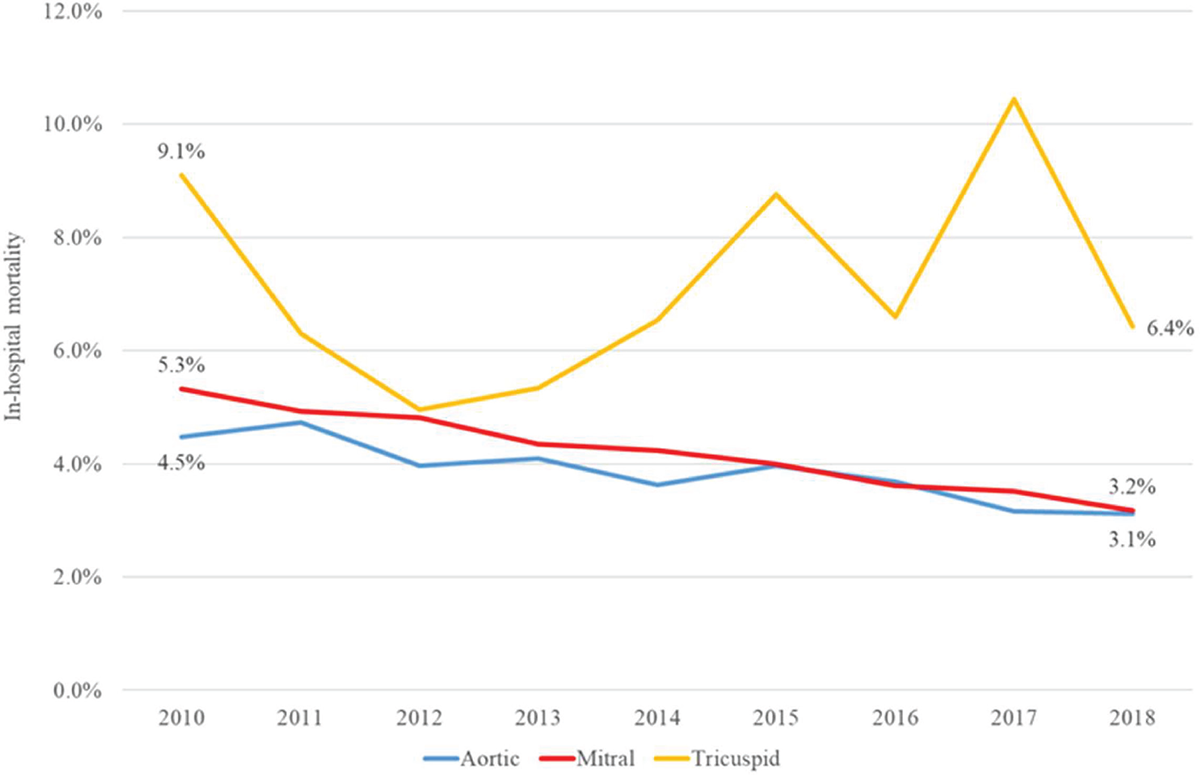
FIGURE 5 - In-hospital mortality for cardiac valve interventions.
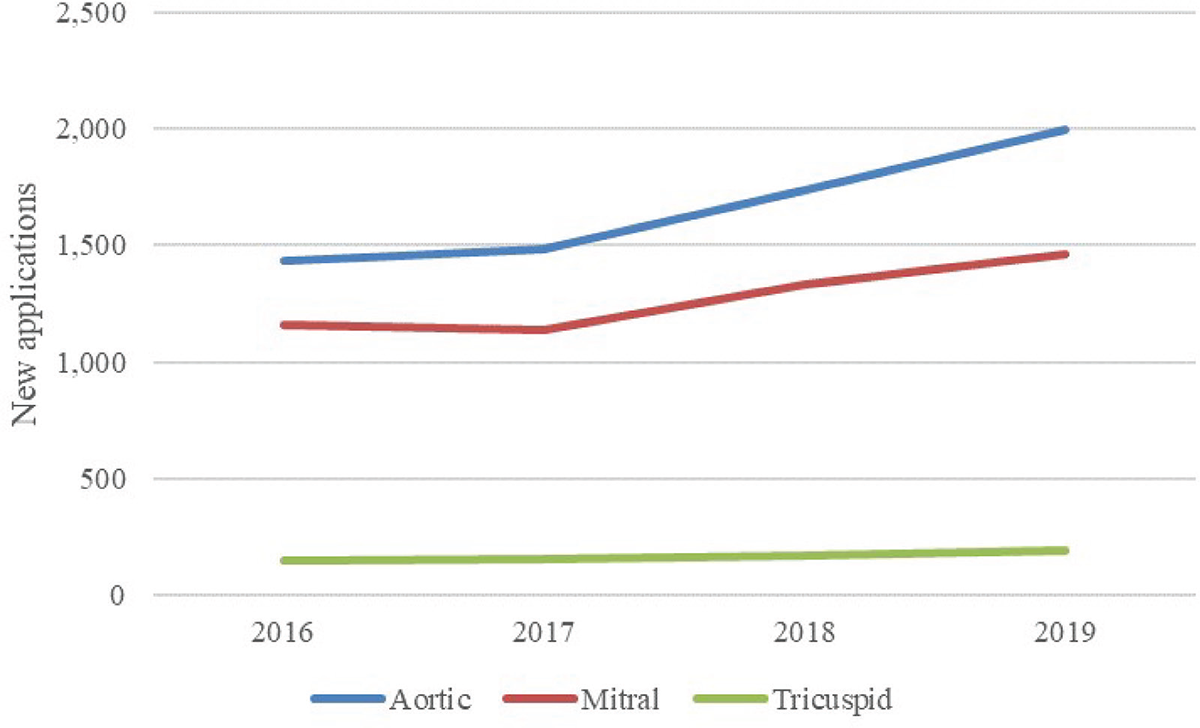
FIGURE 6 - New applications for social security benefits, by year and type.
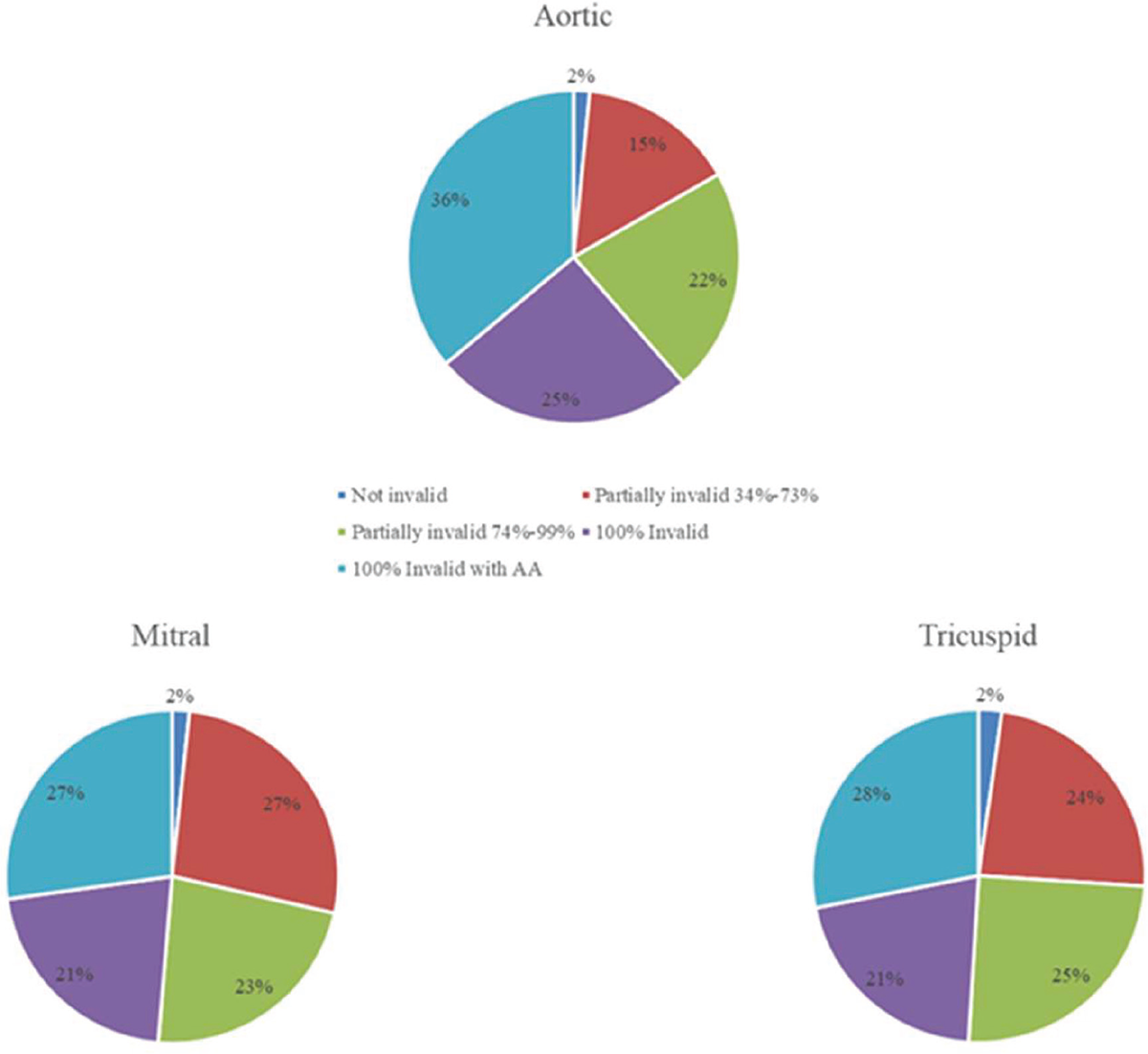
FIGURE 7 - Distribution of new applications by type and outcome.
On average, each year, 2,814 beneficiaries of social security benefits with diseases or disorders of the aortic valve were estimated, while recipients for the mitral and the tricuspid valve were 1,628 and 221, respectively. The average annual expenditure amounted to €28.9 million (Table 2).
Discussion
The aim of this study was to estimate the expenditure related to HVDs in Italy through an analysis of real-world data. This study provided a detailed overview of the prevalence and economic burden of HVDs in Italy, utilizing real data from the Italian national SDO and requests for social security benefits.
The analysis revealed a consistent increase in hospitalizations for cardiac valve interventions during the period 2010-2018, with a higher incidence of interventions on the aortic and mitral valves, with respect to the tricuspid ones. The population undergoing these interventions had an average age of around 70 years, but with significant differences depending on the involved valve. The findings of our study are consistent with several previous studies that have highlighted a significant rise in hospitalizations for cardiac valve interventions over the years. As a matter of fact, the literature confirms these findings for the aortic (21–23), the mitral (24,25), and the tricuspid valve (26,27). This could be attributed to several factors, including the ageing population, improvements in surgical techniques, increased awareness of valve pathologies, and the rising prevalence of chronic hypertension, atherosclerosis, and other cardiovascular conditions (28). Furthermore, the increase in the number of hospitalizations for aortic valve interventions may reflect a rise in the incidence of aortic valve pathologies, such as aortic stenosis or aortic insufficiency, necessitating surgical intervention (29). The analysis revealed a greater increase in hospitalizations between 2010 and 2018 as both patient age and CCI increased. This is likely due to the growing use of the transcatheter approach over the years, which is recommended for older and/or frail patients for whom surgery is unsuitable (30,31).
| Mean annual beneficiaries | Mean annual cost | |
|---|---|---|
| Aortic valve | 2,814 | €17,412,487 |
| Mitral valve | 1,628 | €10,074,088 |
| Tricuspid valve | 221 | €1,365,081 |
| Total | 4,663 | €28,851,655 |
The distribution of hospitalizations by type of intervention highlights a predominance of single interventions on the aortic valve, followed by interventions on the mitral valve. This could be attributed to different valve pathologies and their respective indications for surgical intervention (28). However, it is important to consider that the distribution may vary based on the demographic characteristics and clinical practices of different contexts.
The analysis of in-hospital mortality showed a consistent decrease over the years for interventions on the aortic and mitral valves. This finding is also supported by literature: a single-center study conducted on a cohort of patients in England for SAVR estimated a decreasing in-hospital mortality from 2.9% in 2000-2005 to 0.7% in 2012-2017 (32). A meta-analysis conducted on subjects undergoing TAVI estimated a 30-day mortality of 10.5% in 2007 and 2.3% in 2016 (33). A similar trend, although with a less pronounced reduction (more similar to the estimates obtained in this study), is observed for the mitral valve (25). The evidence is more uncertain regarding the tricuspid valve: one study reported a consistent trend over time in in-hospital mortality in patients with tricuspid valve diseases (34), while another article that analyzed mortality related to tricuspid valve regurgitation estimates a strongly positive trend during the period 2013-2018 (35). In general, these results suggest improvements in perioperative management, surgical techniques, and postoperative intensive care (36). However, mortality rates still remain significant, highlighting the complexity of these procedures and the need for careful monitoring of the quality of care and long-term follow-up for patients undergoing intervention.
The overall expenditure related to HVDs was significant, with an economic value of €808 million in 2018 for hospitalizations alone. The average cost per hospitalization was estimated to be €23,949, with higher expenditure (and average length of stay) for hospitalizations related to the tricuspid valve compared to the overall average. The estimated cost related to valve interventions was slightly lower compared to that reported in a similar study (16). A study conducted using real-world data in Spain reported results similar to ours, with a hospitalization cost for SAVR of €26,684 and for TAVI of €14,940 (37). As for the mitral valve, a study on a cohort of patients in the United Kingdom undergoing intervention reported an average cost of around £16,000 (38). Studies on the direct costs of tricuspid valve intervention were conducted in the United States and reported non-comparable costs due to the different functioning of healthcare systems (39,40). These data confirmed the considerable economic burden of HVDs on the Italian healthcare system, emphasizing the importance of timely and effective interventions to reduce the costs associated with hospitalizations.
The analysis of requests for social security benefits revealed a significant increase in applications for HVDs and disorders. In particular, requests related to the aortic valve showed a more pronounced increase, followed by those concerning the tricuspid and mitral valves. This result contradicts the findings of the 2019 Global Burden of Disease, which estimates a negative temporal trend for cardiovascular diseases in terms of Disability Adjusted Life Years (DALYs) (41).
The estimate of social security benefits costs revealed an annual expenditure of €28.9 million. In our analysis, these costs constitute a minor fraction of the overall economic burden, which is primarily driven by hospital admissions. This expense category only partially represents the total indirect costs related to overall cardiovascular diseases, which could explain the cost trend going against expectations (19).
Although this study, to the best of our knowledge, is among the first to provide a comprehensive description of the epidemiology and economic burden of HVDs in Italy, using real-world data, some limitations must be acknowledged. First, the use of SDO limits the scope of the study to hospital-based interventions, excluding non-surgical treatments and outpatient care. Consequently, the study may underestimate the overall number of patients affected by HVDs, particularly those managed conservatively or with comorbidities that preclude surgical interventions. Additionally, the social security data used in this study is limited to applications for disability and attendance allowances. This approach may underrepresent the indirect costs borne by patients and their families, such as productivity losses for family members providing care or out-of-pocket expenses for medications, specialist visits, and home-based rehabilitation. Third, our study didn’t take into account potential regional disparities in the treatment of valve diseases. The decentralized structure of Italy’s healthcare system often results in regional differences in the management and treatment of diseases. These differences can stem from variations in economic resources, healthcare infrastructure, and the availability of specialized centers. Regional disparities can influence both access to care and patient outcomes, potentially creating inequities across the country (30). Factors such as procedural volumes, availability of trained specialists, and organizational efficiency of healthcare services contribute to these variations. Higher-volume centers are often associated with better outcomes, highlighting the importance of ensuring equitable access to specialized care across all regions (42). Finally, this study focuses exclusively on the epidemiological figures and associated costs of clinical cases where an intervention has been performed. As such, the costs related to patients managed conservatively with medical therapy are not included in the analysis. This limitation may lead to an underestimation of the overall economic burden of HVDs, as it excludes a potentially significant subset of patients who do not undergo surgical or transcatheter interventions.
The findings of this study underscore the significant economic burden associated with HVD and highlight the need for targeted policy actions. The PREVASC study, a large-scale registry focused on asymptomatic individuals of age 65+, revealed the substantial prevalence of undiagnosed and underreported valvular heart diseases, particularly in aging populations (43). The analysis revealed that 3 out of 4 patients, despite not having a history of HVDs, presented at least one valve defect. This percentage increased to 87% in patients over 75. Early detection initiatives, such as systematic screening programs for high-risk groups (e.g., individuals over 65 years of age), should be prioritized, including systematic auscultation and routine echocardiograms. These programs could be complemented by raising awareness among non-specialist physicians, to address gaps in detection and diagnosis. Additionally, structured pathways for timely interventions and multidisciplinary follow-up care should be established to optimize outcomes and reduce mortality. Public health efforts should include campaigns to enhance patient engagement and empowerment, ensuring adherence to treatment plans and promoting preventive measures.
Conclusions
This study highlights the growing impact of HVDs on public health and the Italian healthcare system. HVDs pose a clinically and socioeconomically relevant issue, and the management of these conditions requires a multidisciplinary and personalized approach. Further efforts should be dedicated to the prevention, early diagnosis, and treatment of HVDs to reduce the healthcare burden and improve the quality of life for patients.
Disclosures
Conflicts of interest: The authors have no relevant financial or non-financial interests to disclose.
Funding: The study was funded by Edwards Lifesciences. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author contributions: All authors contributed to the study’s conception. PS and FSM developed the study design, PS and MS conducted the statistical analysis and derived the analytical results. The first draft of the manuscript was written by PS and MS. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1. Istituto Superiore di Sanità. Valvulopatie. Online (Accessed August 2024)
- 2. Ministero della Salute. Malattie Delle Valvole Cardiache. Online (Accessed August 2024)
- 3. Azraai M, Gao L, Ajani AE. Cost-Effectiveness of Transcatheter Aortic Valve Intervention (TAVI) Compared to Surgical Aortic Valve Replacement (SAVR) in Low- to Intermediate-Surgical-Risk Patients. Cardiovasc Revasc Med. 2020 Sep;21(9):1164-1168. CrossRef PubMed
- 4. Doyle MP, Woldendorp K, Ng M, Vallely MP, Wilson MK, Yan TD, Bannon PG. Minimally-invasive versus transcatheter aortic valve implantation: systematic review with meta-analysis of propensity-matched studies. J Thorac Dis. 2021 Mar;13(3):1671-1683. CrossRef PubMed
- 5. Iung B, Vahanian A. Epidemiology of acquired valvular heart disease. Can J Cardiol. 2014 Sep;30(9):962-970. CrossRef PubMed
- 6. Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J Am Coll Cardiol. 2019 Nov 19;74(20):2529-2532. CrossRef PubMed
- 7. Roth GA, Mensah GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risks: A Compass for Global Action. J Am Coll Cardiol. 2020 Dec 22;76(25):2980-2981. CrossRef PubMed
- 8. d’Arcy JL, Coffey S, Loudon MA, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J. 2016;37(47):3515-3522. CrossRef PubMed
- 9. Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999;83(6):897-902. CrossRef PubMed
- 10. Prihadi EA, van der Bijl P, Gursoy E, et al. Development of significant tricuspid regurgitation over time and prognostic implications: new insights into natural history. Eur Heart J. 2018;39(39):3574-3581. CrossRef PubMed
- 11. Corriere della Sera. Corriere Salute. Screening per il cuore, la diagnosi precoce potrebbe salvare la vita a 150mila persone l’anno. Online (Accessed August 2024)
- 12. Moore M, Chen J, Mallow PJ, Rizzo JA. The direct health-care burden of valvular heart disease: evidence from US national survey data. Clinicoecon Outcomes Res. 2016;8:613-627. CrossRef PubMed
- 13. Trochu JN, Le Tourneau T, Obadia JF, Caranhac G, Beresniak A. Economic burden of functional and organic mitral valve regurgitation. Arch Cardiovasc Dis. 2015;108(2):88-96. CrossRef PubMed
- 14. Galper BZ, Chinnakondepalli KM, Wang K, et al; PARTNER Investigators. Economic Outcomes of Transcatheter Versus Surgical Aortic Valve Replacement in Patients with Severe Aortic Stenosis and Low Surgical Risk: results from the PARTNER 3 Trial. Circulation. 2023;147(21):1594-1605. CrossRef PubMed
- 15. Cork DP, McCullough PA, Mehta HS, et al. The economic impact of clinically significant tricuspid regurgitation in a large, administrative claims database. J Med Econ. 2020;23(5):521-528. CrossRef PubMed
- 16. Berti E, Fortuna D, Bartoli S, et al. [Transcatheter aortic valve implantation versus aortic valve replacement: cost analysis from the regional health service and hospital perspectives]. G Ital Cardiol (Rome). 2016;17(12)(suppl 1):22S-30. PubMed
- 17. Santarpino G, Lorusso R, Moscarelli M, et al. Sutureless versus transcatheter aortic valve replacement: A multicenter analysis of “real-world” data. J Cardiol. 2022;79(1):121-126. CrossRef PubMed
- 18. Kotseva K, Gerlier L, Sidelnikov E, et al. Patient and caregiver productivity loss and indirect costs associated with cardiovascular events in Europe. Eur J Prev Cardiol. 2019;26(11):1150-1157. CrossRef PubMed
- 19. Cebr. The Economic Cost of Cardiovascular Disease from 2014-2020 in Six European Economies. Online (Accessed August 2024)
- 20. Russo S, Mariani TT, Migliorini R, Marcellusi A, Mennini FS. The economic burden of musculoskeletal disorders on the Italian social security pension system estimated by a Monte Carlo simulation. Reumatismo. 2015;67(2):45-56. CrossRef PubMed
- 21. Mauri V, Abdel-Wahab M, Bleiziffer S, et al. Temporal trends of TAVI treatment characteristics in high volume centers in Germany 2013-2020. Clin Res Cardiol. 2022;111(8):881-888. CrossRef PubMed
- 22. Stortecky S, Franzone A, Heg D, et al. Temporal trends in adoption and outcomes of transcatheter aortic valve implantation: a SwissTAVI Registry analysis. Eur Heart J Qual Care Clin Outcomes. 2019;5(3):242-251. CrossRef PubMed
- 23. Auffret V, Lefevre T, Van Belle E, et al; FRANCE TAVI Investigators. Temporal Trends in Transcatheter Aortic Valve Replacement in France: FRANCE 2 to FRANCE TAVI. J Am Coll Cardiol. 2017;70(1):42-55. CrossRef PubMed
- 24. Paparella D, Fattouch K, Moscarelli M, et al. Current trends in mitral valve surgery: A multicenter national comparison between full-sternotomy and minimally-invasive approach. Int J Cardiol. 2020;306:147-151. CrossRef PubMed
- 25. Elbadawi A, Elgendy IY, Mohamed AH, et al. Temporal Trends and Outcomes of Transcatheter Mitral Valve Repair and Surgical Mitral Valve Intervention. Cardiovasc Revasc Med. 2020 Dec;21(12):1560-1566. CrossRef PubMed
- 26. Zack CJ, Fender EA, Chandrashekar P, et al. National Trends and Outcomes in Isolated Tricuspid Valve Surgery. J Am Coll Cardiol. 2017;70(24):2953-2960. CrossRef PubMed
- 27. Torres C, Lozier MR, Davidson CJ, et al. In-Hospital Outcomes of Transcatheter Tricuspid Valve Repair: An Analysis From the National Inpatient Sample. J Soc Cardiovasc Angiogr Interv. 2022;1(5):100414. CrossRef PubMed
- 28. Aluru JS, Barsouk A, Saginala K, Rawla P, Barsouk A. Valvular Heart Disease Epidemiology. Med Sci (Basel). 2022 Jun 15;10(2):32. CrossRef PubMed
- 29. Ambrosy AP, Go AS, Leong TK, et al. Temporal trends in the prevalence and severity of aortic stenosis within a contemporary and diverse community-based cohort. Int J Cardiol. 2023;384:107-111. CrossRef PubMed
- 30. Masiero G, Musumeci G. Transcatheter aortic valve implantation in Italy: an uneven growth. Eur Heart J Suppl. 2020;22(suppl E):E96-E100. CrossRef PubMed
- 31. Tarantini G, et al. [Updated SICI-GISE position paper on institutional and operator requirements for transcatheter aortic valve implantation]. G Ital Cardiol (Rome). 2018;19:519-529 CrossRef PubMed
- 32. Dimagli A, Sinha S, Caputo M, Angelini GD, Benedetto U. Trend in morbidity and mortality in surgical aortic valve replacement: a retrospective, observational, single-centre study. Interact Cardiovasc Thorac Surg. 2020;31(6):796-802. CrossRef PubMed
- 33. Mattke S, Schneider S, Orr P, Lakdawalla D, Goldman D. Temporal Trends in Mortality after Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Regression Analysis. Struct Heart. 2020;4(1):16-23. CrossRef
- 34. Kolte D, Kennedy KF, Passeri JJ, Inglessis I, Elmariah S. Temporal Trends in Prevalence of Tricuspid Valve Disease in Hospitalized Patients in the United States. Am J Cardiol. 2020;125(12):1879-1883. CrossRef PubMed
- 35. Shariff M, Kumar A, Hirji SA, Majmundar M, Adalja D, Doshi R. Ten Years Mortality Trends of Tricuspid Regurgitation in the United States, 2008 to 2018. Am J Cardiol. 2021 Feb 1;140:156-157. CrossRef PubMed
- 36. Tan MC, Yeo YH, San BJ, et al. Trends and Disparities in Valvular Heart Disease Mortality in the United States From 1999 to 2020. J Am Heart Assoc. 2024;13(8):e030895. CrossRef PubMed
- 37. Areces S, Hernández-Vaquero D, Avanzas P, García-Aranda FJ, Silva J, Morís C. Cost comparison between transcatheter aortic valve implantation and surgical valve replacement using individual data in a Spanish public hospital. Cir Cardiovasc. 2021;28(6):317-324. CrossRef
- 38. Perin G, Shaw M, Toolan C, Palmer K, Al-Rawi O, Modi P. Cost Analysis of Minimally Invasive Mitral Valve Surgery in the UK National Health Service. Ann Thorac Surg. 2021;112(1):124-131. CrossRef PubMed
- 39. Alperi A, Almendárez M, Álvarez R, Moris C, Leon V, Silva I, Hernández-Vaquero D, Pascual I, Avanzas P. Transcatheter tricuspid valve interventions: Current status and future perspectives. Front Cardiovasc Med. 2022 Sep 14;9:994502. CrossRef PubMed
- 40. Alqahtani F, Berzingi CO, Aljohani S, Hijazi M, Al-Hallak A, Alkhouli M. Contemporary Trends in the Use and Outcomes of Surgical Treatment of Tricuspid Regurgitation. J Am Heart Assoc. 2017;6(12):e007597. CrossRef PubMed
- 41. Masaebi F, Salehi M, Kazemi M, Vahabi N, Azizmohammad Looha M, Zayeri F. Trend analysis of disability adjusted life years due to cardiovascular diseases: results from the global burden of disease study 2019. BMC Public Health. 2021;21(1):1268. CrossRef PubMed
- 42. Agenas. Programma Nazionale Esiti. Edizione 2023. Online (Accessed August 2024)
- 43. Amico MA, Busi G, Vannini M, et al. PREVASC: prospective registry of epidemiology of valve disease in asymptomatic italian subjects [Internet]. 2024. Online (Accessed August 2024)