 |
Glob Reg Health Technol Assess 2024; 11: 258-264 ISSN 2283-5733 | DOI: 10.33393/grhta.2024.3186 ORIGINAL RESEARCH ARTICLE |
 |
The economic burden of post-endoscopic retrograde cholangiopancreatography (ERCP) procedure infections in Italy
ABSTRACT
Introduction: The infections of multidrug-resistant organisms (MDROs) associated with duodenoscopes during endoscopic retrograde cholangiopancreatography (ERCP) procedure have become a significant cause for concern, especially in fragile patients. While the clinical impacts of these infections are well-documented, their economic implications remain underexplored. This study assesses the incidence and economic burden of post-ERCP infections in Italy using an administrative database.
Methods: We conducted a retrospective observational study using administrative databases from A.O.U. Città della Salute e della Scienza di Torino. The study included all patients who underwent their first inpatient ERCP between 2018 and 2021. Infections were identified using ICD-9-CM codes for Pseudomonas aeruginosa, Clostridium difficile, Escherichia coli, Klebsiella spp., and Staphylococcus aureus. A 1-year follow-up was defined in order to estimate healthcare resource utilization and related costs, including readmissions, drug prescriptions, and outpatient specialist and laboratory services.
Results: The study included 686 inpatient ERCP cases, an overall infection rate of 4.2% was observed. Higher infection rates were observed in women (4.6%), patients over 70 years old (4.6%), emergency admissions (5.1%), and transplant patients (19.1%). The average hospital stay doubled for infected patients (24.3 vs. 11.3 days; p=0.001). Post-ERCP infections led to a 28% increase in average costs (€12,256 vs. €9,561; p=0.048). With an annual volume of 25,000 ERCP procedures, post-ERCP infections in Italy contribute approximately €2.9 million in additional direct costs per year.
Conclusion: Post-ERCP infections impose substantial financial burdens on the healthcare system, underscoring the critical importance of implementing cost-effective prevention strategies to mitigate this public health threat in Italy.
Keywords: Economic burden, Endoscopic retrograde cholangiopancreatography, Healthcare resource utilization, Multidrug resistant, Post-ERCP infections, Real-world data
Received: June 29, 2024
Accepted: November 12, 2024
Published online: December 31, 2024
Global & Regional Health Technology Assessment - ISSN 2283-5733 - www.aboutscience.eu/grhta
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
The endoscopic retrograde cholangiopancreatography (ERCP) is a sophisticated endoscopic procedure and, as such, is burdened by potential complications. These complications are related to risk factors associated with the type of procedure or patient characteristics (age, gender, history of previous pancreatitis, coagulation abnormalities, concurrent illnesses, etc.). Major adverse events reported in the literature include acute pancreatitis (3.5%, ranging from 1.6% to 15.7%), bleeding (1.3%, ranging from 1.2% to 1.5%), perforation (0.1% to 0.6%), and infections such as cholangitis (1%-2%) and cholecystitis (0.2%-0.5%) (1,2).
Endogenously transmitted infections related to endoscopic procedures are the most common infections involving the patient’s intestinal flora. Simultaneously, exogenous transmission of microorganisms to patients undergoing ERCP is correlated with the prevalence of duodenoscope contamination (3). While exogenous infections can theoretically be prevented through effective reprocessing (4,5), a growing number of infection outbreaks associated with duodenoscopes have been reported in various healthcare systems (6-10).
Several studies have investigated the risk factors for the occurrence of infections following ERCP and the associated outcomes (11-15). Significant risk factors for the transmission of pathogens include non-compliance with disinfection guidelines, the promotion of biofilm deposition due to complex design and surface defects, and automated endoscope reprocessing. Indeed, a recent meta-analysis highlights that contaminations of reprocessed patient-ready duodenoscopes account for 15.25% (16). The precise risk of a patient contracting an infection from a contaminated endoscope remains uncertain; however, previous duodenoscope-associated outbreaks have shown attack rates ranging from 12% to 41% (17).
In the literature, Pseudomonas aeruginosa, along with carbapenem-resistant Enterobacteriaceae (CRE), has been increasingly recognized as the leading cause of infections associated with contaminated duodenoscopes (18-21).
Contaminated duodenoscopes have been reported also in Italy (22). In a recent Italian survey, 36 (69.2%) centers reported at least one episode of duodenoscope-related infection experienced with a variable number of patients per center contaminated during ERCP (23). However, to our knowledge, there are no studies aimed at estimating the economic burden of ERCP and the associated infections in Italy. Thus, this study aimed to fill the gap by assessing the incidence of post-ERCP infections and evaluating their economic burden.
Methods
Data sources
The study was based on data obtained from the administrative databases of the A.O.U. Città della Salute e della Scienza Di Torino. Specifically, the following datasets were made available for the period from January 1, 2018, to June 30, 2022:
- Hospital Discharge Record (HDR), which records all hospitalizations and includes patient demographic and clinical information. Diagnoses and procedures performed during the hospital stay are classified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) system. HDR also includes Diagnosis-Related Group (DRG) information and related charges provided by the Italian National Health System (INHS).
- Outpatient Specialist Services, which records all outpatient specialist healthcare services, including specialist visits and procedures performed on an outpatient setting, maternal and child health clinic activities, instrumental, diagnostic, and laboratory diagnostic services.
- Pharmaceutical database, which records pharmaceutical services dispensed directly by the Institution’s hospital pharmacy. It collects Anatomical-Therapeutic Chemical (ATC) code, marketing authorization code, number of packages, number of units per package, unit cost per package, and prescription date.
The use of a unique patient identifier code across all databases facilitated electronic linkage between these diverse datasets. To ensure patient privacy and comply with the European General Data Protection Regulation (GDPR) (2016/679), each subject included in the study was assigned an anonymous and unique numeric code. No personally identifiable information related to patients was accessible to the authors.
The study has been notified to and approved by Comitato Etico interaziendale, A.O.U. Città della Salute e della Scienza di Torino – A.O. Ordine Mauriziano di Torino – A.S.L. Città di Torino.
Study design and cohort
This retrospective observational study examines the healthcare costs of patients undergoing ERCP from the perspective of the healthcare system. The eligible population consisted of adult patients who underwent inpatient ERCP procedures with non-disposable duodenoscope. To identify the study population, all acute admissions in ordinary regimen with a discharge date between January 1, 2018, and June 30, 2021, and a primary or secondary procedure of ERCP (ICD-9-CM 51.10) were selected. In cases where a patient had multiple admissions with ERCP procedures during the enrolment period, the first admission in chronological order was selected as the index event.
The selected hospitalizations were stratified based on the presence of infections related to the ERCP procedure. Specifically, the presence of ICD-9-CM codes, listed in the appendix, related to infections caused by Pseudomonas aeruginosa, Clostridium difficile, Escherichia coli, Klebsiella spp., and Staphylococcus aureus was evaluated in either the primary or secondary diagnosis.
The enrolled patients were followed for a period of 1 year, with the end of the follow-up period set at June 30, 2022. During this time, healthcare resource utilization (HCRU) including readmissions, medication use, and outpatient specialist and laboratory services was estimated.
Specifically, during the follow-up period, all readmissions for reintervention and/or conditions related to the study pathology (see appendix), dispensation of antibiotic and/or anticoagulant medications, and all specialist services related to clinical chemistry laboratory, microbiology and virology, general surgery, gastroenterology, general medicine, and day hospital/day service were selected.
Hospitalizations were valued based on the regional tariffs for hospital services in the Piedmont region, the cost of medications was determined using the regional reimbursement price, and the value of outpatient specialist and laboratory services was calculated using the regional tariffs in effect in the year of service provision.
For each patient, the annual expenditure, including the index hospitalization, readmissions, medication use, and outpatient specialist and laboratory services, was calculated.
The proportions of post-ERCP infections and per-patient expenditure observed in the study population were used to estimate the economic burden of infections and the corresponding 95% confidence interval at the national level. National ERCP procedure volumes were derived from the “Annual Report on Hospital Activity – year 2019” published by the Ministry of Health (24).
To account for the uncertainty in assuming that the proportion of post-ERCP infections observed in the study sample was representative at the national level, the random error of this proportion was estimated. Subsequently, a bootstrap procedure with 1,000 simulations was applied to calculate the 95% confidence interval for the number of post-ERCP infections at the national level. Additionally, to make the economic estimates more generalizable, the economic burden of post-ERCP infections was estimated using national reimbursement tariffs for hospital and outpatient specialist services, and ex-factory prices net of mandatory discounts for medications.
Statistical analysis
Descriptive analyses were undertaken, summarizing categorical data using numbers and percentages, and continuous data as mean and standard deviation (SD). The crude association between outcomes and study groups was assessed using χ2 tests for categorical variables, Student’s t-tests for normally distributed data, and Mann-Whitney tests for non-normally distributed data.
All analyses were performed using SAS statistical package, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 853 patients who underwent an ERCP procedure between January 1, 2018, and June 30, 2021, were selected for the study. Among these, 686 (80.4%) were on an inpatient ordinary regimen (66.3% emergency and 33.7% elective admissions), while 167 (19.6%) were treated in day hospital and, as per the protocol, were excluded from the analysis (Fig. 1).
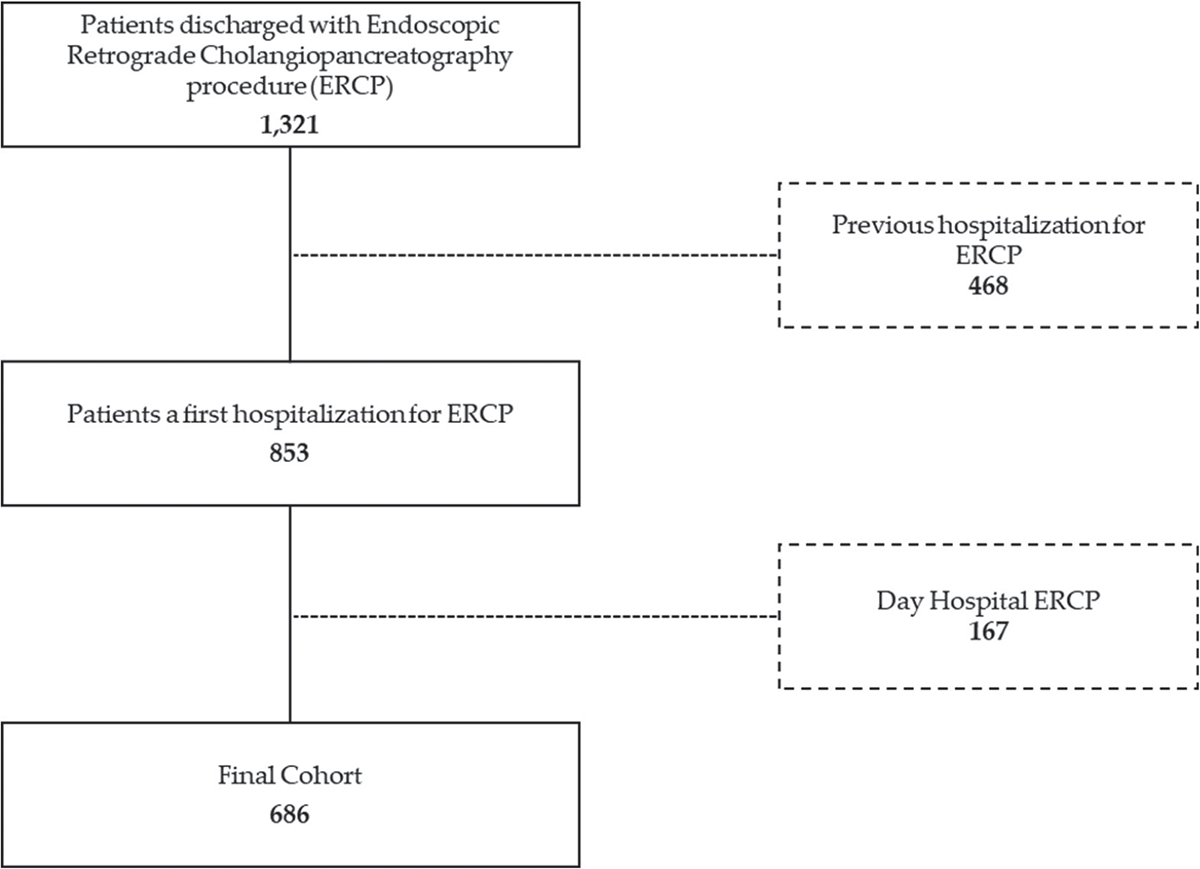
FIGURE 1 - Flowchart of study cohort selection. ERCP = endoscopic retrograde cholangiopancreatography.
Of the 686 patients included in the study, 55.4% were male, and the average age was 68.8 years, with a range from 20 to 98 years. Additionally, 9.5% of the patients had acute pancreatitis, 22.0% had or had previously been diagnosed with malignant tumors, 5.7% were undergoing chemotherapy or radiotherapy treatment, and 3.8% consisted of transplant patients (Tab. 1).
| Characteristics | N | % |
|---|---|---|
| Sex | ||
| Male | 380 | 55.4 |
| Female | 306 | 44.6 |
| Age group | ||
| 18-59 | 165 | 24.1 |
| 60-69 | 133 | 19.4 |
| 70-79 | 217 | 31.6 |
| 80+ | 171 | 24.9 |
| Type of admission | ||
| Elective | 231 | 33.7 |
| Emergency | 455 | 66.3 |
| Acute pancreatitis | ||
| No | 621 | 90.5 |
| Yes | 65 | 9.5 |
| Frailty | ||
| None | 470 | 68.5 |
| Solid organ transplant | 26 | 3.8 |
| Chemo/radiotherapy | 39 | 5.7 |
| Cancer | 151 | 22.0 |
| TOTAL | 686 | 100.0 |
Infections related to the ERCP were reported in 4.2% of procedures. A higher proportion was reported for women (4.6% vs. 3.9%), for older patients, although a linear trend was not observed (4.6% for those over 70 years old and 3.6% for under 70), for emergency admissions (5.1% vs. 2.6%), for admissions where there was no diagnosis of acute pancreatitis (4.5% vs. 1.5%), and for transplant patients (19.1%) (Tab. 2).
| Characteristics | No infection N (%) |
Infection after ERCP N (%) |
p Value |
|---|---|---|---|
| Sex | |||
| Male | 365
(96.1) |
15
(3.9) |
0.685 |
| Female | 292
(95.4) |
14
(4.6) |
|
| Age group | |||
| 18-59 | 161
(97.6) |
4
(2.4) |
0.387 |
| 60-69 | 126
(94.7) |
7
(5.3) |
|
| 70-79 | 209
(96.3) |
8
(3.7) |
|
| 80+ | 161
(94.2) |
10
(5.8) |
|
| Type of admission | |||
| Elective | 225
(97.4) |
6
(2.6) |
0.130 |
| Emergency | 432
(94.9) |
23
(5.1) |
|
| Acute pancreatitis | |||
| No | 593
(95.5) |
28
(4.5) |
0.510 |
| Yes | 64
(98.5) |
1
(1.5) |
|
| Frailty | |||
| None | 448
(95.3) |
22
(4.7) |
0.000 |
| Solid organ transplant | 21
(80.8) |
5
(19.2) |
|
| Chemo/radiotherapy | 37
(94.9) |
2
(5.1) |
|
| Cancer | 151
(100.0) |
0
(0.0) |
|
| TOTAL | 657 (95.8) |
29 (4.2) |
|
ERCP = endoscopic retrograde cholangiopancreatography.
The average length of hospital stay (LoS) for patients undergoing ERCP procedures was 11.9 days and doubles in the presence of infection (24.3 vs. 11.3; Mann-Whitney test p-value 0.001). Moreover, for patients with post-ERCP infection, there was a higher proportion of readmissions within one year (63.0% vs. 59.1%, chi-square test p-value 0.693) and a greater prescription of antibiotics and/or anticoagulants (44.4% vs. 29.8%, chi-square test p-value 0.106), although not statistically significant. The proportions of patients receiving at least one outpatient specialist service were similar (51.9% vs. 53.8%, chi-square test p-value 0.844) (Tab. 3).
| Post-ERCP infection | |||
|---|---|---|---|
| HCRU | No | Yes | p Value |
| N | 657 | 29 | – |
| LoS index event | 11.3 | 24.3 | <0.0001 |
| Discharged alive (N) | 634 | 27 | 0.286 |
| Readmitted within 1 year (%) | 59.1 | 63.0 | 0.693 |
| Patients with at least one antibiotics a/o anticoagulant dispensation (%) | 29.8 | 44.4 | 0.106 |
| Patients with at least one specialistic service (%) | 53.8 | 51.9 | 0.844 |
ERCP = endoscopic retrograde cholangiopancreatography; HCRU = healthcare resource utilization; LoS = length of hospital stay.
The average expenditure per patient, including the index hospitalization and the HCRU during the follow-up year, was significantly higher for patients with post-ERCP infection: €12,256 compared to €9,561 (Mann-Whitney test p-value 0.048). In detail, the most significant difference was related to the index hospitalization costs (€8,546 vs. €5,487; Mann-Whitney test p-value 0.000). Even the expenditure for specialized services during the follow-up, which primarily included blood chemistry and microbiological tests, liver and kidney function tests, specialized outpatient visits, and imaging services, was higher in the case of infection (€307 vs. €256), although the differences were not statistically significant (Mann-Whitney test p-value 0.681). On the other hand, despite a higher readmission rate for infected patients, the average expenditure per readmission was lower (€3,395 vs. €3,804; Mann-Whitney test p-value 0.331), while pharmaceutical expenses were negligible for all patients (€14 vs. €9) (Figure 2).
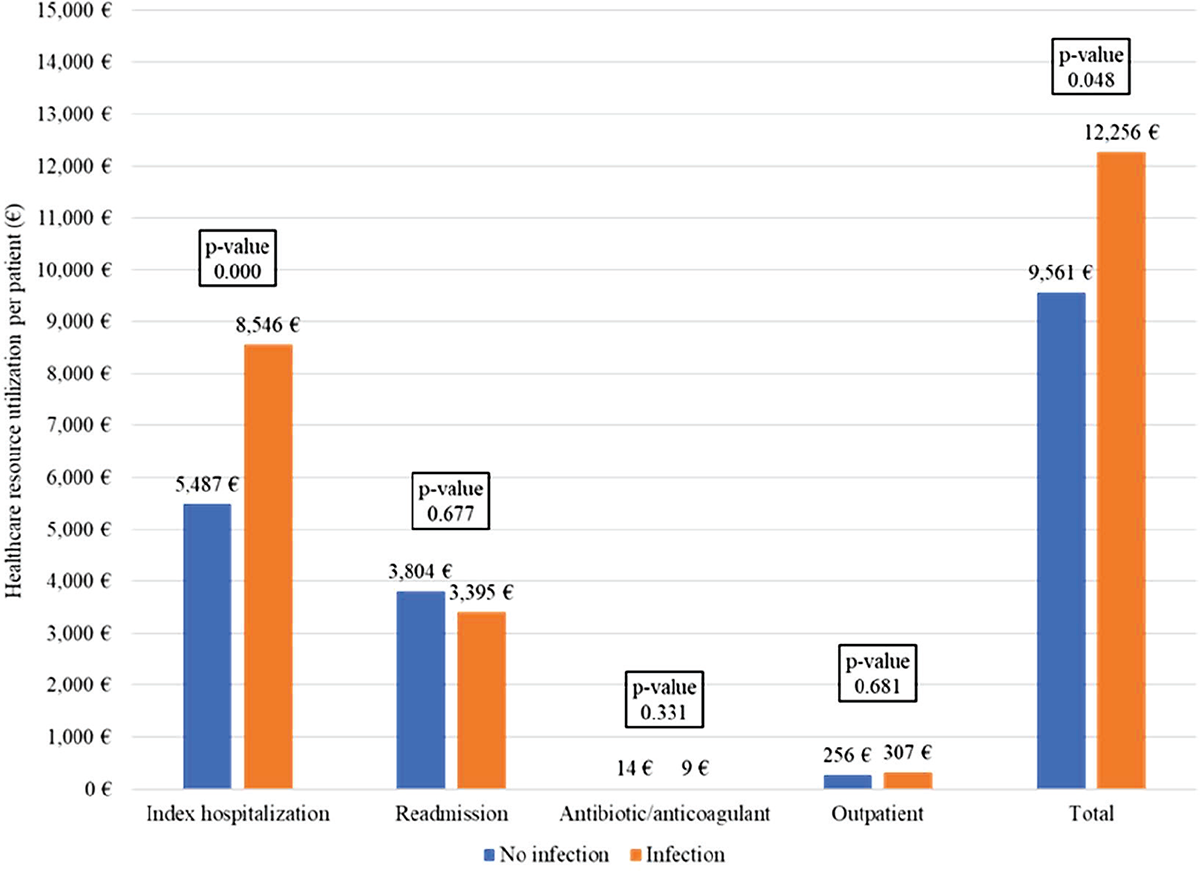
FIGURE 2 - One-year healthcare cost per patient by post-ERCP infection. ERCP = endoscopic retrograde cholangiopancreatography.
Based on the estimates obtained from the study population, it was possible to estimate a proportion of post-ERCP infections at the national level ranging from 2.7% to 5.7%. Assuming a constant differential in healthcare resource consumption attributed to post-ERCP infections and an annual volume of approximately 25,000 ERCP procedures performed in Italy in ordinary regimen, the economic burden of post-ERCP infections would amount to approximately € 3.0 million (95%CI € 1.9–€ 4.1 million) per year.
Discussion
This study aimed to assess the burden of post-ERCP infections in Italy by estimating the prevalence of hospital-acquired infections and evaluating their associated HCRU and economic impact. The observed proportion of post-ERCP infections in our study was 4.2%, with notable prevalence in older patients and emergency admissions, consistent with the literature. A recent study (12) identified 823,575 patients undergoing ERCP between January 2015 and December 2021 in the US, of which 3.5% were hospitalized for infection within 7 days from ERCP. Urgent ERCP, chronic conditions, older age, and non-white race were identified as the strongest risk factors for infection. Ayres et al. (14) aimed to evaluate variables that affect the risk of contamination for ERCP, and endoscopic ultrasound endoscopes found an overall pathogenic contamination rate of 4.72%. Finally, a single-center retrospective study of the first 200 ERCPs performed in the hospital reported an acute cholangitis rate from 4% to 1%, with a tendency to reduce with increased experience of the practitioner (25).
Our study highlighted a significant impact of post-ERCP infections on HCRU, resulting in prolonged hospital stays, higher readmission rates, and increased prescription of antibiotics and/or anticoagulants. In cases of infection following ERCP, the length of hospitalization more than doubled (24.3 days compared to 11.3 days). This result aligns with findings highlighted by Kuduva Rajan et al. (26), in a retrospective cross-sectional study utilizing data from 4,411 U.S. hospitals. In this case, the occurrence of post-ERCP infections resulted in an 89.7% increase in the LoS. The same impact was observed in a retrospective cohort study conducted in the United States using the National Readmission Database for the year 2016. The authors analyzed a total of 135,704 ERCPs; out of these, 8% were associated with post-ERCP bacteremia that led to significantly longer stays (10.71 vs. 5.64 days, +89.9%) (27).
Few studies have investigated the economic impact of post-ERCP infections, and all were conducted in the United States. Specifically, Kuduva Rajan et al (26) highlighted how patients with post-ERCP infection incurred significantly higher costs compared to those without infection ($107,520 vs. $53,554; p value <0.0001). Similarly, Bhurwal et al (27) estimated the impact of infections on costs, showing an increase from $58,351 to $119,517 (p=0.016). Our findings reveal a statistically significant increase in the average expenditure per patient, particularly evident in the context of hospitalization costs, which saw a notable rise of 55.75%. The economic burden, when extrapolated nationally, amounted to approximately €3.0 million per year, emphasizing the financial strain posed by these infections on the healthcare system.
Despite the comprehensive nature of our study, several limitations should be acknowledged. The reliance on administrative databases, which, by their very nature, were not designed for epidemiological research, introduces potential sources of bias such as underreporting and misclassification of key variables. Another notable limitation pertains to challenges in identifying patient-related clinical variables, leading to potential inaccuracy regarding disease severity and overall clinical history. The study also encounters constraints in tracking the specific utilization of medical devices.
Additionally, due to the retrospective nature of the study, the lack of information on pre- and post-treatment laboratory tests to confirm the presence of infection for all patients inherently introduces some limitations. This absence may result in the underdetection of post-ERCP infections that were managed exclusively in the community without hospital referral. Moreover, it poses a risk of overlooking patients already infected before undergoing the ERCP procedure.
However, the study is based on data from one of the largest hospital facilities in Italy, providing a sample that is representative of the national case scenario and offering insights into the economic implications of post-ERCP infections. The national extrapolation of economic burden provides a valuable perspective for healthcare policymakers. The identification of consistent risk factors aligns with existing literature, enhancing the reliability and generalizability of our findings.
Conclusions
The study provides valuable insight about the economic impact of post-ERCP infections within the Italian healthcare context, addressing a previously existing informational gap. The identified burden of infections is substantial in Italy, emphasizing the need for proactive preventive measures. By comparing our findings with existing literature, we further strengthen the robustness of the identified risk factors and their implications for healthcare outcomes and costs. Effectively addressing the challenge of post-ERCP infections is essential not only for enhancing patient care, but also for alleviating economic burden for the healthcare system and advancing the field of endoscopy.
Disclosures
Conflict of interest: The authors have no relevant financial or non-financial interests to disclose.
Financial support: This study was funded by Boston Scientific. The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author’s contribution: PS and FC: Conceptualization; AF and SMAG: Data Curation; PS: Formal Analysis and Software,Writing – original draft; All authors: Writing – review & editing.
References
- 1. Anderson MA, Fisher L, Jain R, et al; ASGE Standards of Practice Committee. Complications of ERCP. Gastrointest Endosc. 2012;75(3):467-473. CrossRef PubMed
- 2. Rauwers AW, Voor In ’t Holt AF, Buijs JG, et al. High prevalence rate of digestive tract bacteria in duodenoscopes: a nationwide study. Gut. 2018;67(9):1637-1645. CrossRef PubMed
- 3. Rauwers AW, Troelstra A, Fluit AC, et al. Independent root-cause analysis of contributing factors, including dismantling of 2 duodenoscopes, to investigate an outbreak of multidrug-resistant Klebsiella pneumoniae. Gastrointest Endosc. 2019;90(5):793-804. CrossRef PubMed
- 4. Chandra S, Klair JS, Soota K, Livorsi DJ, Johlin FC. Endoscopic retrograde cholangio-pancreatography-obtained bile culture can guide antibiotic therapy in acute cholangitis. Dig Dis. 2019;37(2):155-160. CrossRef PubMed
- 5. Masadeh M, Chandra S, Livorsi D, Johlin F, Silverman W. Evaluation of biliary bacterial resistance in patients with frequent biliary instrumentation, one size does not fit all. Dig Dis Sci. 2018;63(12):3474-3479. CrossRef PubMed
- 6. Kwakman JA, Erler NS, Vos MC, Bruno MJ. Risk evaluation of duodenoscope-associated infections in the Netherlands calls for a heightened awareness of device-related infections: a systematic review. Endoscopy. 2022;54(2):148-155. CrossRef PubMed
- 7. Gastmeier P, Vonberg RP. Klebsiella spp. in endoscopy-associated infections: we may only be seeing the tip of the iceberg. Infection. 2014;42(1):15-21. CrossRef PubMed
- 8. Deb A, Perisetti A, Goyal H, et al. Gastrointestinal endoscopy-associated infections: update on an emerging issue. Dig Dis Sci. 2022;67(5):1718-1732. CrossRef PubMed
- 9. Petersen BT, Koch J, Ginsberg GG. Infection using ERCP endoscopes. Gastroenterology. 2016;151(1):46-50. CrossRef PubMed
- 10. Aumeran C, Poincloux L, Souweine B, et al. Multidrug-resistant Klebsiella pneumoniae outbreak after endoscopic retrograde cholangiopancreatography. Endoscopy. 2010;42(11):895-899. CrossRef PubMed
- 11. Kim S, Russell D, Mohamadnejad M, et al. Risk factors associated with the transmission of carbapenem-resistant Enterobacteriaceae via contaminated duodenoscopes. Gastrointest Endosc. 2016;83(6):1121-1129. CrossRef PubMed
- 12. Hutfless S, Shiratori Y, Chu D, Liu S, Kalloo A. Risk factors for infections after endoscopic retrograde cholangiopancreatography (ERCP): a retrospective cohort analysis of US Medicare Fee-For-Service claims, 2015-2021. BMJ Open. 2022;12(9):e065077. CrossRef PubMed
- 13. Cennamo V, Landi S, Aragona G, et al. The management of endoscopic retrograde cholangio-pancreatography-related infections risk: results of an Italian survey at regional level. Ann Ig. 2023;35(1):84-91. PubMed
- 14. Ayres AM, Wozniak J, O’Neil J, et al. Endoscopic retrograde cholangiopancreatography and endoscopic ultrasound endoscope reprocessing: variables impacting contamination risk. Infect Control Hosp Epidemiol. 2023;44(9):1485-1489. CrossRef PubMed
- 15. Conti CB, Cereatti F, Salerno R, et al. Disposable duodenoscopes: evidence and open issues. Life (Basel). 2023;13(8):1694. CrossRef PubMed
- 16. Larsen S, Russell RV, Ockert LK, et al. Rate and impact of duodenoscope contamination: a systematic review and meta-analysis. EClinicalMedicine. 2020;25:100451. CrossRef PubMed
- 17. Rauwers AW, Kwakman JA, Vos MC, Bruno MJ. Endoscope-associated infections: a brief summary of the current state and views toward the future. Tech Gastrointest Endosc. 2019;21(4):150608. CrossRef
- 18. Rahman MR, Perisetti A, Coman R, Bansal P, Chhabra R, Goyal H. Duodenoscope-associated infections: update on an emerging problem. Dig Dis Sci. 2019;64(6):1409-1418. CrossRef PubMed
- 19. Epstein L, Hunter JC, Arwady MA, et al. New Delhi metallo-β-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA. 2014;312(14):1447-1455. CrossRef PubMed
- 20. Dabaja-Younis HK, Schechner V, Firan I, et al. Identification and control of two outbreaks of unrelated New Delhi metallo-β-lactamase-producing carbapenem-resistant Escherichia coli traced to the same endoscope defect. Infect Control Hosp Epidemiol. 2023;44(10):1673-1675. CrossRef PubMed
- 21. Humphries RM, Yang S, Kim S, et al. Duodenoscope-related outbreak of a carbapenem-resistant Klebsiella pneumoniae identified using advanced molecular diagnostics. Clin Infect Dis. 2017;65(7):1159-1166. CrossRef PubMed
- 22. Cristina ML, Sartini M, Schinca E, et al. Is post-reprocessing microbiological surveillance of duodenoscopes effective in reducing the potential risk in transmitting pathogens? Int J Environ Res Public Health. 2019;17(1):140. CrossRef PubMed
- 23. Fugazza A, Lamonaca L, Craviotto V, et al. Duodenoscope-related infections: an Italian pick in 2019. Gastrointest Endosc. 2020;91(6):AB369. CrossRef
- 24. Ministero della Salute. Rapporto annuale sull’attività di ricovero ospedaliero (Dati SDO 2019). 2020. Online
- 25. Riesco-López JM, Vázquez-Romero M, Rizo-Pascual JM, et al. Efficacy and safety of ERCP in a low-volume hospital 105, no. 2 68-73. s.l. Rev Esp Enferm Dig. 2013. CrossRef
- 26. Kuduva Rajan S, Madireddy S, Jaladi PR, et al. Burdens of postoperative infection in endoscopic retrograde cholangiopancreatography inpatients. Cureus. 2019;11(7):e5237. CrossRef PubMed
- 27. Bhurwal A, Pioppo L, Reja M, et al. Post ERCP bacteremia and post ERCP fever leads to early unplanned readmission – incidence and outcomes. Gastrointest Endosc. 2020;91(6):AB349-AB350. CrossRef