 |
Glob Reg Health Technol Assess 2023; 10: 1-11 ISSN 2283-5733 | DOI: 10.33393/grhta.2023.2492 ORIGINAL RESEARCH ARTICLE |
 |
Cost-minimization analysis to support the HTA of Radiofrequency Echographic Multi Spectrometry (REMS) in the diagnosis of osteoporosis
ABSTRACT
Introduction: A timely diagnosis of osteoporosis is key to reducing its growing clinical and economic burden. Radiofrequency Echographic Multi Spectrometry (REMS), a new diagnostic technology using an ultrasound approach, has been recognized by scientific associations as a facilitator of patients’ care pathway. We aimed at evaluating the costs of REMS vs. the conventional ionizing technology (dual-energy X-ray absorptiometry, DXA) for the diagnosis of osteoporosis from the perspective of the Italian National Health Service (NHS) using a cost-minimization analysis (CMA).
Methods: We carried out structured qualitative interviews and a structured expert elicitation exercise to estimate healthcare resource consumption with a purposeful sample of clinical experts. For the elicitation exercise, an Excel tool was developed and, for each parameter, experts were asked to provide the lowest, highest and most likely value. Estimates provided by experts were averaged with equal weights. Unit costs were retrieved using different public sources.
Results: Considering the base-case scenario (most likely value), the cost of professionals amounts to €31.9 for REMS and €48.8 for DXA, the cost of instrumental examinations and laboratory tests to €45.1 for REMS and €68.2 for DXA. Overall, in terms of current costs, REMS is associated with a mean saving for the NHS of €40.0 (range: €27.6-71.5) for each patient.
Conclusions: REMS is associated with lower direct healthcare costs with respect to DXA. These results may inform policy-makers on the value of the REMS technology in the earlier diagnosis for osteoporosis, and support their decision regarding the reimbursement and diffusion of the technology in the Italian NHS.
Keywords: Cost-minimization analysis, Dual-Energy X-ray Absorptiometry (DXA), Economic evaluation, Health Technology Assessment (HTA), Osteoporosis, Radiofrequency Echographic Multi Spectrometry (REMS)
Received: September 15, 2022
Accepted: January 15, 2023
Published online: February 6, 2023
Global & Regional Health Technology Assessment - ISSN 2283-5733 - www.aboutscience.eu/grhta
© 2023 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Osteoporosis is a systemic disease of the skeletal system, characterized by the deterioration of the density and quality of bone tissue, with a consequent increase in bone fragility and the risk of fracture (1). As people age, bone mass declines and the risk of fragility fractures increases (2). Prevalence of osteoporosis is increasing steadily (3), with an estimated worldwide prevalence of 18.3% (4). In Italy, it is estimated that approximately 3.2 million women and 0.8 million men suffer from osteoporosis, with a higher prevalence in the over 50 age group (5). Osteoporosis represents a relevant and growing public health problem, being a widespread and costly disease that generates a significant burden in terms of disability and impaired quality of life (6). In Italy, fragility fractures are associated with the loss of more than 500,000 healthy life years, ranking fourth among the most serious diseases (7). In addition, the direct health costs associated with fragility fractures amount to approximately 10 billion euros, with significant productivity losses (94 sick leave days/year for 1,000 individuals) (7). Thanks to significant advances in disease management over the last years, osteoporosis is now eminently treatable and the associated fragility fractures preventable (8,9). However, osteoporosis still remains both an underdiagnosed and undertreated disease (10-12). The International Osteoporosis Foundation revealed that restricted access to diagnosis before the first fracture is one of the main causes of osteoporosis underdiagnosis and undertreatment (13). Therefore, identifying patients at risk and making a timely diagnosis are key factors to help reduce the risk of fragility fractures and therefore the burden of the disease (14).
The diagnosis of osteoporosis is based on the assessment of bone mineral density or the anamnesis of femoral or vertebral fractures in adulthood in the absence of major trauma (15). To date, dual-energy X-ray absorptiometry (DXA) at the level of the lumbar spine and proximal femur represents the conventional technology for the diagnosis of osteoporosis (16). Despite the high accuracy of DXA, there are some factors that hinder its adequacy for mass screening, including the cost of the technology, the use of radiations and, in some cases, its limited accessibility (due to a limited number of densitometers, lack of qualified healthcare personnel to correctly perform the exam and/or absence of reimbursement in some countries) (17-19). Overall, this may limit the ability of the health system of timely diagnosing osteoporosis, with a negative impact on fracture prevention. Recently, a new technology that performs the analysis of bone quantity and quality through an ultrasound, non-ionizing approach, called Radiofrequency Echographic Multi Spectrometry (REMS), has been developed for the diagnosis of osteoporosis (20,21). The use of REMS technology for the diagnosis of osteoporosis has been clinically validated by several single-center and multicenter studies, which have shown that REMS has a precision and diagnostic accuracy at least comparable to that of DXA (18,20-23) in several patient populations, including postmenopausal women (18) and female patients aged between 30 and 90 years (22,23). Moreover, an Italian multicenter prospective observational study found that, for the vertebral site, REMS has a greater ability than DXA to identify true positives (i.e., osteoporotic patients who suffered an incident fragility fracture during follow-up) and a similar ability to identify true negatives (i.e., healthy patients who did not have fractures during follow-up), while for the femoral site the predictive ability is similar between REMS and DXA (22). Through its consensus paper published in 2019, the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases has established that REMS represents a valid approach for mass population screening, early diagnosis and therapeutic monitoring (19). In fact, the REMS approach presents some advantages including the absence of radiation, the easy portability of the device and its lower cost (17). In 2021, the Italian Inter-Society Health Ministry Guidelines developed by the Italian National Institute of Health – Istituto Superiore di Sanità (ISS) – for the “Diagnosis, risk stratification and continuity of care for Fragility Fractures” recognized the REMS ultrasound examination as a diagnostic technology that can facilitate the patients’ care pathway (24).
To complement the current evidence on the clinical value of REMS, the objective of this study was to evaluate the costs associated with the use of the REMS approach for the diagnosis of osteoporosis compared to DXA from the perspective of the Italian National Health Service (NHS) using a cost-minimization analysis (CMA), based on the assumption that the two approaches have comparable diagnostic precision and accuracy and therefore guarantee equivalent health outcomes.
Methods
We performed structured, individual qualitative interviews with a selected sample of clinicians (n = 6) who are recognized experts in the diagnosis and management of patients with osteoporosis and in the use of the REMS technology (e.g., authors of peer-reviewed publications on REMS). The interview guide is reported as Supplementary file 1. Clinicians were selected through a purposive sampling to reflect current practice across different specialties (namely radiology, gynecology, internal medicine, orthopedics and traumatology, endocrinology and rheumatology) and Italian regions (Lombardia, Veneto, Emilia Romagna, Toscana, Lazio, Puglia). The interviews had the objective of: (i) understanding the current and future use of REMS (being a technology recently introduced in the Italian NHS); (ii) gathering qualitative information on the diagnostic pathway and follow-up of osteoporotic patients; (iii) identifying the target population of REMS and DXA; (iv) identifying the types of healthcare resources consumed (e.g., outpatient visits, laboratory tests, healthcare personnel involved) for the diagnosis of osteoporosis. Information collected through qualitative interviews, especially regarding points (iii) and (iv), was used to develop the CMA model.
An initial review of the literature revealed that resource consumption data for both DXA and REMS in Italy are scant. Therefore, we performed a structured expert elicitation exercise in order to collect quantitative estimates of healthcare resource consumption. Structured expert elicitation is the process by which the beliefs of experts about unknown quantities or parameters can be formally collected in a quantitative manner (25,26). Expert elicitation is a useful approach when evidence is missing, is not well developed or limited (27). Expert elicitation is increasingly recognized as a valuable method for informing healthcare decision-making as it allows to quantify parameter uncertainty and take it into account within an economic evaluation model (28). Clinical experts involved in the qualitative interviews and other clinicians purposefully identified, who are current users of and knowledgeable about the REMS approach (e.g., authors of peer-reviewed publications on REMS) and are experts in the diagnosis and management of patients with osteoporosis, were invited to participate in the elicitation exercise. A purposeful sampling was deemed appropriate in order to identify information-rich cases, that is, individuals who are especially knowledgeable about or experienced with the phenomenon of interest (29). We developed an ad hoc tool on Microsoft Excel. For each parameter of interest, we asked experts to provide three point estimates, that is, the lowest (L), highest (H) and most likely value (M). As the target population for REMS and DXA can be quite heterogeneous (as confirmed by the clinicians interviewed), for the purposes of the CMA we considered women aged between 30 and 90 years as the target population, as it was the most cited by the clinicians interviewed and the one considered in several studies on REMS (22,23). In the Excel tool, clinicians were explicitly invited to give their estimates considering this target population.
The tool was developed for self-administration, and was sent by email with instructions for autonomous completion. Although face-to-face elicitation is recommended for some consensus methods and can be beneficial in terms of experts’ performance and engagement, it is not deemed necessary when the purpose of the study is to aggregate judgments mathematically (28). The tool consisted of an initial introductory section, with summary information on the study objectives and methods, and a questionnaire section, where experts were invited to provide their resource consumption estimates separately for REMS and DXA. In this section, clinicians were asked to indicate either the quantity of resources consumed (e.g., the time in minutes dedicated by different healthcare professionals in carrying out the diagnostic examination) or the percentage of patients consuming a certain resource (e.g., percentage of patients undergoing a certain laboratory test). The main cost items for which we gathered experts’ estimates were: (i) healthcare professionals’ time; (ii) administrative professionals’ time; (iii) additional instrumental examinations; (iv) laboratory tests; (v) consumables. The tool automatically verified the completeness and consistency of the estimates provided (e.g., that the M estimate was lower than the H and higher than the L) through a series of macros. In case data were not complete or consistent, an error message appeared, inviting responders to provide or correct their estimates in order to proceed with completion. Clinical experts filled in the tool between November 2021 and January 2022, and analyses were carried out in February 2022. Collected data were analyzed by averaging the estimates provided by experts. All experts were given equal weight.
Unit costs were retrieved using different sources in order to evaluate the consumption in monetary terms and perform the CMA. The unit costs of laboratory tests and instrumental examinations were sourced from “Nomenclatore dell’assistenza specialistica ambulatoriale”, an official document providing Italian national tariffs for outpatient services (30). Gross wage of personnel working in the healthcare sector was retrieved from “Conto annuale”, a census survey on Italian public administrations that provides data on the annual wages of Italian public employees for the latest year available (2019) (31). As regards residents, their gross wage, which is established by law, was retrieved from the official Decree of the Italian Ministry of Health (32). All wages were adjusted for inflation to 2021 (adjustment coefficient: 1.030) (33). In order to derive the wage per minute, we calculated the average number of working days and minutes based on the information provided in the most recent National Collective Work Contract, which regulates the working conditions for the professionals employed in the NHS (34). The cost of the devices (REMS and DXA) was collected from the accounting departments of the hospitals in which clinicians involved in the expert elicitation exercise operate (clinicians were asked on a voluntary basis to provide these data in a section of the tool).
We provided three different scenarios: (i) the base-case scenario (only M values considered); (ii) the most conservative scenario (only L values considered); (iii) the least conservative scenario (only H values considered). We calculated the difference in resource consumption and costs for REMS and DXA. The equality of estimates’ mean was assessed through a Student’s t-test (the p-value was reported). We provided separate estimates for current costs (e.g., time dedicated by personnel for diagnosis, laboratory test, etc.) and one-off costs (e.g., training and cost of the device).
A one-way deterministic sensitivity analysis was performed in order to assess how parameters’ uncertainty affected the results for current costs. Elicited parameters were varied according to their minimum (L) and maximum (H) estimate using the base-case scenario as reference. Unit costs and tariffs were varied according to ±20%. Results were graphically represented through tornado diagrams; only the parameters with the highest impact on costs were shown.
Results
Fifteen clinicians were invited to participate in the expert elicitation exercise. Thirteen of them agreed to participate and filled in the Excel tool (response rate = 85%; completion rate = 100%). The experts involved in this phase operate in seven Italian regions (i.e., Emilia-Romagna, Lazio, Liguria, Lombardia, Piemonte, Puglia, Toscana), in both private and public facilities, are representative of different medical specialties, and have an average experience of 24.5 years in the management of patients with osteoporosis (Supplementary table 1).
The clinicians provided all data compulsorily requested (i.e., there were not missing data as regards REMS and DXA resource consumption). Three clinicians completed only the section relative to REMS as they declared to have no experience of use of DXA.
Current costs
Supplementary table 2 shows the number of professionals involved, and the time (in minutes) dedicated by each professional to the different activities for the diagnosis of osteoporosis, for REMS and DXA approach respectively.
The total time dedicated to diagnosis by the different professionals was computed by multiplying the number of professionals involved in the diagnosis by the time dedicated to the different activities, separately for each responder. Then, the different estimates obtained for all responders were averaged. Table I reports the estimates relative to the total time dedicated to diagnosis (in minutes) by each professional figure for the three scenarios.
Table I also shows resource consumption estimates related to additional instrumental exams and laboratory tests for the diagnosis of osteoporosis. The high proportion of patients undergoing a DXA exam after REMS is due to the fact that, at the time of this study, DXA was the only diagnostic exam recognized by the Italian Medicines Agency (Agenzia Italiana del Farmaco – AIFA) for the prescription and reimbursement of some high-cost drugs (35,36). For this reason, in cost calculation we did not consider this item. In order to counterbalance this omission and be conservative in our estimates, we did not consider the REMS exam performed after DXA. However, unlike the former case, the execution of REMS after DXA is not driven by drug prescription and reimbursement needs. Therefore, we may infer that clinicians voluntarily decide to perform REMS after DXA to improve the diagnosis of osteoporosis, for example, in those cases where DXA results can be biased by the presence of some artifacts (e.g., osteoarthritis, previous vertebral fracture), as underlined by the interviewees.
TABLE I - Resource consumption estimates
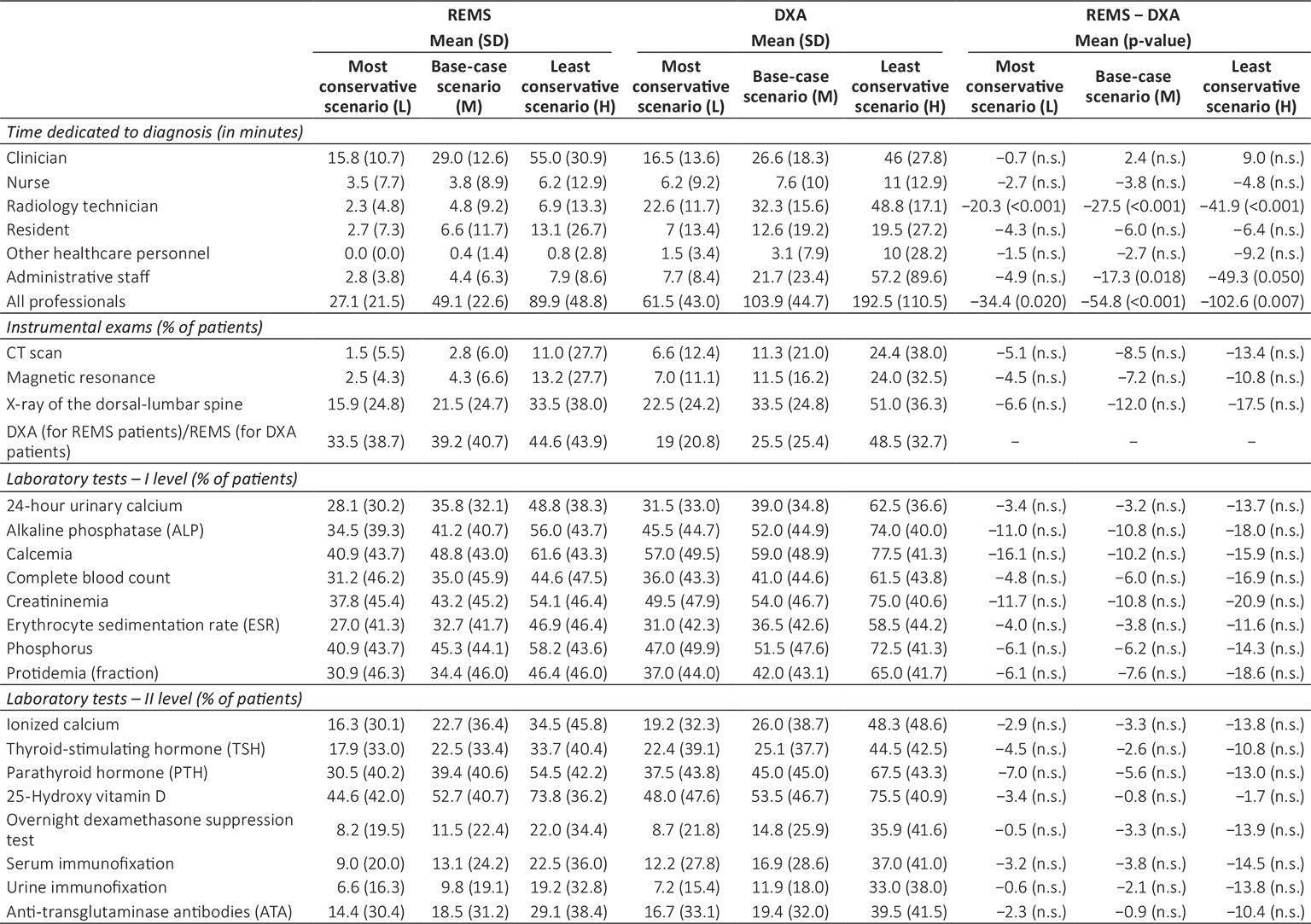
Since the p-value is also affected by the sample size (the smaller the sample size, the higher the p-value), we should be careful in interpreting the lack of statistical significance of the difference in estimates (as it may be partly driven by the low number of observations).
CT = computed tomography; DXA = dual-energy X-ray absorptiometry; n.s. = not significant; REMS = Radiofrequency Echographic Multi Spectrometry; SD = standard deviation.
The cost of consumables (i.e., gloves, medical bed sheet, disinfectant, gel) was not considered in the present analysis due to the very limited quantity used for both exams and their contained unit cost.
Supplementary table 3 reports the gross wages of professionals (31,32), and Supplementary table 4 shows the unit cost of instrumental exams and laboratory tests (30).
Table II shows the average cost of personnel (healthcare professionals and administrative staff), instrumental examinations and laboratory tests for the diagnosis of osteoporosis. Considering the base-case scenario, the cost of all professionals for the diagnosis of osteoporosis amounts to €31.9 for REMS and €48.8 for DXA, entailing a saving of €16.9 for REMS. It is interesting to note that, for REMS, the cost of clinicians represents the major driver of personnel cost (approximately 80% of the total personnel cost). For DXA, the personnel cost is more distributed across different professional figures, namely clinicians (48%), radiology technicians (24%) and administrative staff (14%). These findings suggest that the use of DXA usually entails the involvement of more professional figures than REMS, with potential consequences in terms of increasing need of coordination and thus organizational costs. The cost of instrumental examinations and laboratory tests amounts to approximately €45.1 for REMS and €68.2 for DXA, with a saving of €23.1 for REMS.
Overall, the use of REMS approach for the diagnosis of osteoporosis is associated with a mean saving for the NHS of €40.0 (range: €27.6-€71.5) for each patient (Fig. 1). By increasing the number of patients diagnosed through the REMS approach (see Fig. 2 for the base-case scenario), the NHS would be able to save a significant amount of healthcare resources to diagnose osteoporosis (approximately €40.000 saved every 1,000 diagnosed patients).

Fig. 1 - Total costs and difference in costs for Radiofrequency Echographic Multi Spectrometry and dual-energy X-ray absorptiometry.
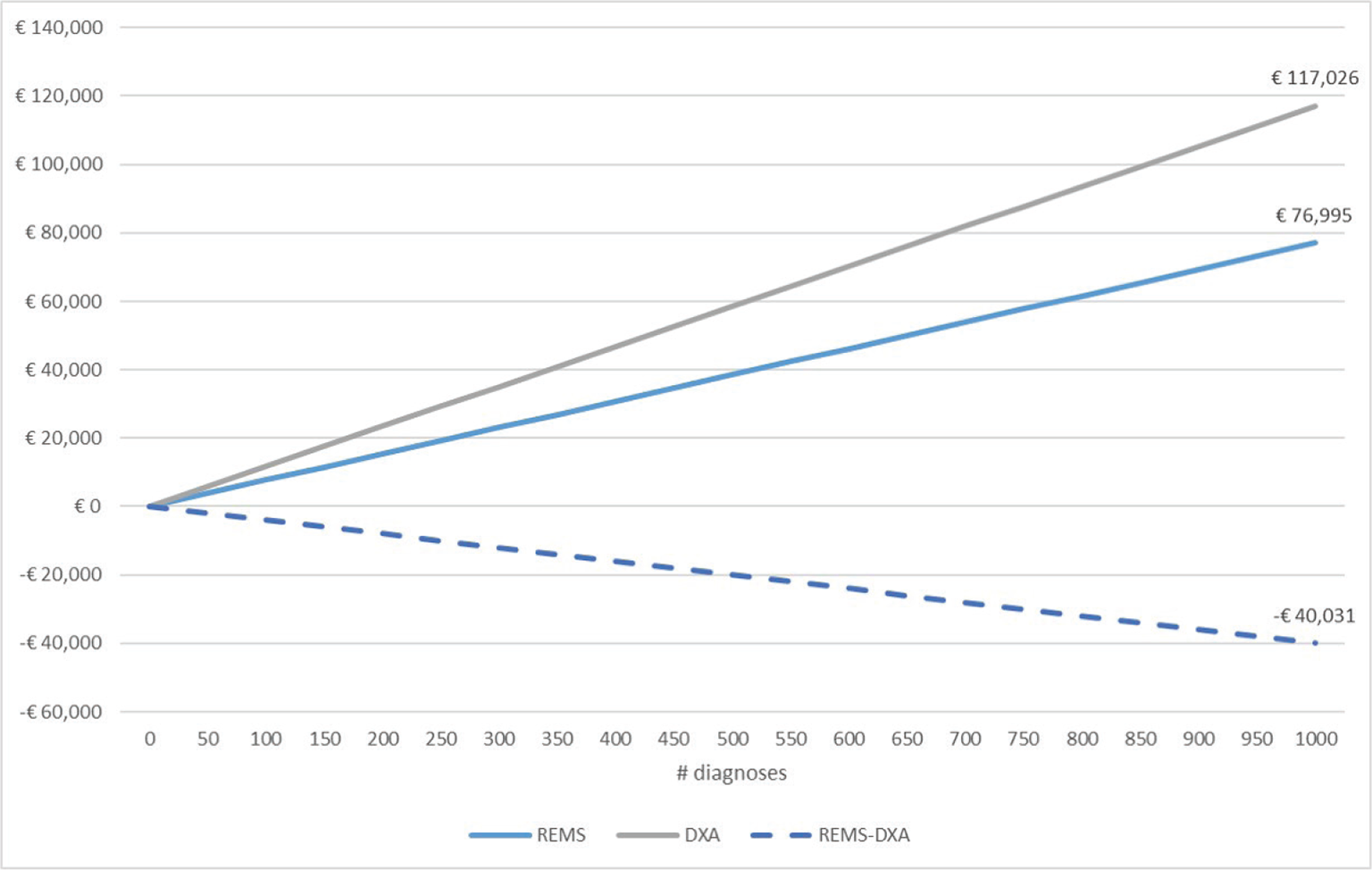
Fig. 2 - Cumulative costs and savings (base-case scenario).
TABLE II - Current costs for the diagnosis of osteoporosis
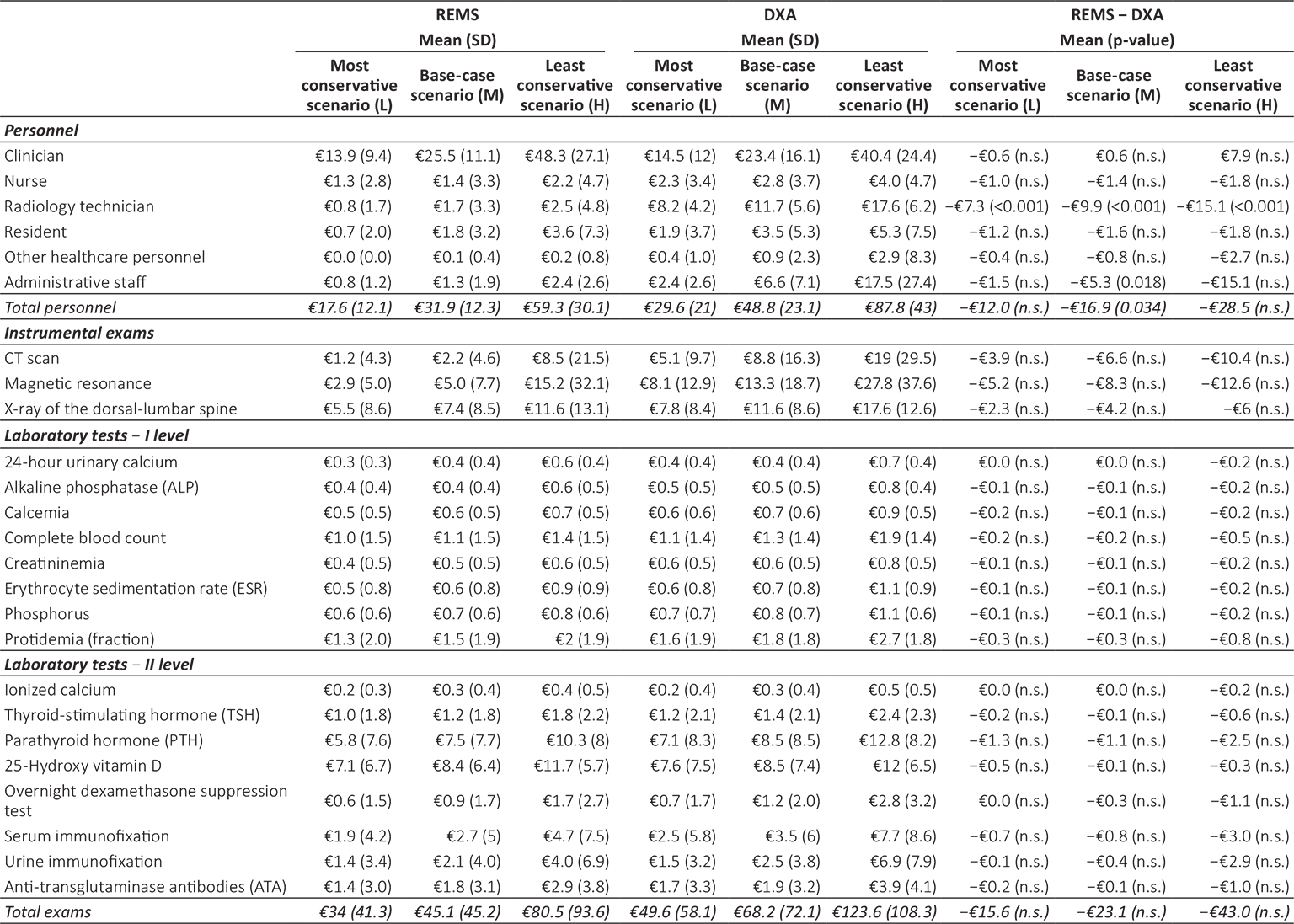
CT = computed tomography; DXA = dual-energy X-ray absorptiometry; n.s. = not significant; REMS = Radiofrequency Echographic Multi Spectrometry; SD = standard deviation.
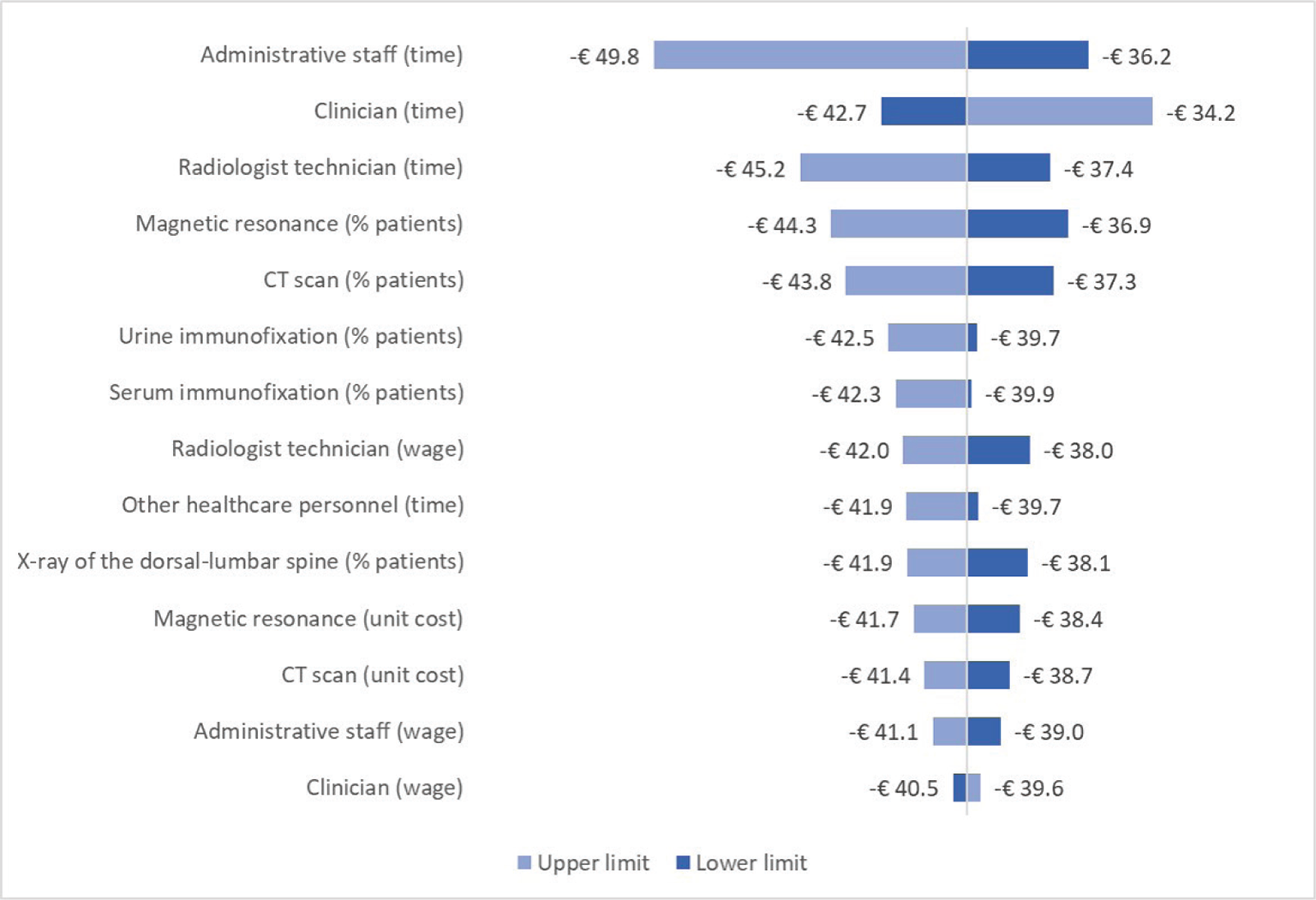
Fig. 3 - Sensitivity analysis – Difference in costs between Radiofrequency Echographic Multi Spectrometry and dual-energy X-ray absorptiometry.
According to the sensitivity analysis, the two parameters whose variation has the largest impact both on REMS and DXA costs are the time dedicated by clinicians to diagnosis and the percentage of patients undergoing magnetic resonance as additional instrumental exam (Supplementary figure 1, Supplementary figure 2). In particular, when the time dedicated by clinicians is varied according to its lower (L estimate) and upper (H estimate) limit, the cost of REMS ranges from €65.4 to €99.8, while the cost of DXA was from €108.2 to €134.1. The three parameters whose variation has the largest impact on the difference in costs between REMS and DXA are the time dedicated by administrative staff, clinicians and radiology technicians (Fig. 3).
One-off costs
In the tool, clinicians were asked to provide an estimate of the training time dedicated by the healthcare professionals to learn how to use the technology in clinical practice, both for REMS and DXA (Supplementary table 5). Considering the base-case scenario, the training for REMS entails a lower amount of time dedicated by healthcare professionals, resulting in a one-off cost of €357.4 compared to €1,169.0 for DXA (Tab. III). A lower training time is likely to be beneficial not only in terms of technology-related costs but also in terms of organizational impact, and could be used to leverage the introduction and uptake of REMS in clinical practice.
Six clinicians provided us with the data regarding the cost of REMS device, and three with the cost of DXA technology (for different models, namely Hologic Horizon, Hologic Lunar and Hologic Discovery). By averaging the values provided, which were quite heterogeneous, the unit cost of acquisition (with VAT) for REMS equals €32,833 (with no maintenance costs), while for DXA it was €45,000 (including €5,000 for maintenance costs). Moreover, although not considered in the present analysis, the use of DXA requires a dedicated radiology room, with a relevant investment for its set-up (e.g., to shield medical personnel from harmful secondary radiation), while REMS can be used in the ambulatory or at the bed of the hospitalized patient or at the patient’s home.
Discussion
REMS has been recognized by international and national scientific associations as a promising approach for the diagnosis of osteoporosis (19,24). In 2021, the Italian Inter-Society Health Ministry Guidelines developed by the Italian National Institute of Health – Istituto Superiore di Sanità (ISS) on Fragility Fractures have stated that, on the basis of published scientific evidence, “REMS reaches a good level of accuracy and precision, is a good predictor of fragility fracture risk and may improve the diagnosis of osteoporosis in the routine care” (page 1173) (24). Moreover, the guidelines envisage a substantial range of applications for REMS, wider than for DXA, including: (i) fracture risk assessment in pediatric patients, pregnant women and patients at risk of secondary osteoporosis (e.g., diabetic or oncological patients); (ii) use in primary care (in some countries, the need for radiological protection with DXA could represent a problem), (iii) use in fractured and non-transferable hospitalized patients (thanks to REMS ease of transportation). Overall, the guidelines recognize that REMS can improve the “continuity of care at the patients’ home” (page 1172) (24). The clinicians interviewed in the present study cited several characteristics of REMS that could favor its diffusion in the coming years, also as a screening method: (i) simplicity of the method; (ii) practicality and portability of the device (e.g., use on bedridden patients); (iii) possibility of following the patient on the territory rather than in the hospital, in line with the recent indications of the Italian Piano Nazionale Resistenza e Resilienza (PNRR); (iv) possibility for the clinician to manage the diagnosis independently, without having to rely on the radiology technician and radiologist for the execution and reporting of the examination respectively; (v) greater reliability in case of artifacts (e.g., osteoarthritis, previous vertebral fracture, calcifications, osteophytes, etc.); (vi) absence of ionizing radiation (use in women of childbearing age, pregnant women and children); (vii) possibility for the patient to be diagnosed timely, avoiding the long waiting lists for DXA in some local or regional contexts in Italy.
TABLE III - Cost of personnel for training
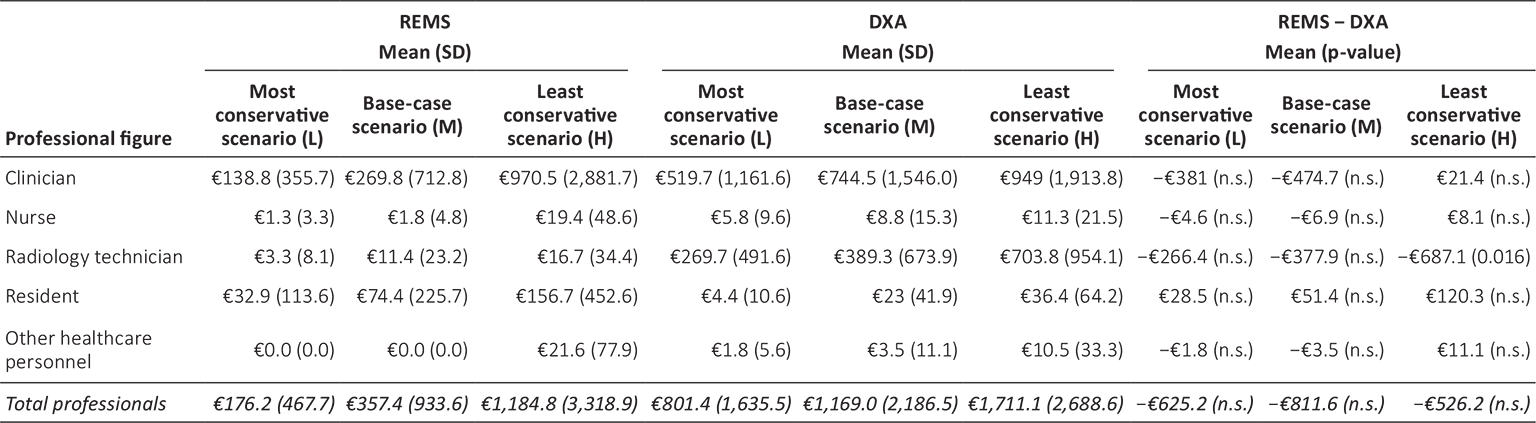
Since the p-value is also affected by the sample size (the smaller the sample size, the higher the p-value), we should be careful in interpreting the lack of statistical significance of the difference in estimates (as it may be driven by the low number of observations).
DXA = dual-energy X-ray absorptiometry; n.s. = not significant; REMS = Radiofrequency Echographic Multi Spectrometry; SD = standard deviation.
To the best of our knowledge, this is the first study investigating the direct healthcare costs associated with the use of the REMS approach vs. DXA for the diagnosis of osteoporosis. The results of our CMA, conducted from the perspective of the Italian NHS, suggest that the REMS approach is associated with lower direct healthcare costs with respect to DXA. Overall, in fact, the mean current costs amount to €77.0 for REMS (€31.9 for time dedicated by healthcare personnel and administrative staff, and €45.1 for additional instrumental exams and laboratory tests) and to €117.0 for DXA (€48.8 for time dedicated by healthcare personnel and administrative staff, and €68.2 for additional instrumental exams and laboratory tests). Also one-off costs are lower for the REMS approach: €357.4 vs. €1,169.0 for training, and €32,833 vs. €45,000 for the acquisition of the device. These findings may inform the decision regarding the inclusion of REMS among Livelli Essenziali di Assistenza, that is, the healthcare services and treatments that the Italian NHS provides to all citizens free of charge or upon payment of a fee. In particular, the evidence on REMS direct healthcare costs could be used by policy-makers to define a fair reimbursement tariff for this novel diagnostic approach, reflecting the cost actually borne by the healthcare system in delivering the care service.
Besides the cost estimates and results provided in the present analysis, it is worth noting that a higher diffusion of REMS could generate additional savings for the healthcare system, the patients and the society as a whole.
In a section of the tool, clinicians declared that, on average, the instrumental exam execution is concomitant with the specialist outpatient visit in the 70% of cases with REMS (L = 56%, H = 88%) while only in the 19% of cases with DXA (L = 12%; H = 35%). Moreover, the communication of diagnostic results is concomitant with exam execution in the 81% of cases with REMS (L = 70%; H = 93%) while only in the 29% of cases with DXA (L = 22%; H = 45%). Although patients now have the possibility to access their medical reports online, the fact that, in the majority of cases, the REMS exam is concomitant with the specialist outpatient visit translates into a significantly lower number of accesses for patients diagnosed with the REMS approach. In turn, this implies savings in terms of direct non-healthcare costs (e.g., cost of transportation for the patient and cost of informal caregiving) and indirect costs (e.g., loss of productivity due to absence from work or leisure time lost).
In the tool clinicians also declared that, on average, 25% of patients cannot undergo DXA due to several reasons (e.g., bedridden patients, pregnant women, etc.). Moreover, the average frequency of follow-up is different between the two approaches: 21 months for DXA (L = 13; H = 28) and 13 months for REMS (L = 9; H = 19). The higher frequency of follow-up and the higher number of patients who can access REMS may have a significant and positive impact on the ability of the NHS to timely diagnose osteoporosis and prevent fragility fractures (as also underlined in the 2021 Italian Inter-Society Health Ministry Guidelines on Fragility Fractures), with a positive impact on both the patient and the overall healthcare system. A prospective observational study with a 5-year follow-up found that REMS is more effective than DXA in identifying incident fragility fractures both at the vertebral (OR = 2.6 for REMS vs. 1.7 for DXA) and the lumbar site (OR = 2.81 for REMS vs. 2.68 for DXA) (22). Fragility fractures have been demonstrated to be associated with a substantial clinical and economic burden. In fact, the study by Borgström and colleagues (2020) (7) estimated that, in Italy, the mean direct healthcare cost of a hip fracture amounts to €21,307, the cost of a vertebral fracture to €4,713 and the cost of a forearm fracture to €1,301. Moreover, the authors reported that, in 2017, the Quality-Adjusted Life-Years lost due to morbidity and mortality associated with osteoporotic fractures in our country were approximately 229,000, and they envisage that these estimates will increase in the next few years due to changing demography. These data suggest that a delay in diagnosis of osteoporosis and fragility fractures will likely translate into a higher burden for the NHS and the society as a whole. Following the Italian Inter-Society Health Ministry Guidelines, a more widespread use of REMS could help enhance the ability of the NHS to improve the overall diagnostic pathway for osteoporosis.
Although this study contributed at filling the evidence gap on the economic impact of REMS and DXA, it has some limitations. Coherently with other expert elicitation studies, we relied on a purposive sample of experts rather than on a random one. Although a purposive sampling may be subject to selection bias issues, it allowed us to carefully select clinicians on the basis of their recognized expertise in the management of patients with osteoporosis and the use of the technology, which could not be possible through a random sampling. This is particularly true for recently introduced technologies, like REMS, for which the number of clinicians knowledgeable about the technology itself is very limited. In line with Bojke and colleagues (28), in selecting the experts for the elicitation exercise we relied on three typically used criteria, that is, normative expertise, substantive expertise and willingness to participate. Moreover, we took into account their geographical distribution, in order to capture heterogeneity in clinical practice in different Italian regions, and different medical specialties (i.e., endocrinology, gynecology, internal medicine, orthopedics, physiatry, radiology and rheumatology). Finally, as suggested by Bojke and colleagues (28), we attempted to minimize experts’ motivational biases by ensuring that our sample contained a range of different viewpoints.
Another limitation concerns the impossibility to retrieve some of the cost data regarding DXA technology (e.g., investment cost for setting up the radiology room), possibly underestimating the cost associated with DXA.
Future avenues of research may explore prospectively the economic impact of the prevention of fragility fractures with REMS vs. DXA in the Italian clinical practice.
Conclusion
Clinical studies have shown that REMS has a diagnostic accuracy and precision at least comparable to that of DXA. Moreover, scientific associations and the 2021 Italian Inter-Society Health Ministry Guidelines on Fragility Fractures have recognized that REMS is a valuable diagnostic approach for osteoporosis that may facilitate the patients’ care pathway. These results and those provided by the present study regarding the economic impact of the two diagnostic approaches may inform policy-makers on the value of the REMS approach in the earlier diagnosis for osteoporosis, and support their decision regarding the reimbursement and diffusion of the technology in the Italian NHS. In particular, the results of this study may contribute to the definition of a fair reimbursement tariff for REMS, which is not yet comprised in Livelli Essenziali di Assistenza, and which should reflect the cost borne by the healthcare system in delivering the care service.
Disclosures
Funding: CERGAS SDA Bocconi received a research grant from Echolight S.p.A. for this study. The funder had no access to the dataset and had no role in study design, data collection or analysis.
Conflict of interest: Ludovica Borsoi and Patrizio Armeni declare no potential conflicts of interest with respect to the research, authorship and publication of this study. Maria Luisa Brandi declares the following competing interests: Echolight S.p.A. (consulting fees).
Author contributions: Conceptualization, Ludovica Borsoi and Patrizio Armeni; Data curation, Ludovica Borsoi; Formal analysis, Ludovica Borsoi; Funding acquisition, Ludovica Borsoi and Patrizio Armeni; Investigation, Ludovica Borsoi; Methodology, Ludovica Borsoi and Patrizio Armeni; Project administration, Ludovica Borsoi and Patrizio Armeni; Supervision, Patrizio Armeni; Visualization, Ludovica Borsoi; Writing – original draft, Ludovica Borsoi; Writing – review and editing, Ludovica Borsoi, Patrizio Armeni and Maria Luisa Brandi.
Research ethics: The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Università Commerciale Luigi Bocconi.
References
- 1. Consensus development conference. Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94(6):646-650. CrossRef PubMed
- 2. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761-1767. CrossRef PubMed
- 3. Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006;194(2)(suppl):S3-S11. CrossRef PubMed
- 4. Salari N, Ghasemi H, Mohammadi L, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609. CrossRef PubMed
- 5. International Osteoporosis Foundation, Fondazione FIRMO. OSSA SPEZZATE, VITE SPEZZATE: un piano d’azione per superare l’emergenza delle fratture da fragilità in Italia. 2017. Online. Accessed September 2022.
- 6. Pazianas M, Miller P, Blumentals WA, Bernal M, Kothawala P. A review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristics. Clin Ther. 2007 Aug;29(8):1548-1558. CrossRef PubMed
- 7. Borgström F, Karlsson L, Ortsäter G, et al; International Osteoporosis Foundation. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos. 2020;15(1):59. CrossRef PubMed
- 8. Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology of osteoporosis. Br Med Bull. 2020;133(1):105-117. PubMed
- 9. Khosla S, Hofbauer LC. Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol. 2017 Nov;5(11):898-907. CrossRef PubMed
- 10. Morris CA, Cabral D, Cheng H, et al. Patterns of bone mineral density testing: current guidelines, testing rates, and interventions. J Gen Intern Med. 2004;19(7):783-790. CrossRef PubMed
- 11. Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res. 2016;31(8):1485-1487. CrossRef PubMed
- 12. Hernlund E, Svedbom A, Ivergård M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8(1):136. CrossRef PubMed
- 13. International Osteoporosis Foundation. How fragile is her future? 2000. Online. Accessed September 2022.
- 14. Levine JP. Identification, diagnosis, and prevention of osteoporosis. Am J Manag Care. 2011;17(6)(suppl 6):S170-S176. PubMed
- 15. Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002 Jun 1;359(9321):1929-1936. CrossRef PubMed
- 16. Rossini M, Adami S, Bertoldo F, et al. Guidelines for the diagnosis, prevention and management of osteoporosis. Reumatismo. 2016 Jun 23;68(1):1-39. CrossRef PubMed
- 17. Caffarelli C, Pitinca MDT, Francolini V, Alessandri M, Gonnelli S. REMS technique: future perspectives in an academic hospital. Clin Cases Miner Bone Metab. 2018;15(2):163-165. Online
- 18. Di Paola M, Gatti D, Viapiana O, et al. Radiofrequency echographic multispectrometry compared with dual X-ray absorptiometry for osteoporosis diagnosis on lumbar spine and femoral neck. Osteoporos Int. 2019;30(2):391-402. CrossRef PubMed
- 19. Diez-Perez A, Brandi ML, Al-Daghri N, et al. Radiofrequency echographic multi-spectrometry for the in-vivo assessment of bone strength: state of the art-outcomes of an expert consensus meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Aging Clin Exp Res. 2019;31(10):1375-1389. CrossRef PubMed
- 20. Casciaro S, Peccarisi M, Pisani P, et al. An advanced quantitative echosound methodology for femoral neck densitometry. Ultrasound Med Biol. 2016;42(6):1337-1356. CrossRef PubMed
- 21. Conversano F, Franchini R, Greco A, et al. A novel ultrasound methodology for estimating spine mineral density. Ultrasound Med Biol. 2015;41(1):281-300. CrossRef PubMed
- 22. Adami G, Arioli G, Bianchi G, et al. Radiofrequency echographic multi spectrometry for the prediction of incident fragility fractures: A 5-year follow-up study. Bone. 2020;134:115297. CrossRef PubMed
- 23. Cortet B, Dennison E, Diez-Perez A, et al. Radiofrequency Echographic Multi Spectrometry (REMS) for the diagnosis of osteoporosis in a European multicenter clinical context. Bone. 2021;143:115786. CrossRef PubMed
- 24. Sistema nazionale per le linee guida. Diagnosi, stratificazione del rischio e continuità assistenziale delle Fratture da Fragilità. 2021. Online. Accessed September 2022.
- 25. Colson AR, Cooke RM. Expert elicitation: using the classical model to validate experts’ judgments. Rev Environ Econ Policy. 2018;12(1):113-132. CrossRef
- 26. Bojke L, Soares M, Claxton K, et al. Developing a reference protocol for structured expert elicitation in health-care decision-making: a mixed-methods study. Health Technol Assess. 2021;25(37):1-124. CrossRef PubMed
- 27. Soares MO, Bojke L. Expert elicitation to inform health technology assessment. In: Dias LC, Morton A, Quigley J, eds. Elicitation: the science and art of structuring judgement. Springer International Publishing 2018; 479-494. CrossRef
- 28. Bojke L, Soares MO, Claxton K, et al. Reference case methods for expert elicitation in health care decision making. Med Decis Making. 2022;42(2):182-193. CrossRef PubMed
- 29. Creswell JW, Poth CN. Qualitative inquiry and research design: choosing among five approaches. SAGE Publications 2016. Online
- 30. Ministero della Salute. Nomenclatore dell’assistenza specialistica ambulatoriale. Online. Accessed September 2022.
- 31. Conto annuale – Costo del lavoro. Online. Accessed September 2022.
- 32. Determinazione del numero globale dei medici specialisti da formare per il triennio 2020/2023 ed assegnazione dei contratti di formazione medica specialistica alle tipologie di specializzazioni per l’anno accademico 2020/2021 (GU Serie Generale n.229 del 24-09-2021). Online. Accessed September 2022.
- 33. Italian National Institute of Statistics (ISTAT). Rivaluta. Online. Accessed September 2022.
- 34. CCNL 2016-2018 del Comparto Sanità. Online. Accessed September 2022.
- 35. Agenzia Italiana del Farmaco (AIFA). Nota 79. Online. Accessed September 2022.
- 36. Agenzia Italiana del Farmaco (AIFA). Nota 96. Online. Accessed September 2022.