 |
Glob Reg Health Technol Assess 2022; 9: (Suppl. 2): 10-13 ISSN 2283-5733 | DOI: 10.33393/grhta.2022.2427 REVIEW |
 |
Socio-economic impact of epilepsy in Italy
ABSTRACT
The World Health Assembly recognizes the growing economic and societal burden of neurological disorders, a leading cause of disability and the second cause of mortality in the world.
In this context we analysed the socio-economic impact of epilepsy in Italy with a specific focus on hospitalizations and costs related to disability pensions (DPs) and ordinary disability allowances.
In the case of epilepsy, between 2009 and 2015 we observed an alarming increasing trend for DPs (+26%), indicating that substantial expenses must be supported throughout the patients’ lifetimes by both the social security system and the National Health Service (NHS) on top of the impact on caregivers.
We also analysed the hospital expenditure on epilepsy through the information available in the Hospital Discharge Cards between 2015 and 2018. Almost all admissions (76% ordinary hospitalizations, 24% day hospitals) were acute (95%), followed by rehabilitation (4%) and long-term care (1%).
The cost of acute and ordinary hospitalizations was by far the highest in 2018, the last year of analysis. This large expense due to hospitalizations could be reduced through the implementation of different organizational and management approaches. Our recommendation is that the policy maker should consider the best approach to ensure an early diagnosis for patients and provide early access to drugs and/or surgery. Finally, the adoption of new innovative treatments should improve effectiveness and, at the same time, reduce the expense of the NHS, of the social system as a whole, with a tangible improvement in patients’ quality of life.
Keywords: Co-morbidities, Economic burden, Economic impact, Epilepsy
Received: May 23, 2022
Accepted: May 30, 2022
Published online: June 28, 2022
Global & Regional Health Technology Assessment - ISSN 2283-5733 - www.aboutscience.eu/grhta
© 2022 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Epilepsy is a chronic brain disorder that affects people worldwide. It is characterized by the recurrence of phenomena called seizures, usually of short duration (seconds or a few minutes). Seizures may occur together with altered consciousness and/or involuntary movements affecting only one part of the body (partial motor seizure). Indeed, seizures can be of different types according to their complexity. More specifically, it is possible to distinguish between: partial seizures which can be more or less developed (simple or complex partial sensory seizures) or generalized seizures which involve the whole body, causing loss of consciousness and sometimes loss of sphincter control (1).
In order to ensure the proper attention that seizures deserve, the World Health Assembly (WHA), that is, the decision-making body of the World Health Organization (WHO), approved resolution WHA73.10 (12 Nov 2020) for ‘Global action on epilepsy and other neurological disorders.’ The resolution strongly encourages member states to provide an ‘integrated (multisector) response about epilepsy as well as other neurological disorders.’
This resolution is crucial for global neurology since it recognizes the growing economic and societal burden of neurological disorders, which are the leading cause of disability and the second cause of mortality all over the world.
Disability and mortality do not imply solely significant effects in terms of reduced health and increased costs for the National Health Service (NHS), but they produce effects also in terms of reduced quality of life (QoL), productivity loss (for both patient and caregiver), and costs borne by the society’s security system (disability pensions [DPs] and ordinary disability allowances (ODAs)). Thus, there are not merely direct health care costs but also indirect costs.
According to international documents (WHO, WHA, and others), we strongly believe that it is crucial to analyse the socio-economic impact of epilepsy in Italy with a specific focus on hospital costs (hospitalizations), costs related to DPs, and ODAs. Following a systematic review of the literature (RSL), few studies have emerged concerning the economic impact of epilepsy in Italy. Of these, two refer to the costs for the treatment of drug-resistant epilepsy (2,3), another to the pharmacological treatment of epilepsy in children and adolescents (4), yet another estimated the direct costs for the treatment of refractory epilepsy (5), a latest study focused attention on the costs of co-morbidities and pharmaceutical expenditure (6). All these studies are also characterized, with the exception of the one on co-morbidities, by an important age of the data. Therefore, there is no current enhancement of the economic weight that weighs on the NHS in terms of hospitalizations but also an initial ‘investigation’ relating to the impact on the Italian social security system.
The main goal of this analysis, consequently, is to examine which costs, very recent, impact the most on the direct management of patients affected by epilepsy and to suggest new approaches to cope with these patients. We believe that it can be helpful to improve the effectiveness of health care intervention and the efficiency of the system (both NHS and social system).
The social security benefits analysis (DP and ODA) allows to understand the potential impact of increased disability due to epilepsy outside the ‘classic’ context (Silos budget approach) of the NHS. Indeed, the social security system, in case of injury or illness, recognizes the right for workers to be eligible for one of the mentioned benefits, depending on the degree of disability and whether they apply for it.
The ODA is designed for workers with a degree of disability of more than two-thirds (between 67% and 99%) whereas the DP is designed for workers recognized as totally disabled (100%).
Thus, an increase in DPs may be considered as a wake-up call for the decision maker because after the disease occurrence, a significant number of patients reach a level of full disability (100%). Such conditions no longer allow for recovery and permanently compromise all the patient’s own activities, resulting in increased productivity loss.
Before focusing on epilepsy from the point of view of the social security system, we believe that it is useful considering the positioning of the nervous system and sense organ diseases within the social security benefits framework. Thus, a preliminary analysis was conducted at the macro level referring to the period 2009-2015. The findings reveal that this grouping of diseases is located among the disease groups with the greatest impact as far as the social security system is concerned.
Regarding the number of recipients of Ordinary Allowances, the Diseases of the Nervous System constitute the fifth largest pathological group (32,000 recipients on average each year) whereas DPs constitute the third largest pathological group (11,400 recipients on average each year), following cancer and mental disorders with a significant and worrying upward trend.
With respect to costs, diseases of the nervous system and sense organs have an average annual expenditure, for ODAs and DPs, of about € 413 million (€ 267 million for ODAs and € 146 million for DPs, accounting for a total of € 2.9 billion over the period (Fig. 1)).
In the case of epilepsy, an average of about 800 applications were filed each year; in 60% of cases these applications were unsuccessful, in 29% of cases disability was recognized, and in 11% of cases total disability was recognized.
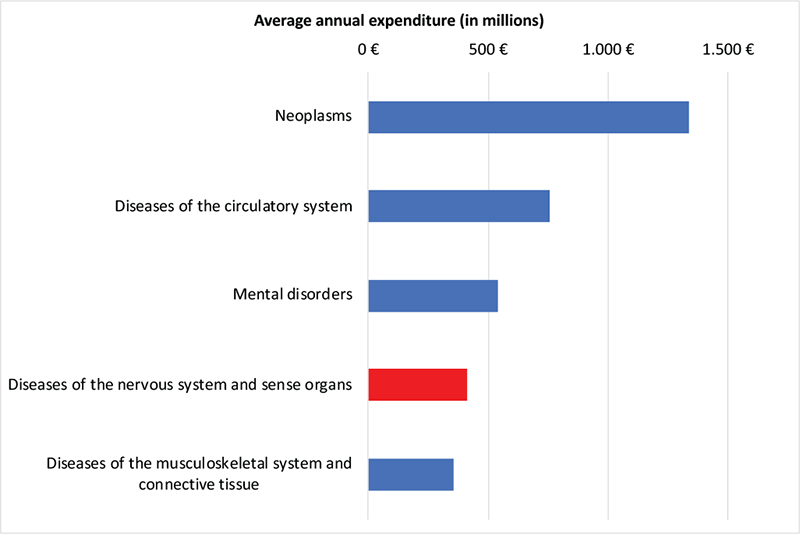
Fig. 1 - Average annual welfare spending (2009-2015).
In terms of beneficiaries, results reveal an average annual number of beneficiaries of 1,964 for ODAs and 620 for DPs (2,584 total). However, the most interesting and alarming finding is the trend recorded in the lifespan considered.
Indeed, between 2009 and 2015 (Fig. 2) it is possible to observe a decreasing trend for ODAs (−9%) unfortunately accompanied by an increasing trend for DPs (+26%). The findings should let us think, because an increase in DPs means an increase in the number of patients who, due to the disease, reach the highest level of disability (100%) with no possibility of recovery.
The trend in DPs is significantly alarming since it has an impact economically and socially. Indeed, substantial expanses must be supported throughout the patients’ lifetimes by both the social security system and the NHS without forgetting the impact on caregivers (out-of-pocket expenses and loss of productivity).
The costs for services analysed amounted to € 171 million in the period considered (an increase of 16%). As regards DPs, an increase of +40% was recorded. Thus, also with respect to costs, it is fundamental to monitor the trend of DPs and think about models that could be implemented in order to control this worrisome growth related to disability.
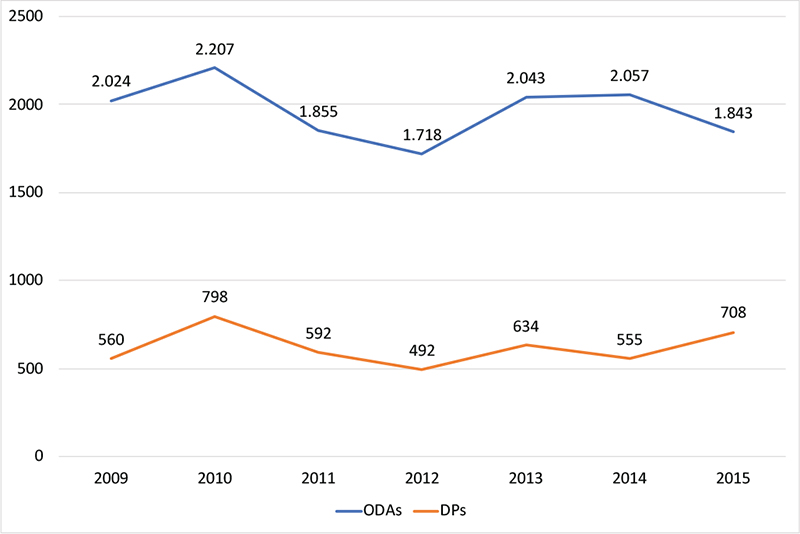
Fig. 2 - Estimated beneficiaries and trend (2009-2015).
Alongside the costs borne by the welfare system, with a specific reference to epilepsy, it is fundamental to analyse the economic burden at the hospital level. Indeed, international studies demonstrate that the greatest burden of epilepsy at the welfare level occurs precisely in hospitalizations. Hence, we analysed the hospital expenditure on epilepsy through the information available in the Hospital Discharge Cards (HDS). All the inpatient admissions with the principal diagnosis of epilepsy in the analysis period considered (2015-2018 – latest data available at the time of analysis) were selected, whereas for cost quantification, inpatient admissions were valued on the basis of the national fee schedule for hospital service remuneration.
The first finding that emerged from the analysis is one related to the distribution of admissions by both type of activity and regimen. With respect to the type of activity, it can be noticed (Figs. 3 and 4) that almost all admissions are acute (95%), followed by rehabilitation (4%) and long-term care (1%). Differently, the finding by hospitalization regimen infers that 76% are ordinary hospitalization, whereas the remaining 24% can be classified as day hospital.
The cost of acute and ordinary hospitalizations is undoubtedly the highest. Hence, reducing this cost item could be particularly important in terms of proper and efficient management of resources, especially considering that reductions in hospitalizations significantly improve the QoL of patients, generating a reduction in lost productivity.
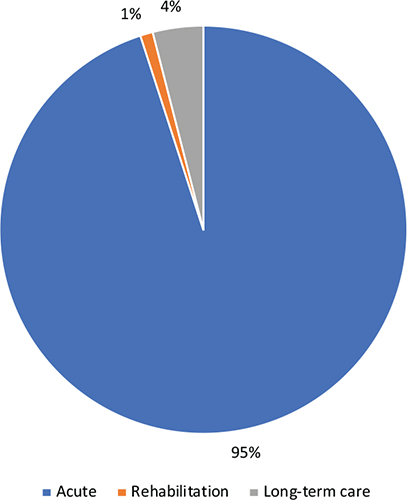
Fig. 3 - Distribution of total hospitalizations by type of activity.
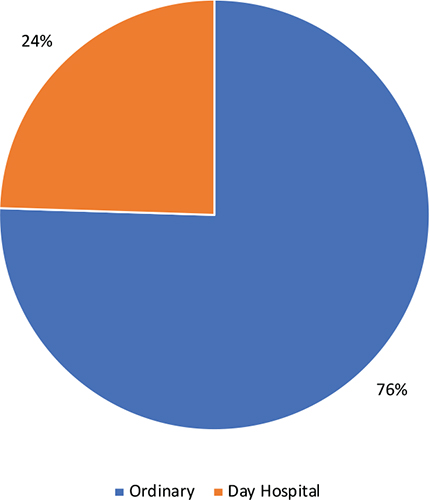
Fig. 4 - Distribution of total hospitalizations by inpatient regimen.
With specific reference to the total cost for hospitalization, the analysis reports a value of € 62 million in 2018 (the last year of analysis).
From the analysis of inherent hospitals and social security costs of epilepsy in Italy, it can be stated that the expense of hospitalizations should/could be reduced through the implementation of different organizational and management approaches. Furthermore, concerning epilepsy, we should bear in mind that, alongside the costs associated with hospitalization and those borne by the social security system, there are costs arising from co-morbidities which should be carefully analysed and considered.
If, then, we add to these costs those charged to pharmaceutical expenditure (more than € 300 million – OSMED Report), we can begin to better understand the magnitude of the problem both for the NHS and for the social system. But, the cost of co-morbidities must also be considered.
The co-morbidities of epilepsy can be identified as a meaningful burden for people affected by the disease, which should be carefully investigated to reduce not merely costs but also health consequences for patients. The number of co-morbid diseases tends to increase with age (7). The economic burden, in fact, varies considerably according to the severity of the disease (frequency of crises, co-morbidities). It is estimated that about 50% of adults with epilepsy have at least one other coexisting disease (8) and other studies report that the prevalence of some specific diseases is higher in people with epilepsy than in the general population (9). A recent analysis (6) calculated the costs due to co-morbidities. Specifically, patients with four or more co-morbidities show an average cost of approximately € 2,000, followed by those with two or three co-morbidities (approximately € 650). Patients who do not have co-morbidities are characterized by an average cost of € 380, highlighting once more how early management accompanied by effective treatments can not only improve patients’ QoL but also be accompanied by an important cost reduction.
According to recent studies (10), screening programmes and guidelines should be developed in order to disseminate the knowledge gained by effective and meaningful clinical interventions. In this way, it might be possible to reduce the economic and social burden of the disease and ensure early patient care. Besides, the policy maker could adopt new innovative treatments to improve effectiveness and, at the same time, reduce the expense of the NHS, of the social system as a whole, with an evident improvement in patients’ QoL.
However, it is fundamental to remind that through pharmaceutical treatments and surgery procedures we can control the disease 80% of the time with noteworthy positive implications on the social and health care system. Despite this awareness, reaching these results seems not to be straightforward, since they first require a change of perspective.
First and foremost, it is inevitable to think about the implementation of a different model in order to ensure an early diagnosis for patients and provide early access to drugs and/or surgery. Besides, there is the need to design homogeneous and shared diagnostic pathways (diagnostic, therapeutic, and assistance pathways [PDTAs]) throughout the country so as to achieve equal access to treatment combined with vertical equity in the welfare pathway.
After all, we believe that resources offered by the National Recovery and Resilience Plan (Piano Nazionale di Ripresa e Resilienza, PNRR) can represent a valid opportunity to implement such care pathways and incentivize the adoption of community-based care wherever possible. In addition, it could ensure better QoL for both patients and caregivers with a meaningful reduction in social costs and out-of-pocket spending.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Payment of publication fees was supported by Angelini Pharma S.p.A.
References
- 1. Epilessia. Istituto Superiore di Sanità; 2019. Online (Accessed June 2022).
- 2. Marras CE, Canevini MP, Colicchio G, et al; Commission on Epilepsy Surgery of the Italian League Against Epilepsy. Health Technology Assessment report on the presurgical evaluation and surgical treatment of drug-resistant epilepsy. Epilepsia. 2013;54(suppl 7):49-58. CrossRef PubMed
- 3. Marras CE, Colicchio G, De Palma L, et al. Health technology assessment report on vagus nerve stimulation in drug-resistant epilepsy. Int J Environ Res Public Health. 2020;17(17):6150. CrossRef PubMed
- 4. Beghi E, Capovilla G, Franzoni E, et al. Midazolam vs diazepam in prolonged seizures in children: a pharmacoeconomic approach. Acta Neurol Scand. 2018 Jan;137(1):24-28. CrossRef PubMed
- 5. Luoni C, Canevini MP, Capovilla G, et al. A prospective study of direct medical costs in a large cohort of consecutively enrolled patients with refractory epilepsy in Italy. Epilepsia. 2015;56(7):1162-1173. CrossRef PubMed
- 6. Lega Italiana contro l’epilessia. Libro Bianco dell’epilessia in Italia. UCB Pharma SpA, 2019. Online (Accessed May 2022).
- 7. Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23(7):455-468. CrossRef PubMed
- 8. Forsgren L. Prevalence of epilepsy in adults in northern Sweden. Epilepsia. 1992;33(3):450-458. CrossRef PubMed
- 9. Gaitatzis A, Sisodiya SM, Sander JW. The somatic comorbidity of epilepsy: a weighty but often unrecognized burden. Epilepsia. 2012;53(8):1282-1293. CrossRef PubMed
- 10. Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol. 2016;15(1):106-115. CrossRef PubMed