 |
Glob Reg Health Technol Assess 2020; 7(1): 139-147 DOI: 10.33393/grhta.2020.2028 ORIGINAL RESEARCH ARTICLE |
 |
Factors influencing short-term effectiveness and efficiency of the care provided by Dutch general practice mental health professionals
ABSTRACT
Introduction: This study examined whether factors related to general practice mental health professionals (GP-MHPs), that is, characteristics of the professional, the function, and the care provided, were associated with short-term effectiveness and efficiency of the care provided by GP-MHPs to adults in Dutch general practice.
Methods: A prospective cohort study was conducted among 320 adults with anxiety or depressive symptoms who had an intake consultation with GP-MHPs (n = 64). Effectiveness was measured in terms of change in quality-adjusted life years (QALYs) 3 months after intake; and efficiency in terms of net monetary benefit (NMB) at 3-month follow-up. A range of GP-MHP-related predictors and patient-related confounders was considered.
Results: Patients gained on average 0.022 QALYs at 3-month follow-up. The mean total costs per patient during the 3-month follow-up period (€3,864; 95% confidence interval [CI]: €3,196-€4,731) decreased compared to that during the 3 months before intake (€5,220; 95% CI: €4,639–€5,925), resulting largely from an increase in productivity. Providing mindfulness and/or relaxation exercises was associated with QALY decrement. Having longer work experience as a GP-MHP (≥2 years) and having 10-20 years of work experience as a mental health care professional were negatively associated with NMB. Furthermore, a higher number of homework exercises tended to be related to less efficient care. Finally, being self-employed and being seconded from an organization in which primary care and mental health care organizations collaborate were related to a positive NMB, while being seconded from a mental health organization tended towards such a relationship.
Conclusions: Findings seem to imply that the care provided by GP-MHPs contributes to improving patients’ functioning. Some GP-MHP-related characteristics appear to influence short-term effectiveness and efficiency of the care provided. Further research is needed to confirm and better explain these findings and to examine longer-term effects.
Keywords: Costs, General practice mental health professionals, Mental disorders, Net benefit, Netherlands, Quality-adjusted life year
Received: January 30, 2020
Accepted: May 13, 2020
Published online: December 14, 2020
© 2020 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Any commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Depression and anxiety are common mental disorders and accountable for large reductions in overall health. Approximately one out of five Dutch adults will experience a depressive disorder (20.2%) at some point in their lives. The same holds true for anxiety disorder (19.6%) (1). Depression is ranked as the single largest contributor to global disability (7.5% of all years lived with disability in 2015); anxiety disorders are ranked sixth (2). Besides their health impact, these common mental disorders cause a significant economic burden due to lost economic output and their comorbidity with costly medical conditions (3). Consequently, prevention of depression and anxiety is recognized as a major public health challenge (4).
Strengthening mental health care in the primary care setting is considered vital for achieving more effective and efficient preventive mental health care (5). In 2014, the Dutch government introduced reforms of the mental health care system to enable substitution of secondary mental health care by primary mental health care. The aim was to realize better cost control of mental health care, while at the same time improving the accessibility and quality of care (6). Since the reform, the proportion of general practices employing a general practice mental health professional (GP-MHP; a function introduced in 2008) has dramatically increased: from 20% in 2010 to 90% in 2015 (7). Together with the general practitioner (GP), the GP-MHP acts as the gatekeeper to more specialized mental health care facilities. The GP-MHP supports the GP in the care for patients with common mental health problems, such as depressive and anxiety symptoms. The GP-MHP provides support, guidance, and short-term treatment and aims to prevent the development of full-blown mental disorders that require referral to more specialized mental health care. The number of adults consulting a GP-MHP increased significantly in recent years, from almost 427,000 in 2015 to 536,000 in 2018 (8).
Given the crucial role of GP-MHPs in strengthening mental health care in Dutch general practice, it is important to gain insight into the effectiveness and efficiency of the care they provide and their relevant factors (9, 10). In this perspective, factors related to the professional GP-MHP, the function, and the care provided are relevant to examine. As different professions can fulfill the function (11), GP-MHPs’ educational backgrounds differ, including psychology, social psychiatric nursing, and social work. Moreover, some GP-MHPs pursued a postbachelor’s training, while others have not. Other characteristics that vary among GP-MNPs include gender, age, and working experience. As the function is relatively new and developing, substantial variation exists in its organization in daily practice (6), such as the collaboration between GP-MHP and GP, and type of employment arrangement. Some GP-MNPs are employed by a general practice, while others are self-employed or seconded from organizations such as primary care or mental health care organizations (9). Previous research has also indicated variation in the care provided by GP-MHPs in terms of the average number of consultations per patient and referral behavior (6).
The current exploratory study aims to determine whether GP-MHP-related factors, that is, characteristics of the professional, the function, and the care provided, are associated with short-term (3-month) effectiveness and efficiency of the care provided by GP-MHPs to adult patients with anxiety or depressive symptoms. Identifying influencing GP-MHP-related characteristics is relevant to further develop the function and to promote effective mental health care in general practice at reasonable costs.
Methods
Study design and population
A prospective cohort study was conducted in which adults with anxiety or depressive symptoms and who had an intake consultation with a GP-MHP (January 2018-March 2019) were followed up for 3 months. This study was part of a larger study on the quality of care provided by GP-MHPs.
Participating GP-MHPs
To ensure variation among participating GP-MHPs, purposive sampling was performed based on type of employment arrangement (i.e., employed by a general practice, self-employed, or seconded from an organization, such as a primary care or a mental health care organization). From the beginning of 2017, GP-MHPs were recruited via seven local/regional organizations located throughout central Netherlands and representing the different employment types. Additional recruitment took place via the National Association of GP-MHP (LV POH-GGZ). To ensure that sufficient patients participated, additional GP-MHPs were recruited (Fall 2018-Spring 2019) via two additional organizations (one was located in the northeast of the Netherlands) and a call on social media sites of the Trimbos Institute. Eventually, 64 GP-MHPs were included in this study, each of whom recruited one or more participating patients.
Participating patients
Patient eligibility criteria were: being at least 18 years old; having an intake consultation with the GP-MHP; presenting with depressive, anxiety, or distress complaints; having not received mental health care in the past 12 months according to the GP-MHP; expecting to have at least two follow-up consultations according to the GP-MHP; having sufficient knowledge about the Dutch language and cognitive skills to fill in questionnaires; and having access to the Internet. Online study-related information was provided to interested patients such that they were able to make a well-considered decision whether to participate.
Figure 1 shows that 483 patients consented to participate and completed questionnaires within 2 weeks after the intake consultation (baseline measurement, T0). Of these, 376 patients (77.8%) completed the questionnaires at 3-month follow-up (T1). A nonresponse analysis revealed no differences between respondents and nonrespondents at T1 regarding their baseline characteristics. Our study examined effectiveness and efficiency of the care provided by GP-MHPs. Therefore, patients who were referred to (more) specialized mental health care (n = 45) or who did not receive care from the GP-MHP (n = 11) were excluded, resulting in a study population of 320 patients.
Measures
Both at T0 and T1, patients completed questionnaires on sociodemographics, anxiety and depressive symptoms, quality of life, health care consumption, and productivity losses. Furthermore, GP-MHPs completed a questionnaire about their background characteristics and the organization of their function in daily practice. Also, after every consultation with a participating patient, GP-MHPs recorded characteristics of the care provided.
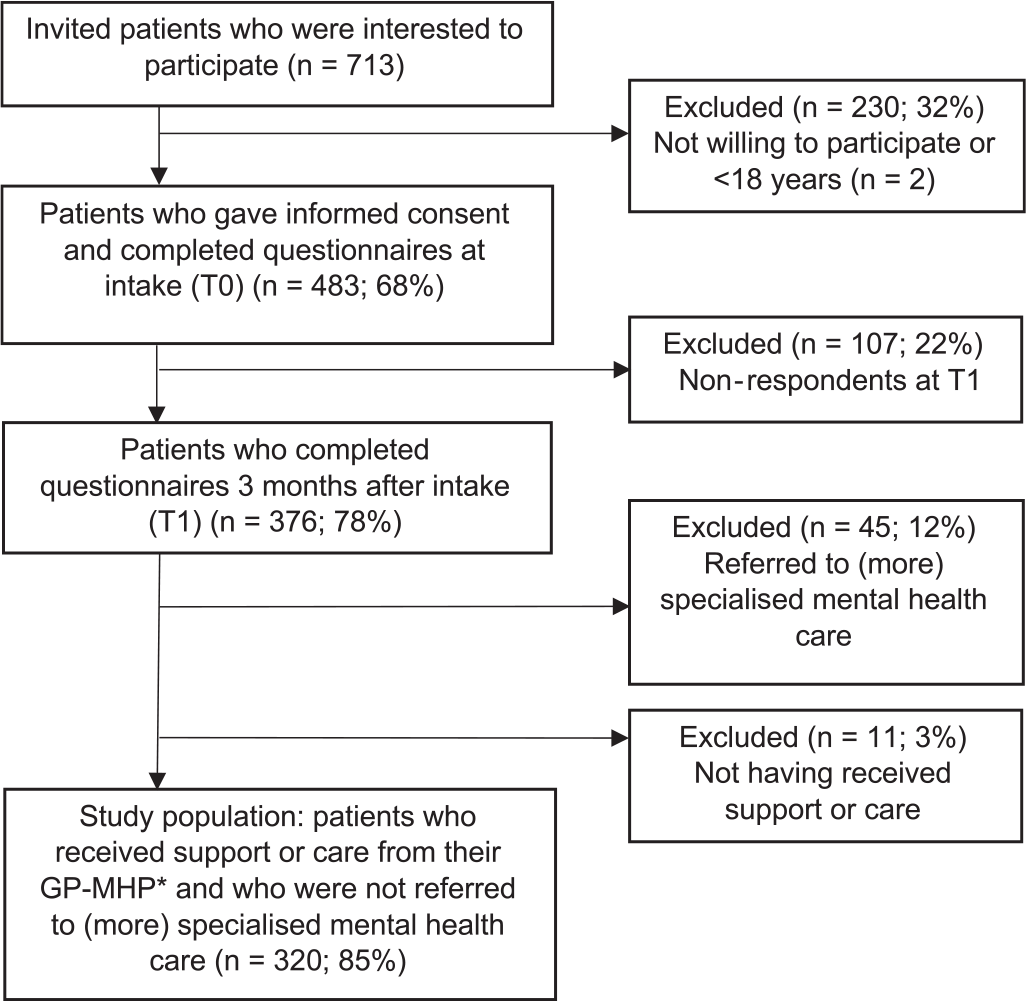
*Patients who had at least two consultations with a general practice mental health professional (GP-MHP) and who received psychological education (guidance and advice), short-term self-help/psychological guidance, relapse prevention, and/or monitoring/long-term guidance during at least one consultation.
Dependent variables
Change in QALYs
According to the guidelines for economic evaluations in health care provided by Care Institute Netherlands (12), the EuroQol questionnaire (EQ-5D-5L) has been used to calculate (changes in) health-related quality of life in terms of quality-adjusted life years (QALYs). The Dutch tariff for the EQ-5D-5L has been used to compute utilities (13). The change in QALYs was calculated by the area-under-the-curve (AUC) method using the utilities at T0 and T1. The change in QALYs ranged between −0.25 and 0.25 given that this is the maximum possible change in 3 months. A negative value indicated a deterioration of a patient’s quality of life at 3-month follow-up, while a positive value indicated an improvement.
Costs
The commonly used and validated questionnaire Treatment Inventory of Costs in Patients with psychiatric disorders (TIC-P) (14) was used to measure the health care consumption and productivity losses for participating patients in the past 3 months, both at T0 and T1. Information about the number and type of GP-MHP consultations was recorded by GP-MHPs for each patient.
The following types of costs were distinguished: health care costs, productivity costs, and patient and family costs (e.g., transportation costs). The Dutch manual for economic evaluation in health care (12) was followed. The reference prices of the Dutch manual were combined with the information obtained from the TIC-P to determine costs. Due to the lack of available reference prices, cost prices of the GP-MHP consultations were obtained from insurance tariffs (15). Psychotropic medication costs were calculated by multiplying number of daily defined dosages (16) by the average prices (17). Absenteeism costs were defined as the days absent from work multiplied by the productivity cost of a paid worker per hour and the average working hours per day. Presenteeism costs were defined as less productive days multiplied by the productivity loss in these days, the productivity costs of a paid worker per hour, and the average daily working hours. Patient and family costs consisted of informal care and transportation costs. Informal care costs were defined as the time and associated costs a family member would be working on the unpaid work when the patient was not able to do this by themselves and was valued using the average wage of housekeeping as defined in the Dutch guideline for economic evaluations. All costs were expressed in Euros and converted to the price year 2018.
Net monetary benefit
Net monetary benefit (NMB) was calculated by subtracting the costs per patient from the benefits ([change in QALYs × willingness-to-pay (WTP) threshold] – costs). The gain in QALYs was converted to monetary values to determine the “benefit.” In the Netherlands, the WTP for preventive interventions is often cited as €20,000 per QALY (18). Our study focused on patients with anxiety or depressive symptoms who received care from a GP-MHP. This can be considered preventive care aimed at preventing the development of full-blown mental disorders. Therefore, a gain of one QALY was set conservatively at €20,000.
Potential predictors of variation in outcomes
Characteristics of the professional and function GP-MHP
Given that several characteristics were considered, an expert panel (consisting of two GP-MHPs, one GP, one representative of a patient organization, and three researchers) selected a priori characteristics that were essential from a policy perspective to be included in analyses: having a nursing background; pursuing or having completed a GP-MHP postbachelor’s training; years of work experience as a GP-MHP; having 10 or more consultations on an average 8-hour working day; and being seconded (irrespective from which organization). Besides these variables, the following characteristics were considered by a statistical selection procedure: age; gender; years of work experience in a mental health profession; number of working hours per week as a GP-MHP; having regular consultation moments with the GP; having a short average waiting time (<2 weeks); using questionnaires always or often to support problem clarification or triage; using questionnaires always or often to monitor outcomes; having received sufficient continuing training (≥20 hours) in the previous 12 months; and having received sufficient peer consultation and/or supervision (≥6 times) in the previous 12 months.
Characteristics of the care provided
The following characteristics as recorded by the GP-MHPs were considered: number of consultations, number of homework exercises, and treatment technique(s) provided during consultations. The following treatment techniques were distinguished: cognitive behavioral therapy techniques; behavioral activation; guided self-help care to improve coping and mental health; mindfulness or relaxation exercises; and solution-oriented or problem-solving treatment. No care characteristics were selected a priori.
Potential patient-related confounders
The following baseline patient characteristics were considered: age, gender, education, living situation, working situation, ethnic origin, and severity of anxiety and depressive symptoms. The widely used and validated questionnaires Generalized Anxiety Disorder (GAD-7) and Patient Health Questionnaire on Depression (PHQ-9) were used to measure severity of anxiety and depressive symptoms, respectively (19). A priori selected characteristics included age, gender, and GAD-7 and PHQ-9 scores.
Statistical analyses
Selection of potential predictors and confounders
Additionally, to a priori selection, a statistical procedure was conducted to select potential predictors and confounders. This procedure removed variables that were redundant and unlikely to add any significant information to the final model using the Least Absolute Shrinkage and Selection Operator (LASSO). LASSO is a regression analysis that performs regularization and variable selection in which a constraint is put on the sum of the absolute values of the model parameters (20). Separate models were run for change in QALYs and NMB per patient. The LASSO models were optimized using fivefold cross-validation in which the data were split into five subsets from which one was used as the test set and the other four were used for building a model. This procedure was repeated iteratively five times to choose the best fitting model. The LASSO regressions were performed with statistical software R version 3.5.2.
Main analyses
Regression models were used to examine the associations of selected GP-MHP-related characteristics with change in QALYs and NMB, while controlling for selected patient-related confounders. Clustered standard errors at the GP-MHP level were used to control for correlation between standard errors of patients treated by the same GP-MHP. Given the relatively low number of missing values, missing data were imputed using median imputation for numerical variables and an “unknown” category was added for categorical variables. Nonparametric stratified bootstrapping (1,000 replications) was performed to calculate 95% confidence interval (CI). Analyses were performed with STATA 12.0. Given the explorative nature of our study and the relatively small sample size, alpha levels were set at 0.1. If a p value was less than 0.05, a result was considered significant; and if a p value was less than 0.1, a result was considered borderline significant.
Sensitivity analyses
Main analyses were repeated: (a) while excluding patients who reported at T0 to have received mental health care utilization in the previous 3 months (n = 93); (b) while excluding patients with minimal anxiety and depressive symptoms at T0 (i.e., GAD-7 and PHQ-9 scores: ≤4) (n = 38); and (c) when taking a health care perspective (i.e., exclusion of productivity losses and patient and family costs).
Results
Characteristics of study population
Table I shows that considerable variation existed among the 64 GP-MHPs regarding measured characteristics, such as working experience, number of working hours per week, and employment arrangement. The number of patients per GP-MNP was on average 5 and ranged from 1 to 15. The GP-MNPs had a mean age of 51.2 years and were predominantly female.
Table II presents baseline patient characteristics. The patients were predominantly 30 years or older (73.7%), female (69.4%), married or living with a partner (66.7%), employee or entrepreneur (74.1%), and of Dutch origin (86.6%). The majority of the patients experienced mild to moderate severe anxiety (69.7%) and/or depressive (63.1%) symptoms.
Selected potential predictors and confounders
In addition to a priori selected predictors and confounders, the LASSO method selected number of working hours per week as a GP-MHP, using mindfulness and/or relaxation exercises by the GP-MHP and patient’s educational level for the model predicting change in QALYs (see supplementary table I). Work experience as a mental health care professional, using questionnaires always or often to monitor outcomes, number of homework exercises, patient’s work situation, and patient’s living situation were additionally selected for the model predicting NMB.
Change in QALYs
Patients gained on average 0.022 QALYs at 3-month follow-up (range: −0.10 to 0.22) (see Tab. IV). As shown in Table V, patients who were offered mindfulness and/or relaxation exercises demonstrated a QALY decrement compared to patients who received other treatment techniques. Other selected GP-MHP-related characteristics exerted no (borderline) significant effect. Of the selected patient-related confounders, more severe baseline anxiety symptoms were associated with a positive change in QALYs, while more severe depressive symptoms tended toward such an association.
| %, – (range) | |
|---|---|
| Female gender | 68.8 |
| Age | 51.2 (33–63) |
| <45 | 18.7 |
| 45–55 | 46.9 |
| ≥55 | 34.4 |
| Nursing background | 73.4 |
| GP-MHP postbachelor’s training degree (in progress or completed) | 59.4 |
| Mean work experience as a mental health care professional in years (range) | 22.3 (1–41) |
| Mean working experience as a GP-MHP in years (range) | 4.9 (0–14) |
| <2 | 18.8 |
| 2–4 | 29.7 |
| 4–8 | 35.9 |
| ≥8 | 15.6 |
| Working hours per week as a GP-MHP | 24.1 (6-40) |
| <16 | 15.6 |
| 16–28 | 45.3 |
| ≥28 | 39.1 |
| Number of consultations on an average 8-hour working day | 9.1 (4–15) |
| <10 face-to-face consults | 56.2 |
| ≥10 face-to-face consults | 43.8 |
| Employment arrangement | |
| Employed by a general practice or self-employed | 34.4 |
| On a secondment basis | 65.6 |
| Regular consultation moments with GP | 53.1 |
| Average waiting time for new patients | |
| <2 wk | 60.9 |
| ≥2 wk | 39.1 |
| Using questionnaires always or often to support problem clarification or triage
Always or often |
54.7 |
| Using questionnaires always or often to monitor outcomes | 20.3 |
| Having received ≥20 h of continuing training (in the previous 12 mo) | 67.2 |
| Having received ≥6 times peer consultation or supervision (in the previous 12 mo) | 76.6 |
GP-MHP = general practice mental health professional.
Net monetary benefit
Costs
The mean total costs per patient were €5,220 in the 3-month period before intake consultation with the GP-MHP, and €3,864 in the 3-month follow-up period (Tab. III), resulting in a mean decrease of €1,356 per patient. This was mainly explained by decreases in mean productivity costs (€1,018) and patient and family costs (€286). Patient and family costs decreased mainly due to a decrease in unpaid work costs (€285).
| %, – (range) | Missing | |
|---|---|---|
| Female gender | 69.4 | |
| Age at intake (years) | 41.9 (18–72) | 1 |
| 18–29 | 26.3 | |
| 30–44 | 33.2 | |
| 45–59 | 26.7 | |
| ≥60 | 13.8 | |
| Living situation | ||
| Married or living with a partner | 66.9 | |
| Other (single, divorced, widow) | 33.1 | |
| Educational level* | ||
| Low | 8.4 | |
| Middle | 52.2 | |
| High | 39.4 | |
| Working situation | 11 | |
| Employee or entrepreneur | 74.1 | |
| Disabled or unemployed | 9.1 | |
| Other (housewife/man, school, retirement) | 16.8 | |
| Ethnicity | ||
| Dutch | 86.6 | |
| Migration background† | 13.4 | |
| Severity of anxiety symptoms‡ | 8.4 (0–20) | |
| Minimal (0–4) | 19.4 | |
| Mild (5–9) | 42.8 | |
| Moderate (10–14) | 26.9 | |
| Severe (15–21) | 10.9 | |
| Severity of depressive symptoms¶ | 9.4 (0–27) | |
| Minimal (0–4) | 19.1 | |
| Mild (5–9) | 36.6 | |
| Moderate (10–14) | 26.6 | |
| Severe (15–27) | 17.8 |
*Low: less than primary education, primary education, lower secondary education. Middle: higher secondary education, lower vocational education. High: higher vocational education, university.
†Migration background: a patient was born abroad, or at least one of the patient’s parents was born abroad.
‡Based on Generalized Anxiety Disorder scale (GAD-7).
¶Based on Patient Health Questionnaire (PHQ-9).
Net monetary benefit
A positive NMB indicates that benefits were larger than the costs, and vice versa. The descriptive statistics of NMB are shown in Table IV. Table V shows that GP-MHPs with longer work experience (≥2 years) offered less efficient care than GP-MHPs with less than two years work experience. Also, the care of GP-MHPs with 10 to 20 years of work experience as a mental health care professional was less efficient compared to the care of GP-MHPs with less than 10 years of work experience. Furthermore, GP-MHPs who were seconded provided more efficient care than GP-MHPs who were employed by a general practice or self-employed. Finally, a higher number of homework exercises tended to be related to a negative NMB. Regarding the selected patient-related confounders, older age of patients tended to be associated with a negative NMB. Moreover, care provided to patients who were not an employee or entrepreneur was more efficient than that offered to employees and entrepreneurs. Finally, more severe baseline depressive symptoms were negatively associated with NMB, whereas more severe baseline anxiety symptoms showed a positive relationship.
| Mean costs during 3 months before intake | Mean costs during 3-month follow-up | |
|---|---|---|
| n = 320 | n = 320 | |
| Health care costs | ||
| Clinical consultation | ||
| General practitioner | 167.5 | 107.5 |
| Social worker | 14.7 | 16.6 |
| Physiotherapist | 53.1 | 57.3 |
| Psychologist | 46.2 | 68.0 |
| Outpatient clinic specialist | 42.4 | 38.2 |
| Addiction consultant | 0.0 | 0.3 |
| Occupational therapist | 20.5 | 45.9 |
| Total clinical consultations [95% CI] | 344.4 [311.4-387.0] | 333.9 [298.3-370.1] |
| GP-MHP consultation | ||
| Face-to-face consultation | ||
| Intake | 17.4* | |
| Short consult (<20 min) | 2.9* | |
| Long consult (>20 min) | 5.7* | |
| Home visit (<20 min) | 4.3* | |
| Home visit (>20 min) | 7.1* | |
| Other (call, mail, feedback, group) | 1.5* | |
| Total GP-MHP costs [95% CI] | 38.8 [35.2-42.5]* | |
| Other health care cost | ||
| Day/night treatment hospital or mental health care center | 25.0 | 30.8 |
| Psychotropic medication | 41.5 | 41.8 |
| Total other health care costs [95% CI] | 66.5 [43.7-98.1] | 71.6 [43.0-124.6] |
| Total health care costs [95% CI] | 410.9 [364.9-459.6] | 442.7 [391.3-507.3]* |
| Productivity costs | ||
| Absenteeism | 3,277.4 | 2,795.9 |
| Presenteeism | 887.0 | 350.3 |
| Total productivity costs [95% CI] | 4,164.3 [3,629.3-4,767.5] | 3,146.2 [2,569.8-3,862.4] |
| Patient and family costs | ||
| Unpaid work | 622.1 | 337.1 |
| Transport costs | 22.3 | 21.5 |
| Total patient and family costs [95% CI] | 644.5 [499.3-817.3] | 358.6 [267.2-470.4] |
| Total costs per patient [95% CI] | 5,219.7 [4,639.1-5,925.7] | 3,863.7 [3,196.0-4,731.2]* |
CI = confidence interval; GP-MHP = general practice mental health professional.
*27 missing observations.
| Dependent variables | n | Mean | Min | Q1 | Q2 | Q3 | Max |
|---|---|---|---|---|---|---|---|
| ΔQALY change* | 320 | 0.022 | −0.102 | 0 | 0.018 | 0.039 | 0.219 |
| NMB† | 293 | –3,421.02 | −80,507.46 | –3,774.26 | –518.63 | 146.09 | 3,282.59 |
Descriptive statistics of study observations.
NMB = net monetary benefit; QALY = quality-adjusted life year.
*Change in quality of life in 3 months.
†NMB in 3 months. The 27 missing observations resulted from the missing cost values.
| ΔQALY change | NMB | |
|---|---|---|
| Characteristics of the professional and function GP-MHP | ||
| Nursing background | 0.005 (0.005) | 632.88 (857.83) |
| GP-MHP post-bachelor’s training degree (in progress/completed) | 0.005 (0.004) | −234.25 (567.60) |
| Work experience as a GP-MHP | ||
| <2 years | Reference | Reference |
| 2−4 years | −0.004 (0.005) | −2037.34** (897.75) |
| 4−8 years | −0.002 (0.005) | −2882.94*** (923.75) |
| ≥8 years | −0.012 (0.007) | −3675.57*** (1032.16) |
| Work experience as a mental health care professional | ||
| <10 years | Reference | |
| 10−20 years | −2580.11** (1205.17) | |
| 20−30 years | −585.25 (1362.35) | |
| ≥30 years | −1322.22 (1249.68) | |
| Working hours per week as a GP-MHP | ||
| <16 hours | Reference | |
| 16−28 hours | −0.008 (0.008) | |
| ≥28 hours | 0.001 (0.007) | |
| Employment arrangement | ||
| Employed by a general practice or self-employed | Reference | Reference |
| Employed on a secondment basis | 0.002 (0.004) | 1872.71** (752.16) |
| Number of consults on an average 8-hour workday | ||
| <10 face to face consults | Reference | Reference |
| ≥10 face to face consults | 0.002 (0.004) | −755.62 (653.19) |
| Using questionnaires to monitor outcomes | ||
| Sometimes/rarely/never | Reference | |
| Always/often | −826.73 (744.97) | |
| Characteristics of the care provided | ||
| Number of homework exercises† | −279.35* (164.00) | |
| Other treatment | Reference | |
| Mindfulness/relaxation exercises | −0.009** (0.004) | |
| Unknown† | −0.009 (0.007) | |
| Baseline patient characteristics | ||
| Age | −0.000 (0.000) | −56.92* (33.27) |
| Female gender | −0.001 (0.004) | 474.77 (777.95) |
| Educational level | ||
| Low | Reference | |
| Middle | 0.014 (0.010) | |
| High | 0.006 (0.011) | |
| Working situation | ||
| Employee or entrepreneur | Reference | |
| School, housewife/man or retired | 3022.42*** (591.48) | |
| Disabled or unemployed | 3624.13*** (574.08) | |
| Unknown‡ | 2138.87 (1571.35) | |
| Living situation | ||
| Other | Reference | |
| Living together/married | −737.82 (603.36) | |
| Severity of anxiety symptoms (GAD-7) | 0.002** (0.001) | 192.77** (86.81) |
| Severity of depressive symptoms (PHQ-9) | 0.001* (0.001) | −326.10*** (84.97) |
| Constant | −0.011 (0.015) | 2868.15* (1460.14) |
| N | 320 | 320 |
| N-clusters | 64 | 64 |
| R-squared | 0.184 | 0.166 |
GAD = Generalized Anxiety Disorder; GP-MHP = general practice mental health professional; NMB = net monetary benefit; PHQ = Patient Health Questionnaire; QALY = quality-adjusted life year.
* p < 0.1. Robust standard errors in parentheses, clustered at the GP-MHP level, ** p < 0.05, *** p < 0.01.
† 27 missing observations
‡ 11 missing observations
Sensitivity analyses
In the first sensitivity analyses, patients who reported mental health care utilization in the 3 months before intake consultation with the GP-MHP were excluded (n = 93). Results showed that providing mindfulness and/or relaxation exercises was no longer negatively associated with change in QALYs at 3-month follow-up (supplementary tables II and III). More severe baseline anxiety and depressive symptoms remained associated with a positive change in QALYs. A new finding was that patients with middle or high levels of education tended to show QALY improvement compared to those with a low educational level. Regarding the model predicting NMB, results were largely robust. Compared to the original analysis using the total study population, a new finding was that the other categories of long work experience (20–30; and ≥30 years) as a mental health care professional also were/tended to be negatively associated with NMB, while number of homework exercises had no longer a borderline effect.
In the second sensitivity analyses, patients with minimal baseline anxiety and depressive symptoms were excluded (n = 38). Regarding the model predicting change in QALYs, the effects of offering mindfulness and/or relaxation techniques and baseline severity of anxiety and depressive symptoms remained. The sensitivity analysis predicting NMB also identified the same GP-MHP-related characteristics and patient-related confounders as the original analysis using the total study population.
When performing the NMB regression from a health care perspective (i.e., exclusion of productivity losses and patient and family costs), the only remaining significant predictor was patients’ severity of anxiety symptoms at baseline (supplementary table IV), which was also shown to be a strong predictor of gain in QALYs at follow-up in the base case analyses. Given that the difference in costs between baseline and follow-up diminishes when taking a health care perspective, it is not surprising that results of this analysis more closely resemble the results of the QALY analysis.
Discussion
The study explored whether GP-MHP-related characteristics influence short-term effectiveness (in terms of change in QALYs) and efficiency (in terms of NMB) of the care provided by GP-MHPs to adult patients with anxiety or depressive symptoms in Dutch general practice. First, the QALY results are discussed, followed by the NMB results.
Receiving mindfulness and/or relaxation exercises was associated with a QALY decrement as compared to receiving other treatment techniques. This may indicate that mindfulness and/or relaxation techniques were offered relatively frequently to more complex patients who are less likely to recover within 3 months, or that these techniques are relatively less effective in the short term. Regarding patient-related characteristics, having more severe anxiety and/or depressive symptoms at baseline was, or tended to be, associated with a QALY improvement. These findings may reflect that patients in a more severe baseline (mental health) state have more room for improvement.
Having longer work experience (≥2 years) as a GP-MHP was associated with less efficient care. Also, having longer work experience (10-20 years) as a mental health professional was related to a negative NMB. Possibly, more complex patients, who are less likely to recover within 3 months and more likely to incur higher costs during this period, are perceived as intrinsically challenging by more experienced GP-MHPs, leading to the decision to treat these patients rather than referring them to (more) specialized mental health care. Furthermore, GPs may be less hesitant to refer more complex patients to more experienced GP-MHPs. Indeed, post hoc analyses revealed that the patients of GP-MHPs with longer work experience (i.e. 2-4; 4-8; and ≥8 years) had lower baseline utilities (resp. 0.74; 0.74; and 0.71) and higher costs during 3-month follow-up (resp. €3,193; €4,332; and €5,913) than the patients of GP-MHPs with little work experience (<2 years) (baseline utility: 0.78; costs: €2,629). The finding that the number of homework exercises tended to be negatively related to NMB might also be explained in terms of complexity of patients: it is likely that more complicated problems require a higher number of homework assignments.
Being seconded rather than being employed by a general practice or being self-employed exerted a positive effect on NMB, suggesting more efficient care. To better interpret this finding, a post hoc analysis was performed in which type of employment arrangement was further categorized (reference category: employed by a general practice) (supplementary table V). Being self-employed and being seconded from an organization in which primary care and mental health care organizations collaborate were associated with a positive NMB compared to being employed by a general practice, while being seconded from a mental health organization tended towards such a relationship. This may suggest that these types of employment arrangement promote collaboration and timely referral between professionals working in general practice and mental health care. Several patient-related confounders were related to NMB. Older age of patients tended to show a negative association, which is understandable given that older patients encounter higher costs. Additionally, unemployed patients had a higher NMB than employed patients, which is expected since only the latter incur productivity losses. Finally, more severe baseline depressive symptoms were associated with costs that increasingly outweighed the benefits (based on QALY gain), whereas greater baseline anxiety symptoms were related to benefits that increasingly outweighed the costs.
Sensitivity analyses excluding patients with minimal baseline anxiety and depressive symptoms showed similar results. Also, when excluding patients who reported mental health care utilization in the 3 months before intake consultation with the GP-MHP (n = 93), most of the identified predictors remained (borderline) significant (except for the negative effect of receiving mindfulness and/or relaxation exercises on QALYs). This suggests that results are largely robust to these changes in study population.
Study strengths include the prospective design, the use of established patient questionnaires, and the wide range of potential GP-MHP-related characteristics and patient-related confounders considered. Yet, some limitations merit discussion. First, given the exploratory nature of the study without a control condition, no causal inferences can be drawn. Second, the GP-MHPs may be unrepresentative of the population. However, they were comparable to members of the LV POH-GGZ in terms of age, gender, and work experience. Third, it is possible that patients in a better mental health state were more likely to participate since other patients may have preferred to focus solely on recovery, leading to a study population in which more severe patients were underrepresented. Fourth, almost 30% of the patients reported recent use of mental health care at baseline. This exclusion criterion could have been overlooked by a GP-MHP, or a patient did not report this to the GP-MHP when invited for participation. Fifth, the registration of GP-MHPs about the characteristics of the care provided to participating patients may be incomplete. Sixth, the sensitivity of the EQ-5D-5L to detect changes could be questioned given its generic character and ceiling effects demonstrated in other studies (21,22). Seventh, the WTP for one QALY was set relatively low (equal to the WTP for preventive interventions). Possibly, the disease burden associated with early stages of depressive and anxiety disorders is higher. The conservative WTP would have made it harder to detect significant positive effects on NMB. Lastly, this study focused on a short-term 3-month follow-up. It is important to study longer-term effects to see if improvements in QALYs and reductions in resource utilization are sustainable.
In conclusion, this study showed that the mean quality of life of adult patients with anxiety or depressive symptoms improved at 3 months after intake consultation with the GP-MHP. Furthermore, the mean total costs per patient during the 3-month follow-up period decreased compared to the 3 months before intake, resulting largely from an increase in productivity. These findings seem to imply that the care provided by GP-MHPs contributes to improving patients’ functioning. Some GP-MHP-related characteristics appear to influence short-term effectiveness and efficiency of the care provided. Further research is needed to confirm and better explain these findings and to examine longer-term effects.
Disclosures
Financial support: This study was funded by the Netherlands Organization for Health Research and Development (ZonMw), grant application number 50-53120-98-020. This study has been approved by the internal Ethics Committee of the Trimbos Institute, Utrecht, The Netherlands.
Conflict of interest: Audry Kenter is working as a GP-MHP, but has no further conflicts of interest. Likewise, all other authors have nothing to declare.
References
- 1. de Graaf R, ten Have M, van Dorsselaer S. De psychische gezondheid van de Nederlandse bevolking. Utrecht: Nemesis-2: Opzet en eerste resultaten, Trimbos Instituut (Netherlands Institute of Mental Health and Addiction) 2010.
- 2. WHO. Depression and other common mental disorders: global health estimates. 2017.
- 3. Mnookin S, Kleinman A, Evans T. Out of the shadows: making mental health a global development priority. Washington, DC: World Bank Group 2016.
- 4. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiat. 2016;3(2):171-178.
- 5. WHO. Integrating mental health into primary care: a global perspective. Geneva: World Health Organization 2008.
- 6. Trend repport GGZ. Versterking van de GGZ in de huisartsenpraktijk. Terugblik, stand van zaken en vooruitblik. Utrecht: Timbos Instituut (Netherlands Institute of Mental Health and Addiction) 2014.
- 7. Magnée T, Schellevis FG, Verhaak PF. Developments in mental health care in Dutch general practices: an overview of recent studies. Tijdschr Psychiatr. 2019;61(2):126-134.
- 8. Vektis. Zorgthermometer Inzicht in de GGZ. Zeist: Vektis 2017.
- 9. van Es M, Nicolaï L. Hoe gaat het met de praktijkondersteuner-ggz? Tijdschr praktijkondersteuning. 2015;10(2):42-48.
- 10. Magnée T, de Beurs D, Schellevis F, Verhaak P. Steeds belangrijkere rol huisartsenpraktijk bij psychische problemen. Huisarts Wet. 2018;61(11):14-17.
- 11. Landelijke Huisartsen Vereniging (LHV). Functie- en competentieprofiel POH-GGZ 2014. Utrecht: Nederlands Huisartsen Genootschap (NHG) 2014.
- 12. Hakkaart-van Roijen L, Van der Linden N, Bouwmans C, Kanters T, Tan SS. Kostenhandleiding. Methodologie van kostenonderzoek en referentieprijzen voor economische evaluaties in de gezondheidszorg In opdracht van Zorginstituut Nederland Geactualiseerde versie 2015.
- 13. Versteegh MM, Vermeulen KM, Evers SM, de Wit GA, Prenger R, Stolk EA. Dutch tariff for the five-level version of EQ-5D. Value Health. 2016;19(4):343-352.
- 14. Bouwmans C, De Jong K, Timman R, et al. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res. 2013;13(1):217.
- 15. Independer. Huisartstarieven 2017. https://www.independer.nl/huisarts/info/wat-kost-een-huisarts/huisartstarieven.aspx. Accessed October 23, 2019.
- 16. Zorginstituut Nederland. Farmacotherapeutisch Kompas Geneesmiddelen. https://www.farmacotherapeutischkompas.nl/. Accessed October 10, 2019.
- 17. Zorginstituut Nederland. Medicijnkosten. https://www.medicijnkosten.nl/. Accessed October 10, 2019.
- 18. Brouwer W, van Baal P, van Exel J, Versteegh M. When is it too expensive? Cost-effectiveness thresholds and health care decision-making. Eur J Health Econ. 2019;20(2):175-180.
- 19. Spitzer RL, Kroenke K, Williams JB. https://www.phqscreeners.com/select-screener. Accessed October 5, 2019.
- 20. Fonti V, Belitser E. Feature selection using lasso. VU Amsterdam Research Paper in Business Analytics 2017.
- 21. Wiebe S, Guyatt G, Weaver B, Matijevic S, Sidwell C. Comparative responsiveness of generic and specific quality-of-life instruments. J Clin Epidemiol. 2003;56(1):52-60.
- 22. Wijnen BFM, Mosweu I, Majoie MHJM, et al. A comparison of the responsiveness of EQ-5D-5L and the QOLIE-31P and mapping of QOLIE-31P to EQ-5D-5L in epilepsy. Eur J Health Econ. 2018;19(6):861-870.