 |
G Clin Nefrol Dial 2021; 33: 99-101 ISSN 2705-0076 | DOI: 10.33393/gcnd.2021.2296 SHORT COMMUNICATION |
 |
Silver dressing in cutaneous emergency management
ABSTRACT
Introduction: Exit-site (ES) and tunnel infections are the main infectious complications in peritoneal dialysis (PD); they also are risk factors for the development of peritonitis, for catheter removal and for dialysis drop-out.
Up to now, besides the recommendations of the Guidelines there is no uniformity on the classification, nor on the treatment strategies of the infected ES.
Recent experiences are reported with alternative types of dressings that aim to reduce the incidence of ES infection and consequently of the subcutaneous tunnel.
Methods: The Tuscan group conducted a retrospective observational study of 44 patients with PD who, showing signs of a suspected but not ascertained infection (negative microbiological culture), such as redness, edema, secretion, scab, had been medicated with silver ions releasing Exit-Pad Ag. The aim was to evaluate and classify the evolution of ES lesions, in order to confirm the preventive efficacy of the silver ions releasing dressing compared to the traditional ones.
Results: After 4 weeks of treatment with Exit-Pad Ag maintained in situ for 72 hours, 24 patients no longer had any signs of inflammation. In two cases, several weeks of treatment were necessary to achieve a complete recovery, while in two other cases the signs of inflammation became negative in less time (2 weeks, 1 week).
Conclusions: With the utilization of an alternative dressing such as Exit-Pad Ag on PD patients showing early signs of inflammation, the onset of a true infection can be prevented, with a progressive improvement of the ES.
Keywords: Exit-site, Infection, Prevention, Silver
Received: July 26, 2021
Accepted: August 5, 2021
Published online: September 15, 2021
Giornale di Clinica Nefrologica e Dialisi - ISSN 2705-0076 - www.aboutscience.eu/gcnd
© 2021 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Prevention of catheter exit-site (ES) infections is considered essential for the proper maintenance of peritoneal dialysis (PD). These infections are considered serious as their evolution can lead to peritonitis, loss of the catheter and drop-out from dialysis. The preventive actions that make it possible to reduce their incidence are therefore of extreme importance (1). In the case of colonization of the ES, the bacteria are able to produce inflammatory reactions characterized by the appearance of the classic signs such as local redness, pain, scab, secretion, even without there being clinical evidence of a real infection. According to the 1993 ES alteration classification system (2), the presence of scab or redness without purulent secretion, of keloid without serous or purulent secretion, of serous secretion during emergence maturation indicates an ES to ‘Keep under observation’. To date, in addition to the recommendations of the Guidelines, there is no uniformity on the classification or on the treatment strategies of infected ES, but it is also recognized that its proper management is the primary element for the prevention of infections (3).
The literature reports numerous experiences with types of advanced dressings that aim to stabilize the emergency site through ‘continuous’ disinfection, in order to reduce the incidence of infection of the ES and consequently of the subcutaneous tunnel (4). These devices releasing antimicrobial substances seem to have the dual advantage of counteracting the onset of infections and improving the management of patients undergoing dialysis treatment. Recently (2017–2018) the Tuscan Nursing Group of Peritoneal Dialysis (GIT DP) conducted an observational retrospective study on several PD patients who, showing signs of a suspected but not ascertained infection (negative swab), such as redness, edema, secretion, presence of crust, had been medicated with Exit-Pad Ag silver ion-releasing pad, comparing them with patients who, despite presenting the same symptoms, continued to use a traditional dressing. The purpose was to evaluate, classify and observe the evolution of ES lesions, in order to confirm the preventive effectiveness of the silver-release dressing, compared to the standard ones (in gauze).
Methodology
In the period between February 2017 and February 2018, 49 patients on home PD treated by GIT DP showed signs of inflammation following the evaluation of the ES, based on the ISPD 2005 classification (5).
This classification provides for a scoring system according to Table I:
| 0 points | 1 point | 2 points | |
|---|---|---|---|
| Edema | No | ES <0.5 cm | >0.5 cm ES and/or Tunnel |
| Scab | No | <0.5 | >0.5 |
| Redness | No | <0.5 | >0.5 |
| Pain | No | Modest | Severe |
| Secretion | No | Serous | Purulent |
ES = exit site.
Of these patients, five had a positive result with culture swab and followed appropriate antibiotic therapy.
Therefore, data relating to the dressings performed on 44 patients were collected, 28 of whom had followed a protocol that provided for the use of a pad with controlled release of silver ions, instead of the traditional gauze dressing, as an adjuvant for the prevention of the onset of infection at the ES.
For all patients evaluated, the protocol envisaged applying the new dressing (standard or advanced silver release) every other day, or at least twice a week, removing the old one and observing the emergence point and the surrounding area to detect any signs of redness, edema or discharge.
Results
Of the total 44 patients monitored, 28 used advanced medication until the complete regression of symptoms, and in any case for a period not exceeding 4 weeks, while 16 used a standard dressing.
Out of the total number of patients, 26 no longer showed signs of inflammation in 4 weeks, and of these 92% had used the silver ion dressing (Graph 1).
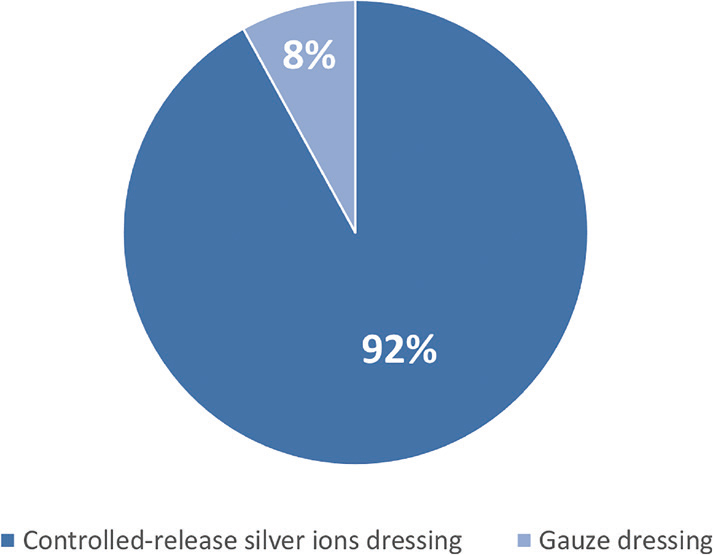
Graph 1 - Patients with total regression of signs of inflammation.
Of the patients who did not show signs of healing, 78% used the cotton gauze dressing (Graph 2), and in two cases the clinical situation worsened until infection, with a positive culture swab.
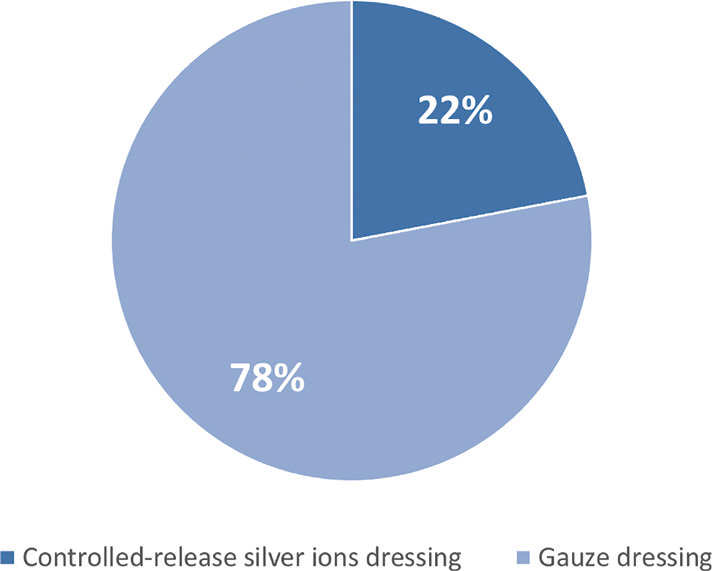
Graph 2 - Patients without regression of signs of inflammation.
In 86% of cases in patients receiving advanced medication, the symptoms disappeared in the first 4 weeks, and in most cases (71%), this happened within 2 weeks. Only two patients medicated with cotton gauze healed within the observation time.
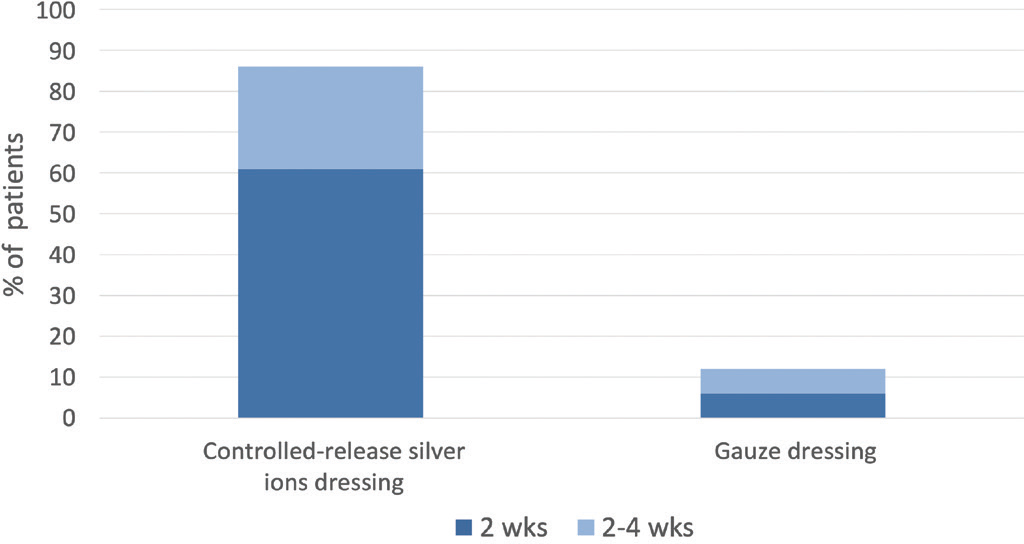
Graph 3 - Time chart for symptom resolution in patients with total regression of signs of inflammation.
In the group of patients who performed the advanced dressing, there were two cases of resolution of symptoms in the time interval between two dressings (3 days) and three cases in a week.

Fig. 1- Exit site detection of red skin stage 2, pain and scab stage 1.
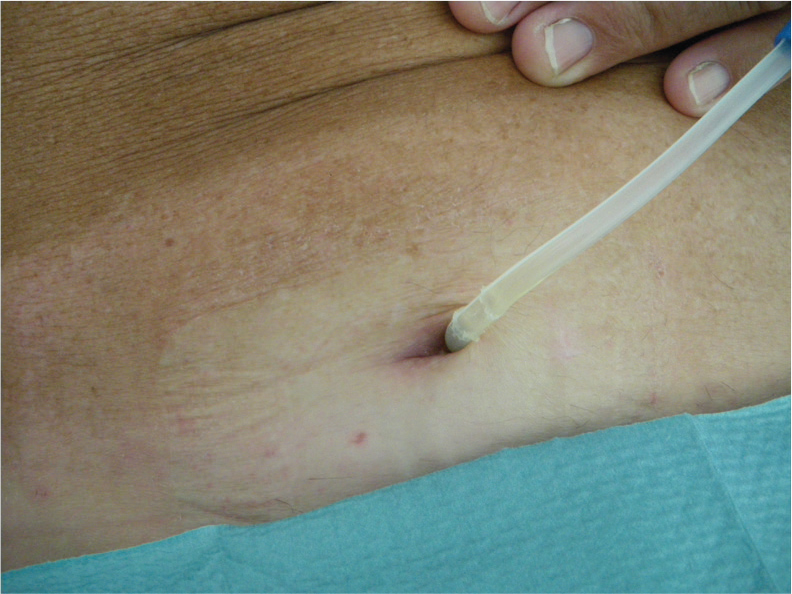
Fig. 2 - Exit site resolution after 4 weeks of treatment with silver ion-releasing dressing.
Conclusions
From the analysis of the results collected in this observational evaluation conducted by GIT DP it emerged that the correct use of an advanced dressing that has a controlled antibacterial action, such as that releasing silver ions, can help prevent infections and consequently it can improve EC in those patients who present with inflammatory symptoms, but who, not having a positive result with culture swab, are not subjected to antibiotic therapy.
Acknowledgment
This is the final version of record of this article as stated in DOI 10.33393/gcnd.2021.2359
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: The publication of this article has been made possible through an unconditional support from Emodial Srl.
References
- 1. De Vecchi AF. Le infezioni dell’exit-site in dialisi peritoneale De Vecchi. Giornale Italiano di Nefrologia; 2004;21:519-530. Online (Data di accesso Luglio 2021).
- 2. Cancarini G, De Vecchi A. Diagnosi e cura dell’infezione dell’emergenza del catetere nei Centri del Gruppo Cooperativo: impressioni ed esperienze. In: Manuale di Dialisi Peritoneale. Milano: Wichtig Editore 1993:156-169.
- 3. Lovedaya HP, Wilson JA, Pratt RJ, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hospital Infect. 2014; 86 (Suppl 1): S1-S70. CrossRef PubMed
- 4. Prowant BF, Warady BA, Nolph KD. Peritoneal dialysis catheter exit-site care: results of an international survey. Perit Dial Int. 1993;13(2):149-154. CrossRef PubMed
- 5. Piraino B, Bailie GR, Bernardini J, et al; ISPD Ad Hoc Advisory Committee. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005;25(2):107-131. CrossRef PubMed