 |
Drug Target Insights 2023; 17: 114-119 ISSN 1177-3928 | DOI: 10.33393/dti.2023.2614 ORIGINAL RESEARCH ARTICLE |
 |
Prevalence of antibiotic misuse in cases of pneumonia and diarrhea in Saudi Arabia
ABSTRACT
Background: Antibiotic misuse is a major public health issue with long-term repercussions.
Objective: The purpose of this investigation was to evaluate the effects of pneumonia and diarrhea, with an emphasis on antibiotic misuse.
Methodology: This study included 410 participants (217 fathers and 193 mothers), of whom 239 purchased antibiotics for their children without a prescription, whereas 171 had a prescription or were unsure if one was required.
Results: Antibiotics were used incorrectly by 58.1% of respondents. About 51.2% of participants said they were taking two antibiotics at the same time. Around 30% of people admitted to using antibiotics inefficiently. The most prevalent reason for use was “viral and bacterial,” followed by “viral,” and then “bacterial,” with 35%, 21%, and 20%, respectively. In addition, 22.4% of patients have used antibiotics for an unknown reason.
Conclusion: Saudi parents of children with pneumonia and diarrhea abuse antibiotics. Saudi legislation banning medications without a prescription has helped reduce antibiotic abuse, but more community-based education and awareness are needed.
Keywords: Antibiotic abuse, Antibiotic misuse, Diarrhea, Pneumonia, Saudi Arabia
Received: May 31, 2023
Accepted: September 7, 2023
Published online: October 9, 2023
Corresponding author:
Hussain Gadelkarim Ahmed
Department of Histopathology and Cytology
FMLS, University of Khartoum, Khartoum - Sudan
hussaingad5@gmail.com
Drug Target Insights - ISSN 1177-3928 - www.aboutscience.eu/dti
© 2023 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Abuse of antibiotics is a major global public health hazard, needing concerted efforts to control its spread (1). Antimicrobial resistance threatens global food, health, and development. Antibiotic resistance is caused by antibiotic misuse. Maximizing antibiotic use improves medical outcomes, reduces toxicity, and prevents resistance (2). Antibiotic resistance genes (ARGs) have plagued antibiotic treatment and antimicrobial chemotherapy worldwide due to overuse and misuse (3).
Like any health issue, affluence and antibiotic usage vary depending on the type of antibiotic abuse and the country’s health level. Understanding the social and economic factors could help create antibiotic misuse prevention programs and policies (4).
Because of the country’s high rates of antimicrobial administration without a prescription, antimicrobial abuse and misuse have reached pandemic proportions in Saudi Arabia. Implementation of the regulation in Saudi Arabia’s public pharmacies led to a slight decrease in the use of antimicrobials without prescriptions (5). Most antibiotics are misused or overused in Saudi Arabia for the treatment of upper respiratory tract infections (URTIs), which are predominantly viral infections (6). The current study investigates antibiotic usage in Saudi Arabia after the restriction on antibiotic sales without a prescription, with pneumonia and diarrhea being the most common indicators of antibiotic misuse.
Materials and methods
Between May 2022 and December 2022, 410 local inhabitants participated in a community-based survey in Hail, which is located in northern Saudi Arabia. When selecting participants at random, no consideration was paid to their age, social standing, degree of education, or monthly income. To be eligible, a child’s parents had to show that they had already purchased antibiotics for their child’s pneumonia or diarrhea. Antibiotic misusers are parents who give antibiotics to their children without first obtaining a doctor’s prescription or doing a culture and sensitivity test. Individuals whose antibiotic use could be proven were considered not to be misusing the medications. A poll found that 239 parents bought antibiotics for their children without a prescription, whereas 171 had a prescription or were unsure if they needed one (including 217 fathers and 193 mothers).
Data analysis
The data was analyzed using SPSS, which generated cross-tabulations, frequencies, and statistically significant results. We utilized a 95% confidence interval (CI) chi-square test to determine significance. Data with a p-value less than 0.05 was considered significant.
Results
This study comprised parents aged 20 to 60 years; 217/410 (52.9%) fathers and 193/410 (47.1%) mothers were polled. A total of 239/410 (58.1%) respondents admitted to using antibiotics inappropriately; an additional 12/410 (3.1%) were unsure. About 210 (51.2%) of the 410 participants reported using two antibiotics at the same time, while 17 (4.4%) were unsure; 123/410 people (30%) said they didn’t use antibiotics enough, while 28/410 (6.8%) weren’t sure. The most common category was “viral and bacterial,” followed by “viral,” and then “bacterial,” with relative frequencies of 35% (144/410), 22% (89/410), and 20% (85/410). Furthermore, approximately 92/410 (22.4%) patients have used antibiotics for an unknown reason, as indicated in Table I, Figures 1 and 2.
| Variable | Yes | No | Don’t know | Total |
|---|---|---|---|---|
| Antibiotic misuse | 239 | 159 | 12 | 410 |
| Antibiotic double use | 210 | 183 | 17 | 410 |
| Antibiotic complete use | 259 | 123 | 28 | 410 |
| Treatment indication | Viral | Bacterial | Viral and bacterial | Unknown |
| Frequencies | 89 | 85 | 144 | 92 |
About 176 out of 299 participants (59%) chose the wrong antibiotic to treat pneumonia, while 114 out of 299 (38%) chose the right antibiotic and 9 out of 299 (3%) were not sure.
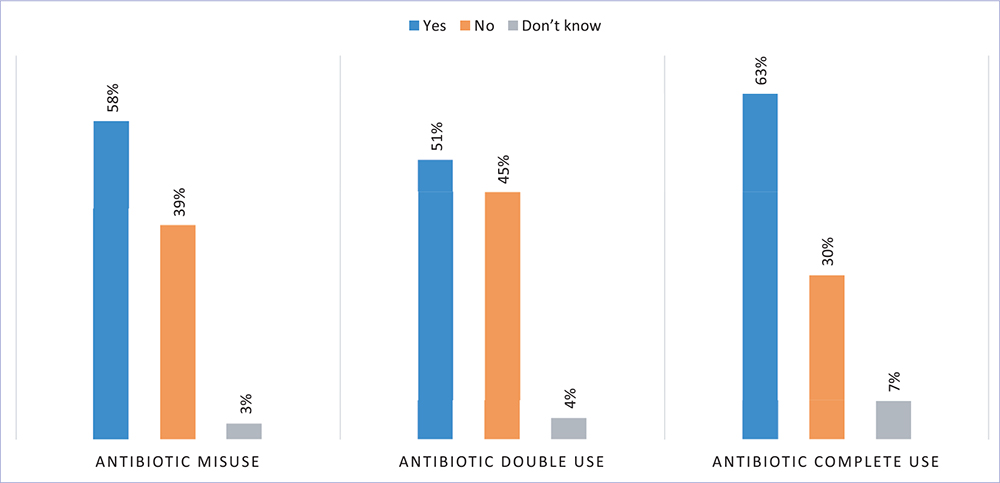
Fig. 1 - Description of the participants by antibiotic use status.
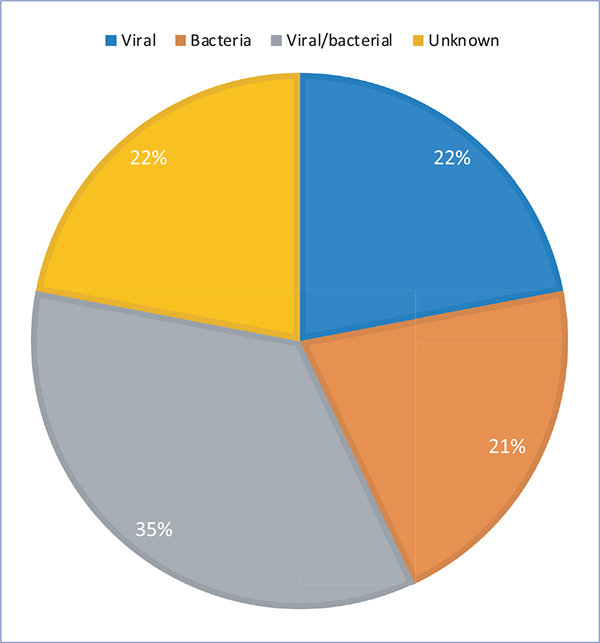
Fig. 2 - Indications of antibiotic use by study participants.
Approximately 68/112 (60.7%) children used the antibiotic incorrectly for diarrhea, 42/112 (37.5%) used it appropriately, and only 2/112 (1.8%) were uncertain. Only 114/299 (38%) of the 299 children with pneumonia had used the right antibiotics, as indicated in Table II.
In comparison to 117/193 (60%) mothers, around 122/217 (56.2%) fathers purchased improper antibiotics. The relative risk (RR) and 95% CI for moms purchasing unsuitable antibiotics were RR (95% CI) = 1.0783 (0.9157 to 1.2697), p = 0.3662.
Antibiotic abuse was most prevalent in the 35–44 age range, followed by 25–34 and 45 years, with 100/239 (42%), 88 (37%), and 42 (17.6%), respectively.
| Antibiotic misuse | Yes | No | Unsure | Total |
|---|---|---|---|---|
| Pneumonia | ||||
| Yes | 176 | 114 | 9 | 299 |
| No | 38 | 33 | 0 | 71 |
| Unsure | 25 | 12 | 3 | 40 |
| Total | 239 | 159 | 12 | 410 |
| Diarrhea | ||||
| Yes | 68 | 42 | 2 | 112 |
| No | 143 | 101 | 6 | 250 |
| Unsure | 28 | 16 | 4 | 48 |
| Total | 239 | 159 | 12 | 410 |
Antibiotic misuse was reported by 58% of married people, 75% of divorcees, and 25% of widows. The probability that children of divorced parents will abuse antibiotics is RR (95% CI) = 1.2305 (0.9179 to 1.6495), p = 0.1654, and the z statistic is 1.387.
Around 132/203 (65%) of those with ≥5 family members reported antibiotic abuse, compared to 107/207 (51.7%) of those with <5 family members. The RR of antibiotic abuse was 1.2580 (1.0656 to 1.4850), with a 95% CI of 1.0656 to 1.4850 (p < 0.001) (see Tab. III, Fig. 3).
The status of antibiotic use in relation to the parents’ level of education, occupation, and income was summarized in Table IV and Figure 4. About 151/275 (55%) parents with a college degree used antibiotics wrongly, compared to 68/107 (64%) parents with a secondary education and 20/28 (71%) parents with a primary education. Reduced education increased the risk of antibiotic abuse: RR (95% CI) = 0.7187 (0.5915–0.8731), p = 0.0009, z statistic = 3.326.
About 158/287 (55%) government employees, 41/63 (65%) self-employed, and 40/60 (67%) unemployed reported antibiotic abuse. The risk associated with self-employed and unemployed antibiotic usage is RR (95% CI) = 1.1962 (1.0146 to 1.4104), p = 0.0330, and the z statistic = 2.132.
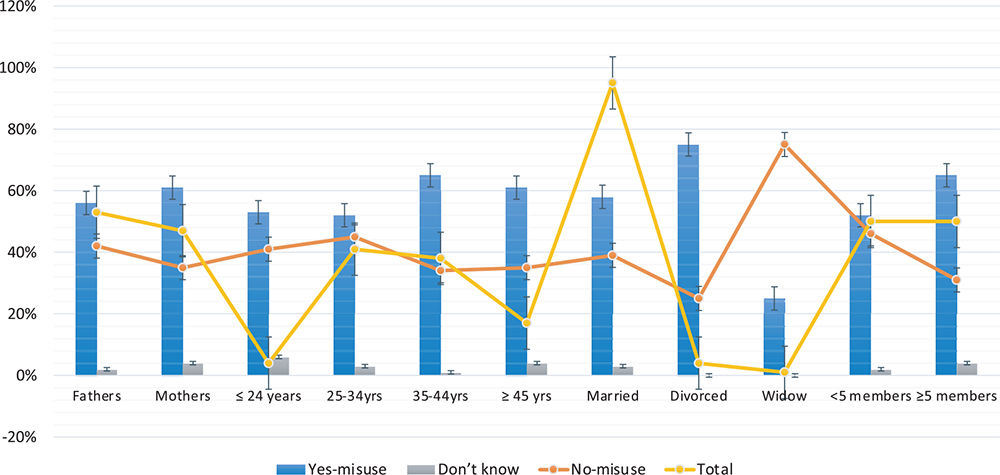
Fig. 3 - Description of status of antibiotic use for each of the categories of social and demographic factors.
About 33/56 (59%), 83/139 (60%), 87/145 (60%), and 36/70 (51%) of parents with monthly incomes of less than 5,000, 5,000 to 9,000, 10,000 to 14,000, and >15,000 SAR, respectively, misused antibiotics.
Table V summarizes the negative effects of using antibiotics in various situations. Approximately 150/230 (65%) of the children of individuals who were exposed to antibiotic overuse later had negative effects; 129/210 (61.4%) of the 210 antibiotics that were used twice had negative effects; 194/299 (65%) of the 299 pneumonia patients experienced adverse symptoms. About 75/112 (67%) of the 112 children who had diarrhea experienced adverse symptoms.
| Antibiotic misuse | Yes | No | Don’t know | Total |
|---|---|---|---|---|
| Parent | ||||
| Father | 122 | 91 | 4 | 217 |
| Mother | 117 | 68 | 8 | 193 |
| Total | 239 | 159 | 12 | 410 |
| Age (years) | ||||
| ≤24 | 9 | 7 | 1 | 17 |
| 25–34 | 88 | 76 | 6 | 170 |
| 35–44 | 100 | 52 | 2 | 154 |
| ≥45 | 42 | 24 | 3 | 69 |
| Total | 239 | 159 | 12 | 410 |
| Social status | ||||
| Married | 226 | 152 | 12 | 390 |
| Divorced | 12 | 4 | 0 | 16 |
| Widow | 1 | 3 | 0 | 4 |
| Total | 239 | 159 | 12 | 410 |
| Family members | ||||
| <5 members | 107 | 96 | 4 | 207 |
| ≥5 members | 132 | 63 | 8 | 203 |
| Total | 239 | 159 | 12 | 410 |
| Antibiotic misuse | Yes | No | Don’t know | Total |
|---|---|---|---|---|
| Education | ||||
| Primary | 20 | 8 | 0 | 28 |
| Secondary | 68 | 33 | 6 | 107 |
| Universal | 151 | 118 | 6 | 275 |
| Total | 239 | 159 | 12 | 410 |
| Occupation | ||||
| Government employees | 158 | 120 | 9 | 287 |
| Self-employed | 41 | 22 | 0 | 63 |
| Unemployed | 40 | 17 | 3 | 60 |
| Total | 239 | 159 | 12 | 410 |
| Monthly income (SAR) | ||||
| <5,000 | 36 | 29 | 5 | 70 |
| 5,000-9,000 | 87 | 55 | 3 | 145 |
| 10,000-14,000 | 83 | 53 | 3 | 139 |
| ≥15,000 | 33 | 22 | 1 | 56 |
| Total | 239 | 159 | 12 | 410 |
Discussion
The findings of this study reveal that despite Saudi Arabia’s ban on acquiring antibiotics without a prescription, a considerable number of people continue to misuse antibiotics. According to the Saudi Law Compendium, pharmacists are not permitted to provide therapeutic advice. The Saudi Ministry of Health (MOH) revised the rule to include financial penalties, license revocation, business closure, and a 6-month prison sentence for the pharmacist. In May 2018, antibiotic distribution regulations were validated (7,8).
| Side effects | Yes | No | Unsure | Total |
|---|---|---|---|---|
| Antibiotic misuse | ||||
| Yes | 150 | 33 | 56 | 239 |
| No | 101 | 28 | 30 | 159 |
| Unsure | 3 | 4 | 5 | 12 |
| Total | 254 | 65 | 91 | 410 |
| Antibiotic double use | ||||
| Yes | 129 | 31 | 50 | 210 |
| No | 120 | 29 | 34 | 183 |
| Unsure | 5 | 5 | 7 | 17 |
| Total | 254 | 65 | 91 | 410 |
| Pneumonia | ||||
| Yes | 194 | 44 | 61 | 299 |
| No | 39 | 15 | 17 | 71 |
| Unsure | 21 | 6 | 13 | 40 |
| Total | 254 | 65 | 91 | 410 |
| Diarrhea | ||||
| Yes | 75 | 12 | 25 | 112 |
| No | 156 | 43 | 51 | 250 |
| Unsure | 23 | 10 | 15 | 48 |
| Total | 254 | 65 | 91 | 410 |
Substantial rates of antibiotic misuse (58.1%) and overuse (51%) were found in the present investigation, both of which have undesirable effects such as the emergence of antimicrobial resistance and financial burdens. Antibiotic resistance is a major public health concern that has received a great deal of attention in recent years from physicians and researchers. Misusing or overusing antibiotics can lead to resistance, which is caused by natural selection and the evolution of bacteria (9).
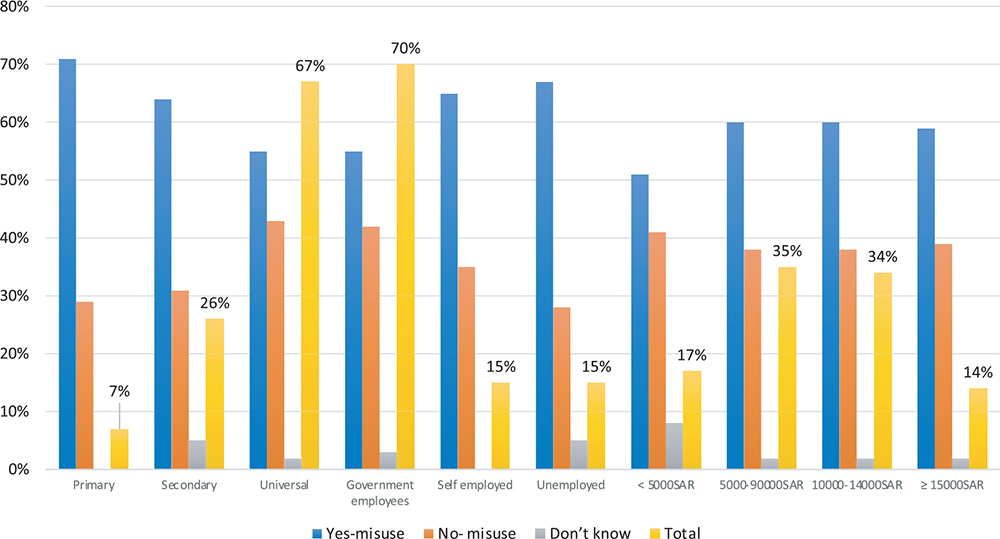
Fig. 4 - Description of antibiotic use status within education, occupation, and income categories.
Physicians are struggling to improve patient outcomes due to rising infection rates, multidrug-resistant bacteria, and antibiotic use. Optimizing antimicrobial use can enhance patient outcomes, avoid resistance, and reduce drug abuse and overuse (10,11). A recent study in Saudi Arabia evaluated the antibiotic consumption after the adoption of a new prescription-only antimicrobial dispensing policy in community pharmacies. Generally, non-prescription antimicrobial use has dropped slightly (5). Although effective prescription limitations must be implemented, community-based activities are deemed essential.
Approximately 30% of this study’s participants reported using an inadequate antibiotic dose, and 6.8% were unclear. Clinicians and other health providers should advise patients to finish the entire course of prescribed antibiotics, even if their symptoms have subsided, in order to stop the spread of antibiotic resistance and avoid a resurgence of illness (12).
According to the findings of this investigation, many drugs were abused in cases of viral ailments. Furthermore, around 59% of patients were given the wrong drug to treat pneumonia. The overuse of antibiotics to treat viral community-acquired pneumonia is a major public health issue. According to one study, antibiotics were given to 98.3% of patients who had viral pneumonia (13). Antibiotic overuse, especially for viral, self-limiting respiratory tract infections like sore throats, increases community-wide antimicrobial resistance. Approximately 80% of sore throats are viral and resolve without medicine. Although there are over-the-counter topical sore throat medicines, antibiotics are still administered inappropriately (14). However, whereas viral illnesses are more prevalent in children, adults with viral respiratory tract infections are more likely to overuse antibiotics (15).
In this study, approximately 60.7% of children used the antibiotic incorrectly for diarrhea. Over a million people die annually from the consequences of infectious diarrhea, which affects more than four billion people worldwide. A consistent geographic surveillance system would help fight the worrying rise in worldwide resistance caused by antimicrobial overuse and misuse (16). However, there is a scarcity of data on how Saudi eating habits may be linked to diarrhea in young children. Diarrhea was shown to be common among children aged 0 to 2 years, and it was also discovered that exclusive breastfeeding was not often followed in Saudi Arabia (17). About 40.3% of Saudi mothers thought it was a major problem in the Saudi community, but nearly 23% couldn’t identify any critical sign of severe diarrhea, and 66% incorrectly stated that diarrhea is caused by teething (18).
According to the current study, mothers, particularly divorced mothers, are more likely to abuse antibiotics. Antibiotic misuse is more common in families with five or fewer members, and additional research is needed in this context. Furthermore, the current study’s findings demonstrate that antibiotic overuse is inversely associated with education level. Furthermore, self-employed individuals receive more antibiotics that are misused than government employees. In this study, however, there was no correlation between monthly income and antibiotic misuse. Parents must accurately observe the use of antibiotics in their children. Although parental antibiotic awareness, attitude, and practice have received little attention, most parents were uninformed, pessimistic, and did not administer antibiotics to their children correctly. Children’s antibiotic use was influenced by their parents’ socioeconomic position, education, occupation, knowledge, and viewpoint (19).
Saudi researchers sought to refute common beliefs among primary school parents regarding when and how to give their children URTI medications. Antibiotics were unnecessary for nasal congestion (62.5%) and fever (74%). Compared to 39.4% for ear pain and 26% for throat discomfort, 61% of respondents correctly identified URTI as a virus, while only 20% believed antibiotics could not immediately treat it (20). Recent systematic reviews and meta-analyses included only 57 of 702 publications. ASM was highest in the Middle East (34%), Africa (22%), Asia (20%), and South America (17%). ASM is more prevalent in children who live far from a hospital or whose families are poor due to having multiple children. Parents may overuse antibiotics when their children develop fevers or recurrent coughs. Antimicrobial pharmaceutical sales should be rigorously restricted to reduce self-medication.
Bert et al revealed that antibiotic self-medication (ASM) among children was highest in the Middle East (34%), Africa (22%), Asia (20%), and South America (17%) and lowest in Europe (8%). ASM risk in children is increased by a long distance from the hospital, a low income, and several children. Antibiotics are sometimes abused by parents due to fever and cough. Self-medication can be reduced by focusing on antimicrobial drug control (21).
Participants in the current study indicated that their children experienced negative side effects because of antibiotic usage for both pneumonia and diarrhea. Antibiotic abuse increases antimicrobial resistance and causes gastrointestinal, neurologic, and mental issues. Amoxicillin-clavulanate hepatotoxicity can be deadly. Overprescribing antibiotics for self-limiting infections increases patient readmission rates (22). However, in an era when new agents are required to combat multiresistant bacteria, balancing the dangers and advantages of existing antimicrobials is an intriguing challenge.
The past decade has significantly influenced global antibiotic stewardship. High-level policy conversations, regulations, and legislation have focused on antibiotic use improvements, and antibiotic stewardship infrastructure has grown rapidly in hospitals, nursing homes, and ambulatory settings (23). Antibiotic stewardship programs (ASPs) effectively reduced antibiotic misuse, decrease antibiotic resistance, and improve treatment outcomes. The Saudi MOH devised a national antimicrobial stewardship plan to implement ASPs in hospitals, but little is known about its success or factors. According to a statewide cross-sectional poll that included all MOH hospitals, the utilization of ASP was only verified in 26% of hospitals (24).
Even though this study was an important update on antibiotic abuse after Saudi Arabia banned antibiotics without a prescription, it had some limitations, such as a cross-sectional design and a low level of acceptability for data collection.
Conclusion
Antibiotic misuse is still prevalent among parents caring for children with pneumonia and diarrhea in Saudi Arabia. Even though laws in Saudi Arabia that say antibiotics can’t be given out without a prescription have helped cut down on antibiotic abuse, it is thought that more community-based education and awareness efforts are needed.
Acknowledgments
The authors are grateful to the study’s participants for providing samples.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This study was funded by the Deputy for Research and Innovation, Ministry of Education, through the Initiative of Institutional Funding at the University of Ha’il in Saudi Arabia. The project’s ID was IFP-22 048.
Informed consent: Participants in this study provided both written and verbal informed consent.
Ethical approval: The research plan received approval from the university’s ethics board. HERC 0137/CM.UOH/5/20 is the approval number.
Data availability: The data presented in this study is available on request from the corresponding author.
References
- 1. Iheanacho CO. “An antibiotic turned contraceptive”: the tale of ampicillin-cloxacillin. Health Sci Rep. 2022;5(1):e481. CrossRef PubMed
- 2. Goranova M, Ochoa G, Maier P, Hoyle A. Evolutionary optimisation of antibiotic dosing regimens for bacteria with different levels of resistance. Artif Intell Med. 2022;133:102405. CrossRef PubMed
- 3. Shi X, Xia Y, Wei W, Ni BJ. Accelerated spread of antibiotic resistance genes (ARGs) induced by non-antibiotic conditions: roles and mechanisms. Water Res. 2022;224:119060. CrossRef PubMed
- 4. Mallah N, Orsini N, Figueiras A, Takkouche B. Income level and antibiotic misuse: a systematic review and dose-response meta-analysis. Eur J Health Econ. 2022;23(6):1015-1035. CrossRef PubMed
- 5. Al-Jedai AH, Almogbel Y, Eljaaly K, et al. Restriction on antimicrobial dispensing without prescription on a national level: impact on the overall antimicrobial utilization in the community pharmacies in Saudi Arabia. PLoS One. 2022;17(7):e0271188. CrossRef PubMeD
- 6. Saleh Faidah H, Haseeb A, Yousuf Lamfon M, et al. Parents’ self-directed practices towards the use of antibiotics for upper respiratory tract infections in Makkah, Saudi Arabia. BMC Pediatr. 2019;19(1):46. CrossRef PubMeD
- 7. Alrafiaah AS, Alqarny MH, Alkubedan HY, AlQueflie S, Omair A. Are the Saudi parents aware of antibiotic role in upper respiratory tract infections in children? J Infect Public Health. 2017;10(5):579-585. CrossRef PubMeD
- 8. AlRukban M, AlRuthia Y, Almasaoud M, et al. Community pharmacists’ views of the enforced antibiotics dispensing law and its impact on oral antibiotics sales in Saudi Arabia. Risk Manag Healthc Policy. 2020;13:2899-2907. CrossRef PubMeD
- 9. Shah RA, Hsu JI, Patel RR, Mui UN, Tyring SK. Antibiotic resistance in dermatology: the scope of the problem and strategies to address it. J Am Acad Dermatol. 2022;86(6):1337-1345. CrossRef PubMeD
- 10. Murphy CV, Reed EE, Herman DD, Magrum B, Beatty JJ, Stevenson KB. Antimicrobial stewardship in the ICU. Semin Respir Crit Care Med. 2022;43(1):131-140. CrossRef PubMeD
- 11. Ashkenazi S. Antibiotic overuse and its effects on our planet. Isr Med Assoc J. 2022;24(6):353-356. PubMeD
- 12. Martinez MN, Papich MG, Drusano GL. Dosing regimen matters: the importance of early intervention and rapid attainment of the pharmacokinetic/pharmacodynamic target. Antimicrob Agents Chemother. 2012;56(6):2795-2805. CrossRef PubMeD
- 13. Jiang R, Han B, Dou C, Zhou F, Cao B, Li X. Analysis of antibiotic usage for viral community-acquired pneumonia in adults. Front Med. 2021;15(1):139-143. CrossRef PubMeD
- 14. Essack S, Bell J, Burgoyne DS, Duerden M, Shephard A. Topical (local) antibiotics for respiratory infections with sore throat: an antibiotic stewardship perspective. J Clin Pharm Ther. 2019;44(6):829-837. CrossRef PubMeD
- 15. van Houten CB, Cohen A, Engelhard D, et al. Antibiotic misuse in respiratory tract infections in children and adults-a prospective, multicentre study (TAILORED Treatment). Eur J Clin Microbiol Infect Dis. 2019;38(3):505-514. CrossRef PubMeD
- 16. Taitt CR, Leski TA, Prouty MG, et al. Tracking antimicrobial resistance determinants in diarrheal pathogens: a cross-institutional pilot study. Int J Mol Sci. 2020;21(16):5928. CrossRef PubMeD
- 17. Shati AA, Khalil SN, Asiri KA, et al. Occurrence of diarrhea and feeding practices among children below two years of age in southwestern Saudi Arabia. Int J Environ Res Public Health. 2020;17(3):722. CrossRef PubMeD
- 18. Alghadeer S, Syed W, Alhossan A, et al. Assessment of Saudi mother’s knowledge and attitudes towards childhood diarrhea and its management. Int J Environ Res Public Health. 2021;18(8):3982. CrossRef PubMeD
- 19. Mutagonda RF, Marealle AI, Nkinda L, et al. Determinants of misuse of antibiotics among parents of children attending clinics in regional referral hospitals in Tanzania. Sci Rep. 2022;12(1):4836. CrossRef PubMeD
- 20. Al-Shawi MM, Darwish MA, Abdel Wahab MM, Al-Shamlan NA. Misconceptions of parents about antibiotic use in upper respiratory tract infections: a survey in primary schools of the Eastern Province, KSA. J Family Community Med. 2018;25(1):5-12. CrossRef PubMeD
- 21. Bert F, Previti C, Calabrese F, Scaioli G, Siliquini R. Antibiotics self medication among children: a systematic review. Antibiotics (Basel). 2022;11(11):1583. CrossRef PubMeD
- 22. Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014;5(6):229-241. CrossRef PubMeD
- 23. Cosgrove SE, Srinivasan A. Antibiotic stewardship: a decade of progress. Infect Dis Clin North Am. 2023 Aug 1:S0891-5520(23)00047-8. CrossRef PubMeD
- 24. Alghamdi S, Berrou I, Aslanpour Z, et al. Antimicrobial stewardship programmes in Saudi hospitals: evidence from a national survey. Antibiotics (Basel). 2021;10(2):193. CrossRef PubMed