 |
Drug Target Insights 2022; 16: 49-53 ISSN 1177-3928 | DOI: 10.33393/dti.2022.2481 ORIGINAL RESEARCH ARTICLE |
 |
Success of 14-day triple and quadruple therapy for the control of Helicobacter pylori infections in Kohat district
ABSTRACT
Introduction: Helicobacter pylori is an important medical pathogen present in more than half of the world’s population. Various treatment regimen are in use for the eradication of H. pylori, but due to the emergence of antibiotic resistance, its management is a big issue for clinicians.
Methods: In this study all suspected cases that had visited District Headquarters Hospital Kohat were considered for screening of H. pylori infections. Preliminary information about their age, gender, general health conditions, occupation, etc. was taken for consideration. After recording initial signs and symptoms, samples were considered for H. pylori detection using stool antigen test and endoscopy. Fourteen-day proton pump inhibitor base triple and quadruple therapy were administered to each patient.
Results: In total (n = 178), there were high numbers of positivity in patients aged below 30 years (82; 46.06%), most of whom belonged to rural areas.
Conclusion: This study concludes that there were high numbers of positive patients aged below 30 years, and according to this study MEL (Metronidazole + Esomeprazole + Levofloxacin) is the most effective treatment regimen for the eradication of H. pylori.
Keywords: Gastric pathology, Helicobacter pylori, Intestinal metaplasia, Peptic ulcer
Received: August 4, 2022
Accepted: November 30, 2022
Published online: December 19, 2022
Drug Target Insights - ISSN 1177-3928 - www.aboutscience.eu/dti
© 2022 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Helicobacter pylori is a Gram negative, microaerophilic bacteria that is very common, infecting more than half of the world’s population (1). H. pylori infection can cause gastric inflammation, peptic ulcer, intestinal metaplasia and can lead to gastric cancer (2,3). Its urease activity, flagella mobility, adhesive proteins and S-shape help to colonize the human stomach and initiate infection (4). Besides these, the cagA and vacA genes are the major virulence factors in H. pylori, responsible for the gastric pathology. The cagA gene is responsible for peptic ulcer disease and adenocarcinoma, while the vagA gene causes injury to gastric epithelium (5,6). Its invasiveness in the human stomach instigates mucosal and systemic immune responses in the infected host but it has acquired some mechanism that can evade host responses (7).
H. pylori infection rates vary by geographic location, age, ethnicity and socioeconomic status of population (8). It has been documented that infection rates are higher in poor socioeconomic conditions, particularly in developing countries (9). Its transmission takes place in different ways. Most common routes of transmission are iatrogenic, feco-oral and person-to-person contact (10,11). Along with this, contaminated food and water may be a source of infection (12).
Different strategies have been adopted for its treatment. Commonly and most acceptable treatment therapies are triple and quadruple therapy (13,14). In recent era due to the emergence of antibiotic resistance, its success has declined. Antibiotic resistance to H. pylori is considered the major cause of the eradication failure (15,16). One of the most enduring debates in the world is the optimal duration of therapy for its eradication (17).
The incidence of H. pylori eradication failure and antibiotic resistance has been documented worldwide. In Pakistan, the rate of H. pylori is very high due to lack of proper diagnosis of dyspepsia and the over-the-counter use of inappropriate doses of proton pump inhibitors (PPIs). In our population of the District of Kohat, the rate of H. pylori infection is increasing day by day, and it is yet to find factors that lead to eruption of resistance. Therefore, keeping in view the existence data regarding its resistance and treatment failure of H. pylori infection, the study was conducted to determine the incidence of H. pylori infection and its response to different regimen of eradication in Kohat district. The aim of the study was to recognize the best treatment regimen for the eradication of H. pylori.
Methods
This study was conducted at the District Headquarters Hospital Kohat and Kohat University of Science and Technology, from April 2021 to December 2021. It was approved by the University Ethical Committee and written consent was taken from all patients. Only positive cases were considered in this study for further analysis.
Patients’ data collection and risk factors
All the patients were asked about the issues related to gastrointestinal problems and their socioeconomic status, and all data were recorded accordingly. A questionnaire was used as the data collection tool, and it was given after obtaining written informed consent. All the patients were also questioned about their gastric information or complaints like nausea, vomiting, epigastric pain and ballottement.
Sample collection
From all suspected cases stool samples (10-20 g) were collected from all the patients and placed in a clean container. Stool antigen test was used for the detection of H. pylori infection. Blood sera were also collected from each patient. Three to 5 mL of blood was taken from each patient and analyzed through an automated hematology analyzer for the complete blood count (18).
Stool antigen test
Stool antigen test was performed for the detection of H. pylori infection. About 1 g of collected sample was diluted with the buffer present in the specimen collection tube. Suspending diluted sample for 2 min, 2-3 drops of the diluted specimen were added to the well and then waited for the appearance of faint line to read the result (19).
Treatment regimen for H. pylori eradication
Three different treatment regimen were used for control of H. pylori positive cases. These were MEL (Metronidazole + Esomeprazole + Levofloxacin), MRL (Metronidazole + Rabeprazole + Levofloxacin) and MELB (Metronidazole + Esomeprazole + Levofloxacin + Bismuth subcitrate) treatment strategies. In the designated study each patient received PPI base triple and bismuth quadruple treatment. All the patients were randomly assigned to the 14-day treatment comprising of Esomeprazole 40 mg, Rabeprazole 20 mg, Metronidazole 500 mg, Levofloxacin 500 mg and bismuth subcitrate. PPI and bismuth were recommended to be taken before meals while all the antibiotics were taken after meals. Successful eradication was defined as negative result after reconfirmation through the stool antigen test after successful 14-day therapy (20).
Statistical analysis
Qualitative and quantitative variables are shown as percentages. The relationship between hematological parameters of H. pylori positive patients and H. pylori negative control group was evaluated using confidential interval method by which the values are calculated for each parameter that will fall between intervals.
Results
In total there were 178 patients positive for H. pylori infection; there were 38.76% (n = 69) female and 61.23% (n = 109) male positive cases. Among the total, there were high numbers of positivity (n = 82; 46.06%) in patients aged below 30 years, while the number of positive patients in group aged 30-50 years is 38.76% (n = 69) and in that of above 50 years is 15.16% (n = 27). Of the 178 patients, 71.91% (n = 128) were living in the rural area while 28.08% (n = 50) were living in the urban area. According to the above results, high numbers of the patients were living in the rural area and only a small number of patients were living in the urban areas. The demographic information and characteristic of the suspected patients are shown in Table I.
| Demographic factors | Numbers | Percentage (%) |
|---|---|---|
| Age | ||
| Below 30 years | 82 | 46.06 |
| 30-50 years | 69 | 38.76 |
| Above 50 years | 27 | 15.16 |
| Gender | ||
| Male | 109 | 61.23 |
| Female | 69 | 38.76 |
| Literate | 40 | 22.47 |
| Illiterate | 138 | 77.52 |
| Place of living | ||
| Rural | 128 | 71.91 |
| Urban | 50 | 28.08 |
Gastrointestinal symptoms were almost similar in all the patients, but there were high numbers of patients who complained of epigastric pain and recurrent abdominal pain; all the patients showed more than one symptom as mentioned in Table II.
| Symptom | Numbers | Percentage (%) |
|---|---|---|
| Epigastric pain | 153/178 | 85.95 |
| Recurrent abdominal pain | 138/178 | 77.52 |
| Nausea | 141/178 | 79.21 |
| Vomiting | 70/178 | 39.32 |
| Ballottement | 30/178 | 16.85 |
| Water brush | 65/178 | 36.51 |
The hematological parameters of H. pylori patients included (n = 52) H. pylori positive patients whose hematological values were compared with H. pylori negative control group (n = 52). It showed that the hemoglobin level was low in the positive patients. Comparing platelets and neutrophile, it was increased in the infected patients as shown in Table III.
| Parameter | Patients (N = 52) | Negative control (N = 52) |
|---|---|---|
| Hemoglobin, g/dL | 12.82 ± 1.79 | 14.37 ± 1.06 |
| Platelet count, % | 304,043 ± 8311.8 | 223,360 ± 3498 |
| Neutrophile | 61.32 ± 5.57 | 59.34 ± 6.91 |
| Eosinophile | 2.85 ± 0.89 | 3.22 ± 1.12 |
| Monocytes | 2.41 ± 0.53 | 4.29 ± 1.16 |
| Lymphocytes | 30.36 ± 7.80 | 27.87 ± 5.97 |
The above results show the eradication percentage of each given regimen in which 100 patients were given MEL, out of whom 88 (88%) patients showed successful eradication (Fig. 1). MRL was given to 53 patients, of whom 40 patients recovered, exhibiting 75.47% eradication percentage. The bismuth-based quadruple therapy (MELB) was given to 25 patients, of whom 21 (84%) patients showed successful eradication after 14 days of therapy, as shown in Table IV.
| Regimen | Eradication (%) | Eradication failure |
|---|---|---|
| MEL | 88/100 (88%) | 12/100 (12%) |
| MRL | 40/53 (75.47%) | 13/53 (24.52%) |
| MELB | 21/25 (84%) | 4/25 (16%) |
MEL = Metronidazole + Esomeprazole + Levofloxacin; MRL = Metronidazole + Rabeprazole + Levofloxacin; MELB = Metronidazole + Esomeprazole + Levofloxacin + Bismuth subcitrate
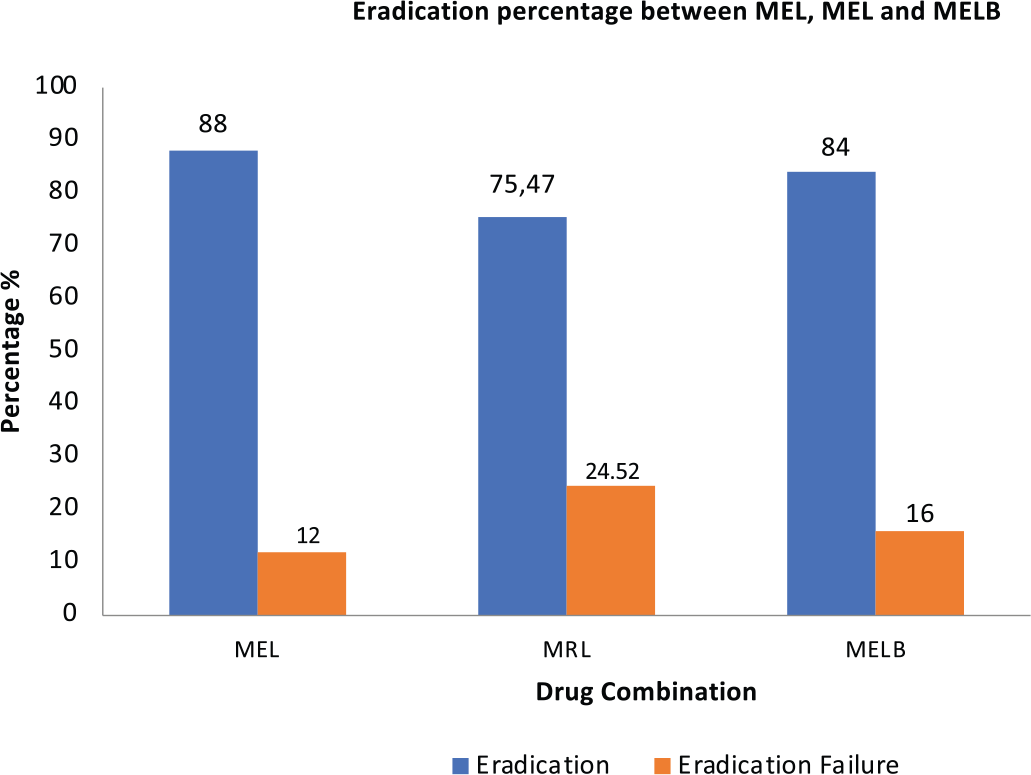
Fig. 1 - Successful eradication and failure percentage between MEL, MRL and MELB drug combinations. MEL = Metronidazole + Esomeprazole + Levofloxacin; MRL = Metronidazole + Rabeprazole + Levofloxacin; MELB = Metronidazole + Esomeprazole + Levofloxacin + Bismuth subcitrate.
Discussion
H. pylori infection is the most common bacterial infection in the world, infecting about half of the world’s population. This infection is more common in areas where there are poor hygienic conditions such as use of contaminated food and water. This bacterium is mainly transmitted by feco-oral route from the fecal contaminated water. The oral-oral route is also the leading cause of the infection, as few authentic studies have cultured H. pylori from the oral cavity (21); the oral-oral transmission has been examined in the eating of premasticated food, the use of the same spoon by mother and children (22). Various diagnostic methods have been identified for the detection of H. pylori but the choice usually depends on the sampling and condition of the patient. In this study, the stool antigen test has been used for the diagnosis of H. pylori as stool antigen test is noninvasive and rapid for the detection of H. pylori infection (23).
H. pylori analysis included 178 positive patients in this study in which most of the patients were less than 30 years of age. One of the studies in Egypt included 89 asymptomatic young patients, out of whom 78 were positive for H. pylori antigen, all aged below 30 years (24). A total of 128 patients out of 178 belonged to the rural areas, exhibiting high percentage because of the poor hygienic conditions of the people living in the rural areas. Most authentic studies have also shown that most of the H. pylori positive patients were from rural areas, where the environment was not hygienic. Similarly, one of the studies in Venezuela revealed that H. pylori in the rural population was found in 87.2% (34/39) of the patients (25). H. pylori is associated with a number of symptoms that are still in debate. In this study, all the patients complained of gastrointestinal symptoms, but there were high number of patients who complained about epigastric pain and recurrent abdominal pain. The main reason behind this is the hyperacidity during peptic ulcer. Primarily, gastrin and oxyntic gland are responsible for the production of more acid during H. pylori infection that can lead to epigastric pain (26).
In this study, we found abnormalities in some of the hematological parameters of H. pylori positive patients when compared to the control group. The hemoglobin level is quite lower than the control group, while the platelets and neutrophil level remarkably increased. This may be due to the inflammatory conditions and immune response to H. pylori.
| Patient details | Treatment 1 (MEL) | Treatment 2 (MRL) | Treatment 3 (MELB) | |||
|---|---|---|---|---|---|---|
| Success % | Failure % | Success % | Failure% | Success % | Failure% | |
| 1. Male (n = 109) | 57 (90.47%) | 6 (9.53 = 2%) | 17 (70.83%) | 7 (30.43%) | 20 (90.90%) | 2 (9.09%) |
| 2. Female (n = 69) | 31 (83.78%) | 6 (16.21%) | 23 (79.31%) | 6 (20.68%) | 1 (33.3%) | 2 (66.6%) |
| Success of treatment regimen according to age | ||||||
| 3. Below 30 years (n = 82) | 45 (84.90%) | 8 (15.09%) | 12 (63.15%) | 7 (36.84%) | 8 (80%) | 2 (20%) |
| 4. 30-50 years (n = 69) | 31 (91.17%) | 3 (8.82%) | 20 (83.33%) | 4 (16.66%) | 9 (81.81%) | 2 (18.18%) |
| 5. After 50 years (n = 27) | 12 (92.30%) | 1 (7.69%) | 8 (80%) | 2 (20%) | 4 (100%) | 0 (0%) |
| Resident wise | ||||||
| 6. Rural (n = 128) | 60 (86.95%) | 9 (13.04%) | 32 (76.19%) | 10 (23.80%) | 14 (82.35%) | 3 (17.64%) |
| 7. Urban (n = 50) | 28 (90.32%) | 3 (9.67%) | 8 (72.72%) | 3 (27.27%) | 7 (87.5%) | 1 (12.5%) |
| Total 178 | 88/100 (88%) | 12/100 (13.72%) | 40/53 (75.47%) | 13/53 (24.52%) | 21/25 (84%) | 4/25 (16%) |
MEL = Metronidazole + Esomeprazole + Levofloxacin; MRL = Metronidazole + Rabeprazole + Levofloxacin; MELB = Metronidazole + Esomeprazole + Levofloxacin + Bismuth subcitrate
Eradication of H. pylori needs combinations of drug treatment with adjuvant regimen that increase antibiotic activity and host responses. The duration of therapy also strongly affects the eradication of H. pylori. One of the studies in the United States was based on the duration of therapy of H. pylori, which shows that RAC (Rabeprazole, Amoxicillin, and Clarithromycin) treatment of 7 days and 10 days had a higher percentage of eradication than the 3-day treatment (27). Similarly, a study in Turkey based on levofloxacin triple therapy in which MEL was given to 92 patients showed 95.5% positive response toward MEL combination. In this study, each patient was given 14 days treatment of PPI base triple and quadruple therapy, which show that MEL had a high percentage of eradication (88/100; 88%) followed by MELB (21/25; 84%). MEL and MRL are the same triple therapy with two different PPIs (Tab. V). The reason for changing one PPI to another was that some of the patients in either group were already using that drug with the same name, so for patient satisfaction, psychologically, we changed the drug. Another reason is some of the studies showed better results with rabeprazole than esomeprazole (28).
Conclusion
This study concludes that there were high numbers of positive patients aged below 30 years in which many patients were from rural area, and according to this study MEL is the most effective treatment regimen for the eradication of H. pylori. This study recommends that clinicians may suggest MEL treatment for H. pylori positive patients for complete eradication of H. pylori.
Disclosures
Financial support: This study was part of the basic research with a focus on patients’ treatment and was mainly supported and conducted at District Headquarters Hospital Kohat, Pakistan. We extend our gratitude to the Department of Microbiology, Kohat University of Science and Technology, for providing lab facilities and supporting this research.
Conflict of interest: The authors declare that they have no conflict of interests.
Authors’ contribution: Syed Fahim Shah and Sohail Aziz Paracha conducted the experiments; Somaid iqbal helped in editing the manuscript and in conducting experimentations; Sadar Zaman, Mudassir Hussain, Hafeez Ullah and Iqbal Muhammad helped in sample collection; Aisha Gul helped in experimentations; and Waheed Ullah designed the project and wrote the manuscript.
References
- 1. Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420-429. CrossRef PubMed
- 2. Eshraghian A. Epidemiology of Helicobacter pylori infection among the healthy population in Iran and countries of the Eastern Mediterranean Region: a systematic review of prevalence and risk factors. World J Gastroenterol. 2014;20(46):17618-17625. CrossRef PubMed
- 3. Qadri Q, Rasool R, Gulzar GM, Naqash S, Shah ZAH. H. pylori infection, inflammation and gastric cancer. J Gastrointest Cancer. 2014;45(2):126-132. CrossRef PubMed
- 4. Scott DR, Marcus EA, Wen Y, Oh J, Sachs G. Gene expression in vivo shows that Helicobacter pylori colonizes an acidic niche on the gastric surface. Proc Natl Acad Sci USA. 2007;104(17):7235-7240. CrossRef PubMed
- 5. Al-Khattaf AS. Helicobacter pylori virulence markers in gastroduodenal disorders. Detection of cytotoxin-associated gene A and vacuolating cytotoxin-associated gene A genes in Saudi patients. Saudi Med J. 2012;33(7):716-721. PubMed
- 6. Ribeiro ML, Godoy APO, Benvengo YHB, Mendonça S, Pedrazzoli J Jr. Clinical relevance of the cagA, vacA and iceA genotypes of Helicobacter pylori in Brazilian clinical isolates. FEMS Immunol Med Microbiol. 2003;36(3):181-185. CrossRef PubMed
- 7. Abadi ATB. Strategies used by Helicobacter pylori to establish persistent infection. World J Gastroenterol. 2017;23(16):2870-2882. CrossRef PubMed
- 8. Omosor KI, Omosor OH, Ibeh IN, et al. Seroprevalence of Helicobacter pylori infection and risk factors among asymptomatic subjects in Delta State, Nigeria. Adv Microbiol. 2017;7(9):641-652. CrossRef
- 9. Zamani M, Ebrahimtabar F, Zamani V, et al. Systematic review with meta-analysis: the worldwide prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2018;47(7):868-876. CrossRef PubMed
- 10. Brown LM. Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev. 2000;22(2):283-297. CrossRef PubMed
- 11. Rothenbacher D, Bode G, Berg G, et al. Helicobacter pylori among preschool children and their parents: evidence of parent-child transmission. J Infect Dis. 1999;179(2):398-402. CrossRef PubMed
- 12. Nurgalieva ZZ, Malaty HM, Graham DY, et al. Helicobacter pylori infection in Kazakhstan: effect of water source and household hygiene. Am J Trop Med Hyg. 2002;67(2):201-206. CrossRef PubMed
- 13. Xie Y, Zhu Y, Zhou, H, et al. Furazolidone-based triple and quadruple eradication therapy for Helicobacter pylori infection. World J Gastroenterol. 2014;20(32):11415-11421. CrossRef PubMed
- 14. Gisbert JP, Romano M, Gravina AG, et al. Helicobacter pylori second-line rescue therapy with levofloxacin- and bismuth-containing quadruple therapy, after failure of standard triple or non-bismuth quadruple treatments. Aliment Pharmacol Ther. 2015;41(8):768-775. CrossRef PubMed
- 15. Zhong Z, Zhang Z, Wang J, et al. A retrospective study of the antibiotic-resistant phenotypes and genotypes of Helicobacter pylori strains in China. Am J Cancer Res. 2021;11(10):5027-5037. PubMed
- 16. Saracino IM, Pavoni M, Zullo A, et al. Antibiotic resistance and therapy outcome in H. pylori eradication failure patients. Antibiotics (Basel). 2020;9(3):121. CrossRef PubMed
- 17. AlRuthia Y, Almadi MA, Alqahtani S, Alrasheed H, Al-Owairdhi M, Alsohaibani F. The cost-effectiveness of sequential versus standard triple therapy for Helicobacter pylori eradication in Saudi Arabia. Saudi J Gastroenterol. 2021 Jul-Aug;27(4):217-222. CrossRef PubMed
- 18. Hsu PI, Tsay FW, Kao JY, et al; Taiwan Acid-related Disease, Microbiota (TARD-M) Consortium. Tetracycline-levofloxacin versus amoxicillin-levofloxacin quadruple therapies in the second-line treatment of Helicobacter pylori infection. Helicobacter. 2021;26(5):e12840. CrossRef PubMed
- 19. Iranikhah A, Ghadir MR, Sarkeshikian S, Saneian H, Heiari A, Mahvari M. Stool antigen tests for the detection of Helicobacter pylori in children. Iran J Pediatr. 2013;23(2):138-142. PubMed
- 20. Sun Q, Liang X, Zheng Q, et al. High efficacy of 14-day triple therapy-based, bismuth-containing quadruple therapy for initial Helicobacter pylori eradication. Helicobacter. 2010;15(3):233-238. CrossRef PubMed
- 21. Wang XM, Yee KC, Hazeki-Taylor N, et al. Oral Helicobacter pylori, its relationship to successful eradication of gastric H. pylori and saliva culture confirmation. J Physiol Pharmacol. 2014;65(4):559-566. PubMed
- 22. Fujimoto Y, Furusyo N, Toyoda K, Takeoka H, Sawayama Y, Hayashi J. Intrafamilial transmission of Helicobacter pylori among the population of endemic areas in Japan. Helicobacter. 2007;12(2):170-176. CrossRef PubMed
- 23. Kouitcheu Mabeku LB, Bello Epesse M, Fotsing S, et al. Stool antigen testing, a reliable noninvasive method of assessment of Helicobacter pylori infection among patients with gastro-duodenal disorders in Cameroon. Dig Dis Sci. 2021;66(2):511-520. CrossRef PubMed
- 24. Salem OE, Youssri AH, Mohammad ON. The prevalence of H. pylori antibodies in asymptomatic young Egyptian persons. J Egypt Public Health Assoc. 1993;68(3-4):333-352. PubMed
- 25. Contreras M, Fernández-Delgado M, Reyes N, García-Amado MA, Rojas H, Michelangeli F. Helicobacter pylori infection in rural and urban dyspeptic patients fr26 Venezuela. Am J Trop Med Hyg. 2015;93(4):730-732. CrossRef PubMed
- 26. Waldum HL, Kleveland PM, Sørdal ØF. Helicobacter pylori and gastric acid: an intimate and reciprocal relationship. Therap Adv Gastroenterol. 2016;9(6):836-844. CrossRef PubMed
- 27. Vakil N, Lanza F, Schwartz H, Barth J. Seven-day therapy for Helicobacter pylori in the United States. Aliment Pharmacol Ther. 2004;20(1):99-107. CrossRef PubMed
- 28. Fock KM, Teo EK, Ang TL, Chua TS, Ng TM, Tan YL. Rabeprazole vs esomeprazole in non-erosive gastro-esophageal reflux disease: a randomized, double-blind study in urban Asia. World J Gastroenterol. 2005;11(20):3091-3098. CrossRef PubMed