 |
Arch Physioter 2024; 14: 90-95 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3267 ORIGINAL RESEARCH ARTICLE |
 |
Indoor and outdoor 10-Meter Walk Test and Timed Up and Go in patients after total hip arthroplasty: a reliability and comparative study
ABSTRACT
Introduction: The 10-Meter Walk Test (10MWT) and Timed Up and Go (TUG) are valid tools for gait performance and mobility assessment after total hip arthroplasty (THA). The study aimed to assess test-retest reliability of 10MWT and TUG in indoor and outdoor environments in patients in acute phase after THA and compare their indoor vs. outdoor performance during these tests.
Methods: Thirty-five inpatients performed 10MWT and TUG in indoor and outdoor settings on the second postoperative day. An additional evaluation session was performed after 1 hour under the supervision of the same operator. Test-retest reliability was assessed using Intraclass Correlation Coefficient (ICC: 2.1) and Minimal Detectable Change (MDC95), while paired t-tests were used to compare indoor vs. outdoor performance.
Results: Indoor (ICC: 0.94, MDC95: 0.13 m/s) and outdoor (ICC: 0.91, MDC95: 0.16 m/s) 10MWT at maximum speed and indoor (ICC: 0.92, MDC95: 2.5 s) and outdoor (ICC: 0.93, MDC95: 2.4 s) TUG revealed excellent reliability. Indoor (ICC: 0.86, MDC95: 0.16 m/s) and outdoor (ICC: 0.89, MDC95: 0.16 m/s) 10MWT at spontaneous speed revealed good reliability. Spontaneous (mean difference [MD]: 0.05 m/s, 95% confidence interval [CI95]: 0.03, 0.07, p < 0.001) and maximum (MD: 0.02 m/s, CI95: 0.01, 0.04, p < 0.001) 10MWT revealed higher gait speed when performed outdoors compared to indoors.
Conclusions: Indoor and outdoor 10MWT and TUG are reliable tests in acute phase after THA. Higher gait speed during outdoor 10MWT may depend on test score variability, due to MDs being lower than MDC95.
Keywords: Gait performance, Hip arthroplasty, Indoor setting, Mobility, Outdoor setting
Received: August 20, 2024
Accepted: October 14, 2024
Published online: November 4, 2024
Corresponding author:
Federico Temporiti
email: federico.temporiti@humanitas.it
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What’s already known about this topic?
- The 10MWT and TUG are valid measurements tools, which are widely used for assessing gait performance and mobility of patients in acute phase after THA.
What does the study add?
- The 10MWT and TUG in indoor and outdoor settings are reliable tests in acute phase after THA. Higher gait speed was found during 10MWT performed outdoors compared to indoors, but changes are lower than MDC95.
Introduction
Total hip arthroplasty (THA) represents a successful surgical procedure to reduce pain and improve function and quality of life in patients with end-stage hip osteoarthritis (1). The advancements in surgical techniques (e.g., minimally invasive surgical approaches) and improvements in perioperative care (e.g., prehabilitation and early mobilization protocols) have allowed for length of stay reduction, which decreased from some weeks to a few days in patients undergoing THA (2-4). When considering patients in acute phase after THA, the achievement of clinical stability and functional outcomes represents a milestone to establish the readiness for hospital discharge (3). In fact, functional independence during the execution of basic daily activities and satisfactory levels of walking performance and mobility are required to ensure a safe discharge in these patients (3,5,6).
The 10-Meter Walk Test (10MWT) and Timed Up and Go (TUG) are valid measurement tools for walking performance and mobility assessment in patients after lower limb orthopedic surgery (7,8). The 10MWT consists of asking patients to walk along a 10-m walkway at self-paced and maximum speed to detect spontaneous and maximum walking speed by timing the performance (7). During TUG, patients are asked to rise from an armchair, walk at a comfortable pace for 3 m, turn and walk back to the chair and sit down again. The performance is timed to detect the test duration, which is an index of functional mobility (8). However, when considering 10MWT and TUG in patients with THA, the reliability of these tests has only been described in patients with end-stage hip osteoarthritis and in the subacute phase after THA and in a sample of patients suffering from heterogeneous musculoskeletal conditions affecting the lower limb (8-12). In addition, the assessment of walking performance and mobility in patients discharged after THA is usually carried out in a hospital setting (e.g., rehabilitative gyms or ward hallways), which represent an indoor, familiar and supervised setting in which patients have performed a rehabilitative program during postoperative days. However, hospital discharge often induces patients to perform outdoor activities in unfamiliar environments, where the ability to adapt to unexpected perturbations during gait and other functional tasks is required (13). In this context, studies have described motor performance changes between unfamiliar outdoor environment and familiar indoor setting in older adults and patients with gait disorders (14,15). Therefore, it is reasonable to speculate that the execution of motor performance tests such as 10MWT and TUG in indoor and outdoor settings may be more representative of the locomotor performance and mobility in patients discharged in acute phase after THA.
To date, no studies have investigated the reliability of indoor and outdoor 10MWT and TUG in patients discharged in acute phase after THA. Moreover, walking performance and mobility in an indoor vs. outdoor environment have never been compared in these patients. The first study’s aim was to assess test-retest reliability of 10MWT and TUG in indoor and outdoor environments in patients in acute phase after THA. The second study’s aim was to compare indoor vs. outdoor performance during these tests in patients in acute phase after THA. We hypothesized that indoor and outdoor 10MWT and TUG would result in good to excellent test-retest reliability in patients in the acute phase after THA. Moreover, we expected better 10MWT and TUG scores when these tests were performed indoors compared to outdoors.
Methods
Participants
Thirty-five inpatients with unilateral THA were enrolled on the second postoperative day. Inclusion criteria were age between 40 and 80 years, primary unilateral THA for osteoarthritis (Kellgren-Lawrence grade of at least 3) and readiness for discharge (16). Patients with a Kellgren-Lawrence grade of at least 3 were included in order to select participants who underwent THA for advanced stage of hip osteoarthritis including narrowing of joint space and bone sclerosis. Discharge criteria included the ability to stand up from a standard chair, walk at least 100 m, and perform stairs with crutches. In addition, dry wound, hemoglobin levels higher than 8 g/dL, perceived pain at rest and during walking lower than 4 points on a Visual Analogue Scale (VAS 0-10), and absence of dizziness or nausea were required. Exclusion criteria were revision surgery, perioperative complications, diagnosis of cognitive impairment or psychiatric disorders, and concurrent neurological or musculoskeletal conditions able to influence postoperative functional recovery. All participants were operated under spinal anesthesia by three orthopedic surgeons of the same unit adopting a standardized posterolateral approach with femur-first technique and uncemented implant fixation (17). All patients followed a postoperative in-hospital rehabilitation program under the supervision of a physiotherapist. The rehabilitative protocol consisted of two 30-minute daily sessions including manual therapy techniques to improve hip range of motion, resistance training to enhance strength of lower limb muscles, and task-oriented exercises performed in standing posture for increasing postural stability. In addition, patients were trained on the execution of functional daily tasks, such as getting out of bed, sitting on a chair, walking as tolerated, and stairs performance with crutches (18). The study was carried out at the Physiotherapy Unit of the Humanitas Clinical and Research Center of Milan, Italy. All participants signed a written informed consent as per the Declaration of Helsinki and the ethical committee of our institute approved the study protocol (number: CLF23/04).
Assessment
An experienced physiotherapist enrolled participants on the afternoon of the second postoperative day. Immediately after the enrollment, participants performed the 10MWT at self-paced and maximum speed and TUG in a familiar indoor (rehabilitation gym) and unfamiliar outdoor (straight sidewalk composed of flat tiles in the hospital garden) settings in a randomized order. The indoor and outdoor sessions were interspaced by a 5-minute resting period and the modified Borg scale was used to monitor the participants’ fatigue (19). Specifically, participants had to report a fatigue level equal to 0 before each session. Moreover, a wheelchair was used to transfer participants from indoor to outdoor environments in order to avoid fatigue onset. During 10MWT, participants were asked to walk with crutches for 14 m at self-paced speed and as quickly as possible. The initial and final 2 m were used for acceleration and deceleration and the performance was timed using a stopwatch to detect spontaneous and maximum gait speed. Two trials were performed for self-paced and maximum speed conditions, and the mean score was used for data analysis (10). After 10MWT, participants were asked to perform the TUG. In particular, they were asked to rise from an armchair, walk at a comfortable speed for 3 m without crutches, turn and walk back to the chair in order to sit down again. After a familiarization trial, two trials were performed. The performance was timed with a stopwatch to detect test duration, and the best trial was used for data analysis (20). The test execution complied with the most recent guidelines on the use of restrictions and assistive devices in patients in acute phase after THA, which recommended the lack of hip movement restrictions in these patients (21). After 1 hour, the indoor and outdoor sessions were repeated in the same sequence adopted during the first session and under the supervision of the same operator to evaluate the test-retest reliability of 10MWT and TUG in indoor and outdoor settings (Fig. 1).
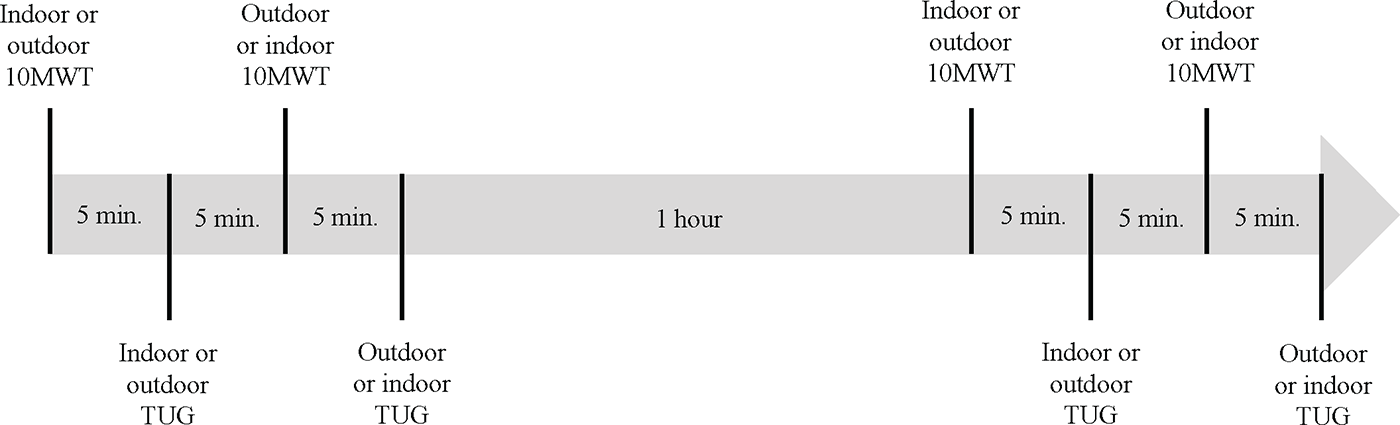
FIGURE 1 - Representation of study design. 10MWT = 10-Meter Walk Test; TUG = Timed Up and Go.
Perceived pain was assessed by an experienced physiotherapist at the end of each indoor and outdoor session using the Numeric Pain Rating Scale (NPRS), which consists of an 11-point numerical scale with a score ranging from 0 (no pain) to 10 points (maximum pain). Finally, hip function and impact of hip-related signs and symptoms on daily activities were assessed to further characterize study participants. Hip function was assessed through the Harris Hip Score (HHS), which consists of a 10-item questionnaire ranging from 0 (high dysfunction) to 100 (no dysfunction) and exploring pain, hip function, daily activities, hip deformities, and range of motion. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) consists of a 24-item self-administered questionnaire used to assess the impact of hip pain, stiffness, and function on the performance of daily activities.
Data analysis
Sample size was calculated a priori using the methodology proposed by Walter and coworkers (22). Considering two repetitions per subject, alpha error of 0.05, power (1-beta) of 80%, and a minimum acceptable Intraclass Correlation Coefficient (ICC) score of 0.5, 35 participants were required to determine an ICC score of 0.8.
All measurements were checked for normality using the Shapiro-Wilk test, and being normally distributed, were expressed as mean and standard deviation. The ICC 2.1 with a 95% confidence interval (CI95) was adopted to assess the relative reliability and interpreted as excellent (0.9 or greater), good (between 0.75 and 0.9), moderate (between 0.5 and 0.75), and poor (0.5 or lower) (23). In addition, the Standard Error of Measurement (SEM) was adopted to investigate the absolute reliability. It was computed as SEM = SD √1-ICC, where SD represents the standard deviation of the mean of all trials, and expressed in the same measurement unit of the test score (m/s for 10MWT and seconds for TUG) and as a percentage of the mean. Moreover, the minimal detectable change with 95% confidence (MDC95) computed as MDC = 1.96 SEM √2 was adopted to obtain a measure of the change in terms of 10MWT and TUG scores that may be considered as a true change beyond the measurement errors.
Finally, paired t-test was used to compare 10MWT and TUG scores in an indoor vs. outdoor setting. Effect size was also quantified using Cohen’s d with 95% CI and interpreted as small (0.2), medium (0.5), or large (0.8 or greater) (24). Data were analyzed using SPSS 28.0 for Windows and the level of significance was set at alpha = 0.05.
Results
All participants completed the evaluation sessions correctly; no dropouts occurred and none of the participants required a longer resting period between indoor and outdoor sessions. Participants had a mean age of 58.5 years (SD: 6.9 years, range: 46-80 years), a mean height of 1.71 m (SD: 0.01 m, range 1.56-1.83 m), a mean weight of 80.6 kg (SD: 16.9 kg, range: 48-102 kg), and a mean body mass index of 26.7 kg/m2 (SD: 4.1 kg/m2, range: 18.8-33.2 kg/m2). Twenty-two men and 13 women who underwent 22 right-sided and 17 left-sided THA were included. Twenty-four patients had preoperative Kellgren-Lawrence grade 3, while nine patients had preoperative Kellgren-Lawrence grade 4. Finally, participants reported a mean WOMAC score of 51.1 points (SD: 21.1 points) and a mean HHS score of 58.5 points (SD: 10.7 points).
Reliability
Excellent test-retest reliability was found for 10MWT performed indoors (ICC: 0.94, p < 0.001, and MDC95: 0.13 m/s) and outdoors (ICC 0.91, p < 0.001, and MDC95: 0.16 m/s) at maximum speed, while good test-retest reliability was found for 10MWT performed indoors (ICC: 0.86, p < 0.001, and MDC95: 0.16 m/s) and outdoors (ICC: 0.89, p < 0.001, and MDC95: 0.16 m/s) at spontaneous speed. Finally, excellent test-retest reliability was found for TUG performed indoors (ICC: 0.92, p < 0.001, and MDC95: 2.5 s) and outdoors (ICC: 0.93, p < 0.001, and MDC95: 2.4 s) (Tab. 1).
| Variables | Test | Retest | ICC [CI 95%] | p-Value | SEM | SEM% |
|---|---|---|---|---|---|---|
| Indoor setting | ||||||
| 10MWT – self-paced speed (m/s) | 0.83 ± 0.17 | 0.92 ± 0.15 | 0.86 [0.13; 0.96] | <0.001 | 0.06 | 6.80 |
| 10MWT – maximum speed (m/s) | 1.10 ± 0.20 | 1.16 ± 0.20 | 0.94 [0.64; 0.98] | <0.001 | 0.05 | 4.34 |
| TUG (s) | 14.6 ± 3.1 | 13.5 ± 3.1 | 0.92 [0.62; 0.97] | <0.001 | 0.89 | 6.33 |
| Outdoor setting | ||||||
| 10MWT – self-paced speed (m/s) | 0.88 ± 0.17 | 0.97 ± 0.17 | 0.89 [0.17; 0.97] | <0.001 | 0.06 | 6.06 |
| 10MWT – maximum speed (m/s) | 1.12 ± 0.20 | 1.18 ± 0.19 | 0.91 [0.72; 0.96] | <0.001 | 0.06 | 5.22 |
| TUG (s) | 14.7 ± 3.4 | 13.9 ± 3.1 | 0.93 [0.84; 0.97] | <0.001 | 0.87 | 6.05 |
10MWT = 10-Meter Walk Test; CI = confidence interval; ICC = intraclass correlation coefficient; SEM = standard error of the measurement; TUG = Timed Up and Go.
| Variables | Indoors | Outdoors | MD [CI 95%] | p-Value | Cohen’s d |
|---|---|---|---|---|---|
| 10MWT – self-paced speed (m/s) | 0.88 ± 0.16 | 0.93 ± 0.17 | −0.05 [−0.07; −0.03] | <0.001 | 0.51 |
| 10MWT – maximum speed (m/s) | 1.13 ± 0.20 | 1.15 ± 0.20 | −0.02 [−0.05; −0.01] | 0.042 | 0.25 |
| TUG (s) | 14.0 ± 3.1 | 14.3 ± 3.3 | −0.3 [−0.59; 0.08] | 0.138 | – |
10MWT = 10-Meter Walk Test; CI = confidence interval; MD = mean difference; SEM = standard error of the measurement; TUG = Timed Up and Go.
Indoor vs. outdoor performance
Participants showed higher gait speed during 10MWT at spontaneous (MD: 0.05 m/s, IC95: 0.03, 0.07 m/s, p < 0.001) and maximum speed (MD: 0.02 m/s, IC95: 0.01, 0.04, p < 0.001) performed outdoor compared to indoor setting. The effect size was medium for 10MWT at spontaneous speed (d = 0.51, IC95: 0.76, 0.26) and small for 10MWT at maximum speed (d = 0.25, IC95: 0.01, 0.49). No significant differences were found for TUG performed in indoor or outdoor settings. Finally, no significant differences were found in terms of VAS at the end of the indoor and outdoor sessions (indoor assessment: 1.9 ± 1.2 points, outdoor assessment: 2.3 ± 1.0 points, p = 0.450) (Tab. 2).
Discussion
The main finding was that excellent to good reliability was found for 10MWT and TUG performed in indoor and outdoor settings in patients in acute phase after THA. Moreover, higher gait speed was found during 10MWT at self-paced and maximum speed, when this test was performed outdoors compared to indoors.
Literature data have described gait speed during 10MWT as an indicator of functional status in patients after lower limb orthopedic surgery including THA (10,25). When considering available literature, a single study of Unver and coworkers investigated the test-retest reliability of the 10MWT in patients with THA (10). The current study findings agree with the results of Unver and coworkers, which demonstrated excellent test-retest reliability (ICC: 0.96) for 10MWT at maximum speed in patients in the first week after THA (10). However, mean gait speed of patients included in the study of Unver and coworkers was substantially lower than mean gait speed observed in the current study participants (0.22 vs. 1.13 m/s), suggesting differences in terms of patients’ characteristics and functional abilities (10). Despite the lack of information, it is reasonable to speculate that hospital discharge criteria were not satisfied in patients enrolled in the study of Unver and coworkers compared to our study participants. In addition, our findings demonstrated good test-retest reliability for 10MWT performed at self-paced speed.
The current study also revealed excellent test-retest reliability for TUG performed indoors and outdoors in patients discharged in acute phase after THA. Our findings revealed ICC values higher than 0.90 both indoors and outdoors and suggested that only changes greater than 2.5 s (MDC95) in terms of TUG score may be interpreted as true changes. When considering existing literature data, studies have investigated the test-retest reliability of TUG performed indoors, showing ICC values ranging from 0.83 to 0.98 in patients after THA (11,20,26). In particular, the clinical features of our study population are similar to the characteristics of patients included in the study of Kirschner and coworkers, which found an ICC value of 0.98 for TUG in patients with THA (26). However, participants included in the aforementioned study had greater body mass index than our study participants and revealed a mean TUG score of approximately 20 s (26). Moreover, Yuksel and coworkers described TUG test-retest reliability of 0.96 and 0.59 in terms of ICC and SEM values in patients at 6 months after THA (20). However, it is reasonable to speculate that patients enrolled by Yuksel and coworkers were extracted from a different population than participants of our study. In fact, Lieberman and co-workers reported that patients usually achieve a complete restoration of functional abilities at 6 months after THA (27). Furthermore, Doll and coworkers reported an ICC value of 0.83 for TUG in patients at 2 weeks after THA. Lower test-retest reliability in the aforementioned study may depend on the use of different walking aids among participants during TUG, such as one or two crutches or a walker (11). In fact, the use of walking aids might have increased the intrasubject variability between test and retest trials, affecting TUG reliability.
This was the first study that compared indoor versus outdoor performance in patients in acute phase after THA. Conversely to our hypothesis, patients with THA revealed higher spontaneous and maximum gait speed outdoors compared to indoors. This finding was consistent with the results of Schmitt and coworkers, which have described higher gait speed in young and elderly subjects in an outdoor compared to indoor setting, as a result of increased stimuli and multisensory feedback provided by the outdoor environment (15). However, it is worth also highlighting that the magnitude of changes in our study were 0.05 and 0.02 m/s for spontaneous and maximum speed, respectively. These values were lower than the MDC95 values described for indoor and outdoor 10MWT in patients in acute phase after THA, suggesting that observed changes may depend on the variability of the test score described in the study population (28). Conversely to Schmitt and coworkers, previous studies have reported no differences between indoor and outdoor performance in older adults and patients with gait disorders for neurological conditions, in agreement with the lack of environment influence on gait abilities and mobility in patients in acute phase after THA (13,29). The results of our study may depend on the fact that the central nervous system tends to redistribute the resources to adequately accomplish the task, when the performance is not maximal (30). In fact, self-paced 10MWT and TUG require submaximal levels of performance and 10MWT at maximum speed was performed using crutches, which might have contributed to limit the task maximality. The lack of task maximality might have hindered potential motor performance changes between indoor and outdoor settings. In addition, the adoption of compensatory mechanisms (e.g., higher reliance on visual inputs) might have played a role in ensuring similar levels of performance between indoor and outdoor settings (13).
The assessment of test-retest reliability of 10MWT and TUG and comparison between indoor and outdoor performance during these tests were carried out in patients in the acute phase after THA. Consistently with time following surgery, patients revealed poor hip function and the presence of hip-related signs and symptoms, as demonstrated by HHS lower than 70 points and WOMAC score of 51.1 points (31,32). In fact, these scores are similar to those reported by previous studies in patients in acute phase after THA (3,31,32).
Some limitations need to be underlined in the current study. First, our findings were extracted from patients in the acute phase after THA showing specific features. In fact, patients had no weight-bearing restrictions on the affected limb and achieved readiness for discharge within the second postoperative day. These factors limit the external validity of our findings and caution is needed to generalize the current results to a broader population undergoing THA. Second, outdoor assessment was carried out using a sidewalk in the hospital garden without ground irregularities or distracting elements, which may be only partially representative of the outdoor setting in which patients usually perform the activities of daily living. Third, mean age of participants was 58.5 years and the age range adopted in the inclusion criteria was slightly different from the age range of the majority of subjects undergoing primary THA in our country (16). Therefore, caution is needed to generalize the current study findings to a broader population of patients with THA. Finally, no instrumental assessment was carried out. In fact, the investigation of the reliability of spatial temporal parameter during 10MWT and TUG might have revealed potential differences between indoor and outdoor performance in acute phase after THA.
Conclusions
Indoor and outdoor 10MWT and TUG were reliable tests to assess walking performance and mobility in patients in acute phase after THA. Moreover, higher gait speed was found during 10MWT at self-paced and maximum speed outdoors compared to indoors, but the relevance of these changes remains questionable.
Acknowledgments
We thank prof. Patricia Taylor for the help on English language revision.
Disclosures
Conflict of interest: The authors have no conflicts of interests.
Funding: The authors received no funding.
Author contributions: FT: conceptualization, methodology, data collection, formal analysis, project administration, and writing. CC: data collection, methodology, visualization, and formal analysis. PA: methodology and data curation. DDL: data curation and visualization. GM: data curation and visualization. GG: conceptualization and supervision. RG: conceptualization, supervision, project administration, and writing.
Data availability statement: The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy policy of the institution.
References
- 1. Sato EH, Stevenson KL, Blackburn BE, et al. Impact of demographic variables on recovery after total hip arthroplasty. J Arthroplasty. 2024;39(3):721-726. CrossRef PubMed
- 2. Ohta Y, Sugama R, Minoda Y, et al. Is the anterolateral or posterolateral approach more effective for early postoperative recovery after minimally invasive total hip arthroplasty? J Clin Med. 2022;12(1):139. CrossRef PubMed
- 3. Temporiti F, Draghici I, Fusi S, et al. Does walking the day of total hip arthroplasty speed up functional independence? A non-randomized controlled study. Arch Physiother. 2020;10(1):8. CrossRef PubMed
- 4. Papalia R, Zampogna B, Torre G, et al. Preoperative and perioperative predictors of length of hospital stay after primary total hip arthroplasty – our experience on 743 cases. J Clin Med. 2021; 10(21):5053. CrossRef PubMed
- 5. Yang G, Chen W, Chen W, Tang X, Huang Y, Zhang L. Feasibility and safety of 2-day discharge after fast-track total hip arthroplasty: a Chinese experience. J Arthroplasty. 2016;31(8):1686-1692.e1. CrossRef PubMed
- 6. Fraser JF, Danoff JR, Manrique J, Reynolds MJ, Hozack WJ. Identifying reasons for failed same-day discharge following primary total hip arthroplasty. J Arthroplasty. 2018;33(12):3624-3628. CrossRef PubMed
- 7. Latham NK, Mehta V, Nguyen AM, et al. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89(11):2146-2155. CrossRef PubMed
- 8. Yeung TS, Wessel J, Stratford PW, MacDermid JC. The timed up and go test for use on an inpatient orthopaedic rehabilitation ward. J Orthop Sports Phys Ther. 2008;38(7):410-417. CrossRef PubMed
- 9. Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord 2005;6:3. CrossRef PubMed
- 10. Unver B, Baris RH, Yuksel E, Cekmece S, Kalkan S, Karatosun V. Reliability of 4-meter and 10-meter walk tests after lower extremity surgery. Disabil Rehabil. 2017;39(25):2572-2576. CrossRef PubMed
- 11. Doll H, Gentile B, Bush EN, Ballinger R. Evaluation of the measurement properties of four performance outcome measures in patients with elective hip replacements, elective knee replacements, or hip fractures. Value Health. 2018; 21(9):1104-1114. CrossRef PubMed
- 12. Halket A, Stratford PW, Kennedy DM, Woodhouse LJ, Spadoni G. Measurement properties of performance-specific pain ratings of patients awaiting total joint arthroplasty as a consequence of osteoarthritis. Physiother Can. 2008;60(3):255-263. CrossRef PubMed
- 13. Zukowski LA, Tennant JE, Iyigun G, Giuliani CA, Plummer P. Dual-tasking impacts gait, cognitive performance, and gaze behavior during walking in a real-world environment in older adult fallers and non-fallers. Exp Gerontol. 2021;150:111342. CrossRef PubMed
- 14. Olmos LE, Freixes O, Gatti MA, et al. Comparison of gait performance on different environmental settings for patients with chronic spinal cord injury. Spinal Cord. 2008;46(5):331-334. CrossRef PubMed
- 15. Schmitt AC, Baudendistel ST, Lipat AL, White TA, Raffegeau TE, Hass CJ. Walking indoors, outdoors, and on a treadmill: gait differences in healthy young and older adults. Gait Posture. 2021;90:468-474. CrossRef PubMed
- 16. Ciccarelli P, Urakcheeva I, Biondi A, Torre M. Italian Arthroplasty Registry. Annual Report 2021 – Addendum, 1st ed. Roma: Il pensiero scientifico editore, 2022; 29. Online (Accessed August 2024)
- 17. Loppini M, Longo UG, Caldarella E, Rocca AD, Denaro V, Grappiolo G. Femur first surgical technique: a smart non-computer-based procedure to achieve the combined anteversion in primary total hip arthroplasty. BMC Musculoskelet Disord. 2017;18(1):331. CrossRef PubMed
- 18. Temporiti F, De Leo D, Adamo P, et al. Impaired modulation of motor and functional performance in patients after total knee arthroplasty: a prospective observational study. BioMed Res Int. 2022;2022:4546836. CrossRef PubMed
- 19. Grant S, Aitchison T, Henderson E, et al. A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and Likert scales in normal subjects during submaximal exercise. Chest. 1999;116(5):1208-1217. CrossRef PubMed
- 20. Yuksel E, Unver B, Kalkan S, Karatosun V. Reliability and minimal detectable change of the 2-minute walk test and Timed Up and Go test in patients with total hip arthroplasty. Hip Int. 2021; 31(1):43-49. CrossRef PubMed
- 21. Ruspi A, De Leo D, Scandelli F, et al. Recommendations on the use of restrictions and assistive devices after total hip arthroplasty: an adolopment of guidelines. Disabil Rehabil. In press.
- 22. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101-110. CrossRef PubMed
- 23. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. CrossRef PubMed
- 24. Durlak JA. How to select, calculate, and interpret effect sizes. J Pediatr Psychol. 2009;34(9):917-928. CrossRef PubMed
- 25. van den Akker-Scheek I, Stevens M, Bulstra SK, Groothoff JW, van Horn JR, Zijlstra W. Recovery of gait after short-stay total hip arthroplasty. Arch Phys Med Rehabil. 2007;88(3):361-367. CrossRef PubMed
- 26. Kirschner J, Michel S, Becker R, et al. Determination of relationships between symmetry-based, performance-based, and functional outcome measures in patients undergoing total hip arthroplasty. J Pers Med 2023;13(7):1046. CrossRef PubMed
- 27. Lieberman JR, Dorey F, Shekelle P, et al. Differences between patients’ and physicians’ evaluations of outcome after total hip arthroplasty. J Bone Joint Surg Am. 1996;78(6):835-838. CrossRef PubMed
- 28. Dijkers MP, Kropp GC, Esper RM, Yavuzer G, Cullen N, Bakdalieh Y. Reporting on reliability and validity of outcome measures in medical rehabilitation research. Disabil Rehabil. 2002;24(16):819-827. CrossRef PubMed
- 29. Donovan K, Lord SE, McNaughton HK, Weatherall M. Mobility beyond the clinic: the effect of environment on gait and its measurement in community-ambulant stroke survivors. Clin Rehabil. 2008;22(6):556-563. CrossRef PubMed
- 30. Clark DJ, Rose DK, Ring SA, Porges EC. Utilization of central nervous system resources for preparation and performance of complex walking tasks in older adults. Front Aging Neurosci. 2014;6:217. CrossRef PubMed
- 31. Singh JA, Schleck C, Harmsen S, Lewallen D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord. 2016;17(1):256. CrossRef PubMed
- 32. Gooch K, Marshall DA, Faris PD, et al. Comparative effectiveness of alternative clinical pathways for primary hip and knee joint replacement patients: a pragmatic randomized, controlled trial. Osteoarthritis Cartilage. 2012;20(10):1086-1094. CrossRef PubMed