 |
Arch Physioter 2024; 14: 170-181 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3228 ORIGINAL RESEARCH ARTICLE |
 |
Effect of Pilates exercises on symptoms of irritable bowel syndrome in women: a randomized controlled trial
ABSTRACT
Objective: The treatment of irritable bowel syndrome (IBS) is challenging, calling for therapeutic strategies other than pharmacological treatment. Therefore, this study aimed to investigate the effects of Pilates exercises on IBS symptoms and severity, frequency of complete spontaneous bowel movements, fatigue, anxiety, depression, and body weight in women with IBS.
Methods: Sixty women with IBS, aged 20-45, completed this study. They were randomly assigned to two equal groups: a study group (n = 30) and a control group (n = 30). The study group received an 8-week Pilates exercise program (2 sessions per week) in addition to dietary advice, while the control group received dietary advice only. Inclusion criteria were women, IBS diagnosed based on Rome IV Diagnostic criteria, constipation-predominant IBS, and moderate to severe IBS. The outcome measures were the IBS severity scoring system (IBS-SSS), the frequency of complete spontaneous bowel movements, the modified fatigue impact scale (MFIS), hospital anxiety and depression (HADS) scale, and body weight (BW).
Results: The study group showed more significant improvements than the control group in total IBS-SSS score (Cohen d = 0.73, p < 0.001), frequency of complete spontaneous bowel movements (Cohen d = 0.50, p < 0.001), total MFIS score (Cohen d = 0.74, p < 0.001), anxiety (Cohen d = 0.56, p < 0.001), and depression (Cohen d = 0.64, p < 0.001). The study group also showed a significant reduction in body weight compared to baseline (p < 0.05). The control group showed significant improvements in all outcomes, except body weight, compared to baseline (p < 0.05).
Conclusion: Pilates exercises, used in addition to dietary advice, may significantly improve IBS symptoms and severity, frequency of complete spontaneous bowel movements, and alleviate fatigue, anxiety, and depression moderately more than dietary advice alone in women with constipation-predominant IBS. Nevertheless, dietary advice alone may also significantly improve these outcomes in this cohort.
Keywords: Anxiety/depression, Fatigue, Irritable bowel syndrome, Pilates exercises, Women
Received: July 26, 2024
Accepted: December 5, 2024
Published online: December 31, 2024
Trial registration
ClinicalTrials.gov, NCT05832801
Corresponding author:
Ahmad Mahdi
email: ahmed.mahdy@pt.cu.edu.eg
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What is already known about this topic
- Pilates exercises can relieve symptoms of fatigue, anxiety, and depression in several populations.
- There is a gap in the literature concerning the potential effect of Pilates exercises on the gastrointestinal and extra-gastrointestinal symptoms of irritable bowel syndrome (IBS).
What this study adds
- This is the first study to reveal the effectiveness of adding Pilates exercises to dietary advice as a lifestyle therapy in women with IBS.
- Pilate exercises added to dietary advice may offer more relief for IBS symptoms and clinically meaningful changes in IBS severity than dietary advice alone in women.
- Pilate exercises with dietary advice may increase the frequency of complete spontaneous bowel movements and reduce fatigue, anxiety, and depression to a greater extent than dietary advice alone in women with IBS.
Introduction
The incidence of irritable bowel syndrome (IBS) is 4.1% worldwide (1), with women being more affected than men (2). IBS with constipation is the most prevalent subtype of IBS and most commonly affects women with overweight and obesity (3). Frequent abdominal pain and annoying bloating associated with irregular bowel habits are the most common symptoms accompanying IBS (4). The frequency and extent of pain vary according to changes in bowel habits (4). Non-gastrointestinal symptoms such as fatigue, anxiety, and depression can also be present (5). The underlying cause of IBS is not yet clear but is known to be multifactorial, involving gut-brain axis dysfunction (6). Dysregulation of the gut-brain axis, a bidirectional pathway connecting the brain to the gut via the vagus nerve, may contribute to the perception of abdominal pain, discomfort, anxiety, and depression by the brain based on sensory input from the gut (3,7). Research has shown that managing IBS symptoms can be challenging (8). Since no established medical treatment can change IBS’s natural course (9), management plans have recently focused on pathophysiology and symptom relief (10). Dietary intervention is the first target therapy to alleviate IBS symptoms, as consuming particular foods can exacerbate symptoms (11). Additionally, Pilates exercises can have a potential role in relieving extra-gastrointestinal symptoms such as fatigue, anxiety, and depression (12).
To our knowledge, no prior research has assessed Pilates exercises’ effectiveness in managing patients with IBS. Thus, this study aimed to determine the effects of Pilates exercises in combination with dietary advice on IBS symptoms and severity, the frequency of complete spontaneous bowel movements, fatigue, anxiety and depression, and body weight compared to dietary advice alone in women with IBS. We hypothesized that Pilates exercises might influence the gastrointestinal symptoms of IBS based on the fact that they comprise a variety of postures combined with deep breathing, which can stimulate the vagal tone (13), thus optimizing the gastrointestinal tract (GIT) function and relieving constipation and associated symptoms. We also hypothesized that Pilates exercises might have positive effects on non-gastrointestinal symptoms of fatigue, anxiety, and depression associated with IBS based on two randomized trials in patients with multiple sclerosis (MS) (12) and post-menopausal women (14) and also based on a recent meta-analysis investigating the effect of Pilates exercises on depression in women with various medical conditions (e.g., MS, schizophrenia, chronic low back pain, type 2 diabetes, and breast cancer) (15). The results of this study may aid efforts targeting lifestyle approaches to improve the symptoms of IBS.
Methods
This study follows the CONSORT 2010 Statement Guidelines for reporting randomized controlled trials (16).
Study design and settings
This is a single-centered, parallel-group, randomized, controlled study. This study recruited patients by referral and continued from July 2023 to February 2024. The Ethics Committee of the senior author’s institution approved the study’s protocol (NO: P.T.REC/012/004218). This study has adhered to the Helsinki Declaration’s guidelines. Patients provided informed consent before the beginning of the study. The study was prospectively registered at ClinicalTrials.gov (registration No.: NCT05832801), and no changes were made to the protocol after the study commenced.
Randomization and concealed allocation
A simple randomization was employed with a 1:1 allocation ratio using a randomization table created by a computer software program. The allocation sequence was hidden using opaque, sealed envelopes with sequential numbers. The participants and the allocator were unaware of the upcoming allocation.
Implementation and blinding
The randomization sequence was generated by a researcher who was not involved in study interventions. Enrollment and assignment of subjects were performed by the physiotherapist involved in study interventions. For practical considerations, the assessor of the outcomes was not blinded to the allocation of subjects. Also, both the subjects and therapist were not blinded either to the dietary advice or the Pilates exercises due to the nature of the interventions.
Subjects
Sixty women with irritable bowel syndrome were recruited for this study by referral from a physician. Eligibility criteria were as follows: women aged 20-45 (i.e., the most common age for developing IBS) (17), a body mass index of 25-34.9 kg/m2 (i.e., IBS is mostly prevalent in overweight and obese subjects) (5,18), a diagnosis of IBS based on Rome IV Diagnostic criteria (4,19) constipation-predominant IBS established by a physician according to the Bristol stool form scale (20), and moderate-to-severe IBS (IBS severity score>174) (21). Exclusion criteria were organic gastrointestinal disorders, thyroid dysfunctions, concurrent cardiovascular, respiratory, renal, hepatic disorders, pregnancy, hematological disease, neurological/musculoskeletal problems, psychiatric disease, fibromyalgia, and previous history of stomach or intestinal excision. Eligible subjects were randomly assigned to a study group (Pilates and Dietary Advice) (n=30) and a control group (Dietary Advice) (n=30). Both groups received dietary advice without pharmacological treatment (e.g., laxatives).
Power analysis
A priori power analysis could not be performed due to the lack of similar studies in this research area. A post-hoc power analysis was conducted based on the total IBS-SSS score data from the present study using the G* Power software program (3.1.9.4). The post hoc power analysis revealed that 60 patients achieved 99% power at alpha = 0.05.
Evaluation
History taking and clinical evaluation
Thorough medical history-taking and clinical evaluation were performed for patient selection. The demographic, anthropometric, and clinical features of eligible patients were recorded at baseline. BMI was calculated at baseline by dividing body weight in kilograms by height in meters squared (22).
Outcome measures
The primary outcome measure was the IBS symptom severity scoring system (IBS-SSS). The secondary outcome measures were the number of complete spontaneous bowel movements, the modified fatigue impact scale (MFIS), the hospital anxiety and depression (HADS) scale, and body weight (BW).
Irritable Bowel Syndrome Severity Scoring System (IBS-SSS)
The IBS-SSS is a valid and reliable patient-based measure that evaluates the severity of IBS symptoms through five clinically significant items over ten days (21), as follows: (1) frequency and (2) severity of abdominal pain; (3) degree of abdominal distention or tightness; (4) dissatisfaction with bowel habits; and (5) affection of IBS on quality of life. A greater score denotes worse conditions. Each item is rated on a visual analog scale (VAS) from 0 to 100, resulting in an overall score ranging from 0 to 500 (21). Based on the data collected, the IBS-SSS scores are divided into three categories: mild symptoms (from 75 to 174), moderate symptoms (from 175 to 299), and severe symptoms (from 300 to 500) (21). Additionally, a 95-point reduction in total IBS-SSS scores is clinically meaningful, indicating an improvement in symptoms (23).
Frequency of complete spontaneous bowel movements
Complete spontaneous bowel movement is defined as a sense of complete evacuation without laxatives, enemas, or suppositories on the day of the bowel movement or the preceding day [24]. A participant with a weekly complete spontaneous bowel movement frequency rate of three or more and an increase of one or more from baseline is considered a responder [24]. The patients reported the number of their complete spontaneous bowel movements per week at baseline and post-intervention. The minimal clinically important change in the number of complete spontaneous bowel movements is 1.3 times per week for subjects suffering from functional constipation treated with acupuncture (25).
Modified Fatigue Impact Scale (MFIS)
This questionnaire measures the impact of exhaustion on life in subjects experiencing fatigue-like symptoms (26). The Arabic version of the questionnaire was used (27). The 21 items in the MFIS are divided into three categories: physical (nine items), cognitive (10 items), and psychosocial (two items). For all items, participants rate their agreement using a 5-point Likert scale, where 0 means “never” and 4 means “almost always.” The total score (0–84) comprises sub-scores for physical (0–36), cognitive (0–40), and psychosocial (0–8) functioning (26). A greater score is worse. The Arabic version of MFIS exhibited high reliability and concurrent validity in MS (27).
The Hospital Anxiety and Depression Scale (HADS)
To evaluate anxiety and depression, the Arabic version of the Hospital Anxiety and Depression Scale (HADS) was used (28). The Arabic version of HADS is a valid and reliable instrument (28). HADS has two subscales (i.e., anxiety and depression), and each subscale has 7 items. Each item is rated on a 4-point Likert scale (0-3) (29). Each subscale has a normal range of 0-7, a borderline range of 8-10, and a range denoting depression or anxiety of 11-21 (29). The minimal clinically important change is 1.17-2.13 for anxiety symptoms and 1.48-2.54 for depression symptoms (30).
Body weight
Body weight was measured at baseline and after 8 weeks.
Interventions
The interventions are reported following the TIDieR checklist (31).
Dietary/lifestyle advice
Dietary advice is an essential component in the management of IBS (32). Patients in both groups were instructed to follow dietary advice as per the guidelines from the National Institute for Health and Care Excellence (NICE) and the British Dietetic Association (BDA) (3334-35) for 8 weeks. The dietary pieces of advice are outlined in Table 1. A physician provided dietary advice through one face-to-face interview in a private clinic at the beginning of the study, and patients were instructed to report their diet using diaries. Then, compliance with the dietary advice was assessed regularly by a physiotherapist who checked patients’ diaries via the Watts-up application. All patients adhered to the dietary advice given. No modifications were made to the dietary advice throughout the study, as patients adhered well to the intervention.
| Dietary advice as per the guidelines from the National Institute for Health and Care Excellence (NICE) and the British Dietetic Association (BDA) (33-35). |
|---|
| Integrating a healthier eating habit, having food at the same time every day with regular intervals |
| Never eat too little or too much. |
| Staying properly hydrated |
| Preventing processed, fatty, and spicy food |
| Limiting caffeine, carbonated, and alcoholic drinks |
| Limiting fiber intake to soluble fibers starts with a low dose and builds up gradually. |
| Avoiding insoluble fibers, gas-producing foods like beans, and sweeteners |
| Awareness of dietary intolerance |
| An additional advice for increasing physical activity. |
Exercise Intervention
Pilates exercises may stimulate the vagal tone, thus enhancing the GIT function (13), and have a role in relieving fatigue, anxiety, and depression (12). Patients in the study group received Pilates exercises and dietary advice for eight weeks. The Pilates exercise program, modified from the protocol by Silva et al. (36), is described in Table 2. A mat and a gymnastic Swiss ball for adults were used. Initially, patients received instructions on the exercises and YouTube’s educational videos, as shown in Table 2. Then, an experienced physiotherapist guided the subjects in Pilates exercises through face-to-face sessions at a physiotherapy clinic. The sessions were scheduled two times per week for a total of 16 sessions. The sessions started with a 5-minute warm-up composed of repeated sit-ups and back extensions on a Swiss ball and 1 set of 30 seconds of hamstring stretch, knee to chest, and global stretch for trunk and back. The session ended with a 5-minute cool-down period with the same activities as the warm-up. The total session lasted for 45-50 minutes. From the 1st to the 3rd week, patients performed each exercise for one set of 8 repetitions that reached 10 repetitions by the end of the 4th week. From the 5th to the 8th week, two sets of 10 repetitions were performed. At this time, exercises were personalized so that the patients who couldn’t perform the two sets continually were allowed to rest for 3–5 minutes between sets. No adjustments were required, as every patient could complete the activities as directed. All patients in this group adhered to the scheduled sessions.
| Pilates exercises [modified from Silva et al. (36)] | Description |
|---|---|
| 1-Swan |
|
| 2-One leg up -down |
|
| 3- Leg circles |
|
| 4-Single leg stretch |
|
| 5-Saw |
|
| 6-Side kicks: front and back |
|
| 7-The hundred |
|
| 8-Pelvic lift on the ball |
|
| 9-Sit-ups with the ball. |
|
| 10-Stretching on the ball for muscle relaxation. |
|
Statistical analysis
Descriptive statistics were used to describe baseline patients’ characteristics (age, weight, height, BMI, IBS duration) as means ±SD. A two-way analysis of variance (ANOVA) was employed to compare outcome measures within and between groups. The chi-squared test was utilized to compare IBS-SSS severity categories between the groups after interventions. All statistical tests were set at a significance level of p < 0.05. Mean differences (MD) and 95% confidence interval (CI) were computed. The effect size was assessed by calculating the absolute mean changes from baseline (change scores) and the standardized mean difference between the two groups (Cohen d). Cohen d was interpreted as per Cohen [37], as <0.2= trivial effect; 0.2‐0.49 = small effect; 0.5‐0.79 = moderate effect; and ≥ 0.8= large effect. The change scores were calculated by subtracting the pre-intervention mean score from the post-intervention mean score. Mean percent changes were also calculated. Statistical Package for Social Sciences (SPSS) software version 24 was used for all analyses.
Results
Participants flow
Of 79 women with IBS, 15 did not fulfill the enrolment criteria, and 4 refused to participate. Sixty women with IBS were randomized to two groups: a study group (Pilates and Dietary Advice) (n = 30) and a control group (Dietary Advice) (n = 30). No losses occurred after randomization, and all participants in each group received the intended interventions and were included in the final analysis. The flow of participants can be seen in Figure 1. Eligible participants were recruited from July 2023 to February 2024.
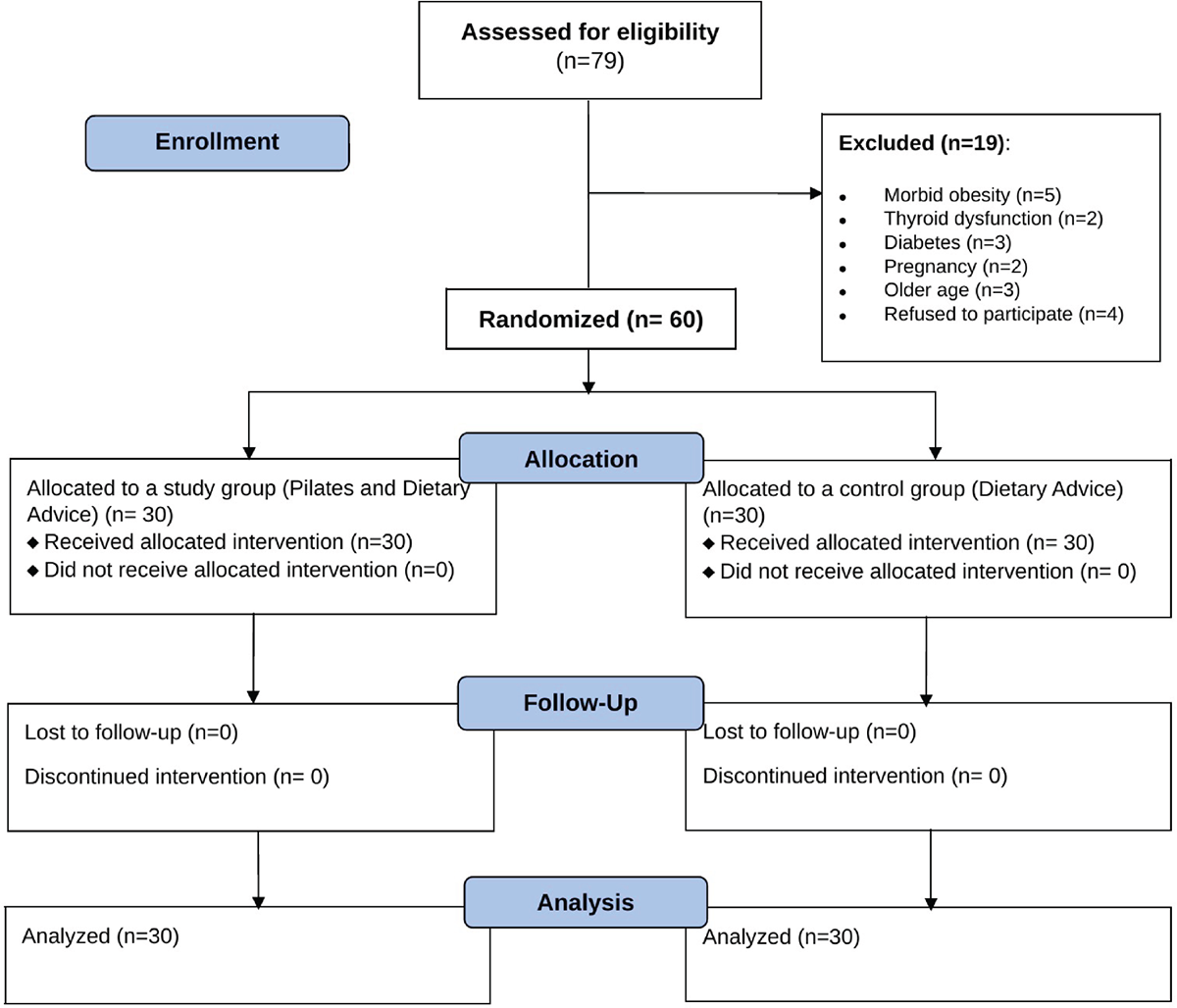
FIGURE 1 - Flowchart of the study.
Baseline data
The age and anthropometric and clinical characteristics of patients in the two groups are listed in Table 3.
Results of irritable bowel syndrome severity scoring system (IBS-SSS)
The total IBS-SSS displayed significant reductions in the study and control groups (p < 0.001) compared to the baseline (Table 4). However, the study group showed a more significant reduction in the total IBS-SSS score than the control group (p < 0.001), with a moderate effect size (Cohen d = 0.73) (Table 4). The percentage changes from baseline in total IBS-SSS were ↓66.75% versus ↓38.28% in the study and control groups, respectively (Table 4). Additionally, the severity of IBS was significantly lower in the study group than in the control group post-intervention (p<0.001) (i.e., 30 mild cases and 0 moderate cases in the study group versus 16 mild cases and 14 moderate cases in the control group) (Table 4).
Frequency of complete spontaneous bowel movements
The mean values of the frequency of complete spontaneous bowel movements showed a significant increase in the study and control groups (p < 0.001) compared to the baseline (Table 5). However, the study group presented a more significant increase in the frequency of complete spontaneous bowel movements than the control group (p < 0.001) with a moderate effect size (Cohen d = 0.5) (Table 5). The percentage changes in the frequency of complete spontaneous bowel movements were ↑97.17 % versus ↑67.69% in the study and control groups, respectively (Table 5).
Results of Modified Fatigue Impact Scale (MFIS)
The subscores of cognitive, physical, and psychosocial subscales of MFIS and the total score of MFIS reduced significantly in the study and control groups compared to baseline (p < 0.001) (Table 5). However, the study group showed significantly greater improvements in the MFIS total score (p < 0.001) than the control group with a moderate effect size (Cohen d = 0.74) (Table 5). The percentage changes in MFIS were ↓55.52% versus ↓28.83% in the study and control groups, respectively (Table 5).
Results of Hospital Anxiety and Depression Scale (HADS)
The mean values of anxiety and depression scores reduced significantly in the study and control groups compared to baseline (p < 0.001); however, the study group showed significantly more reductions in the mean scores of anxiety and depression with moderate effect sizes (d = 0.56, d = 0.64, respectively) than the control group (p < 0.001) (Table 5). The percent changes in anxiety were↓53.45% versus ↓27.64% in the study and control groups, respectively; and in depression, they were↓59.1% versus ↓26.33% in the study and control groups, respectively (Table 5).
Body weight (BW)
After interventions, BW displayed a significant reduction of 4.91% in the study group only (p <0.001), with no significant difference between the two groups (p=0.17) and trivial effect size (Cohen d=0.19) (Table 5).
| Variables | Study group
(Pilates and Dietary Advice) (n1 = 30) |
Control group
(Dietary Advice) (n2 = 30) |
|
|---|---|---|---|
| Age (Years) | 29.4 ± 7.66 | 30.33 ± 8.63 | |
| Body weight (kg) | 77.15 ± 11.16 | 77.63 ± 9.85 | |
| Height (cm) | 160.38 ± 5.57 | 161.32 ± 4.58 | |
| BMI (kg/m2) | 29.9 ± 3.23 | 29.73 ± 3.24 | |
| IBS Duration (Years) | 7.38 ± 5.95 | 7.22 ± 5.98 | |
| Total IBS-SSS score | 312.57 ± 80.1 | 283.7 ± 62.71 | |
| Severity | Moderate | 11 (36.66%) | 17(56.66%) |
| Severe | 19(63.33%) | 13(43.33%) | |
| Frequency of bowel movements | 2.47 ± 0.94 | 2.37 ± 0.89 | |
| Modified fatigue impact scale | 59.87 ± 9.72 | 58.27 ± 12.1 | |
| Anxiety | 13.47 ± 3.7 | 14 ± 3.3 | |
| Depression | 10.83 ± 2.59 | 11.13 ± 3.63 | |
Data are expressed as Means ± SD and frequencies (percent distribution). BMI: Body Mass Index; IBS: Irritable Bowel Syndrome; IBS-SSS: Irritable Bowel Syndrome Severity Scoring System
| IBS-SSS | Study group
(n1 = 30) |
Control group
(n2 = 30) |
MD | 95% CI | Effect size Cohen d |
p-value | ||
|---|---|---|---|---|---|---|---|---|
| Pain severity | Pre | 59.63 ± 19.75 | 59 ± 16.01 | 0.63 | (−8.66,9.93) | – | 0.89 | |
| Post | 21.47±10.37 | 39.37±16.07 | −17.9 | (−24.91, −10.89) | 0.67 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −38.16 | −19.79 | ||||||
| % Mean change | ↓64% | ↓33.27% | ||||||
| Pain duration | Pre | 66.33 ± 24.7 | 52.33±24.31 | 14 | (1.33,26.67) | – | 0.03** | |
| Post | 15 ± 6.3 | 28.33±19.67 | −13.3 | (−20.99, −5.68) | 0.46 | 0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −51.33 | −24 | ||||||
| % Mean change | ↓77.39% | ↓45.86% | ||||||
| Abdominal distention | Pre | 61.7 ± 24.03 | 42.23 ± 23.23 | 19.47 | (7.25,31.68) | – | 0.002** | |
| Post | 18.87 ± 15.49 | 30.67 ± 21.54 | −11.8 | (−21.49, −2.1) | 0.32 | 0.018** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −42.83 | -11.56 | ||||||
| % Mean change | ↓69.42% | ↓27.37% | ||||||
| Defecation satisfaction | Pre | 64.6 ± 25.91 | 62.9 ± 22.09 | 1.7 | (−10.74,14.14) | – | 0.79 | |
| Post | 24.53±15.34 | 36.1±16.32 | −11.5 | (−19.75, −3.38) | 0.36 | 0.006** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −40.07 | −26.8 | ||||||
| % Mean change | ↓62.03% | ↓42.61% | ||||||
| General QOL | Pre | 71.2 ± 18.51 | 67.23 ± 19.99 | 3.97 | (−5.99,13.92) | – | 0.43 | |
| Post | 24.4 ± 9.07 | 40.63 ±17.62 | −16.2 | (−23.53, -8.94) | 0.58 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −46.8 | −26.6 | ||||||
| % mean change | ↓65.73% | ↓39.57% | ||||||
| Total score | Pre | 312.57 ± 80.1 | 283.7 ± 62.71 | 28.87 | (−8.31,66.04) | – | 0.13 | |
| Post | 103.93 ± 27.95 | 175.10 ± 62.80 | −71.1 | (−96.53, −45.8) | 0.73 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −208.64 | −108.6 | ||||||
| % mean change | ↓66.75% | ↓38.28% | ||||||
Severity (based on IBS-SSS total score) |
Post | Mild | 30 (100%) | 16(53.33%) | <0.001¶ | |||
| Moderate | 0 (0%) | 14(46.66%) | ||||||
Data are expressed as Means ± SD, change scores and percent mean changes from baseline, and frequencies and percent distributions. IBS-SSS: Irritable Bowel Syndrome Severity Scoring System; QOL: Quality of life; MD: mean difference; CI: confidence interval. *Significant p-value (p < 0.05) based on the two-way ANOVA within-group comparison; **significant p-value (p < 0.05) based on the two-way ANOVA between-groups comparison; ¶ significant p-value (p < 0.05) based on Chi-square test.
| Outcomes | Study group
(n1 = 30) |
Control group
(n2 = 30) |
MD | 95% CI | Effect size Cohen d |
p-value | ||
|---|---|---|---|---|---|---|---|---|
| Frequency of bowel movements | Pre | 2.47 ± 0.94 | 2.37 ± 0.89 | 0.1 | (−0.37,0.57) | – | 0.67 | |
| Post | 4.87 ± 1.04 | 3.77 ± 1.44 | 1.1 | (0.54,1.66) | 0.5 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | 2.4 | 1.4 | ||||||
| % Mean change | ↑97.17% | ↑67.69% | ||||||
Modified fatigue impact scale (MFIS) |
Cognitive | Pre | 26.83 ± 5.87 | 26.37 ± 5.37 | 0.47 | (−2.6,3.53) | – | 0.76 |
| Post | 12.83 ± 5.02 | 18.13 ± 6.12 | −5.3 | (−8.19, −2.41) | 0.47 | 0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −14 | −8.24 | ||||||
| % Mean change | ↓52.18% | ↓31.25% | ||||||
| Physical | Pre | 26.77 ± 5.19 | 26.53 ± 6 | 0.23 | (−2.67,3.13) | – | 0.87 | |
| Post | 11.83 ± 2.1 | 18.9 ± 4.44 | −7.0 | (−9.54, −4.6) | 0.74 | 0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −14.94 | –7.63 | ||||||
| % Mean change | ↓55.81% | ↓28.76% | ||||||
| Psychosocial | Pre | 5.83 ± 1.34 | 5.37 ± 1.54 | 0.47 | (−0.28,1.2) | – | 0.22 | |
| Post | 1.97 ± 1.38 | 4.3 ± 1.66 | −2.3 | (−3.12, −1.54) | 0.78 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −3.86 | –1.07 | ||||||
| % Mean change | ↓69.3% | ↓19.93% | ||||||
| Total | Pre | 59.87 ± 9.72 | 58.27 ± 12.1 | 1.6 | (−4.07,7.27) | – | 0.57 | |
| Post | 26.63 ± 9.48 | 41.47 ± 10.43 | −14.8 | (−19.98, −9.68 | 0.74 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −33.23 | −16.8 | ||||||
| % Mean change | ↓55.52% | ↓28.83% | ||||||
| Hospital Anxiety and Depression Scale (HADS) | Anxiety | Pre | 13.47 ± 3.7 | 14 ± 3.3 | −0.5 | (−2.35,1.28) | – | 0.56 |
| Post | 6.27 ± 2.7 | 10.13 ± 3.94 | −3.8 | (−5.66, −2.08) | 0.56 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −7.2 | −3.87 | ||||||
| % Mean change | ↓53.45% | ↓27.64% | ||||||
| Depression | Pre | 10.83 ± 2.59 | 11.13 ± 3.63 | −0.3 | (−1.93,1.33) | – | 0.71 | |
| Post | 4.43 ± 2.6 | 8.2 ± 3.27 | −3.7 | (−5.29, −2.24) | 0.64 | <0.001** | ||
| p-value | <0.001* | <0.001* | ||||||
| Change score | −6.4 | −2.93 | ||||||
| % Mean change | ↓59.1% | ↓26.33% | ||||||
| Body weight (kg) | Pre | 77.15 ± 11.16 | 77.63 ± 9.85 | −0.48 | (−5.92, 4.96) | – | 0.86 | |
| Post | 73.36 ± 10.27 | 77.08 ± 10.24 | −3.72 | (−9.02, 1.57 | 0.19 | 0.17 | ||
| p-value | <0.001* | 0.15 | ||||||
| Change score | −3.79 | −0.55 | ||||||
| % Mean change | ↓4.91% | ↓0.71% | ||||||
Data are expressed as Mean ± SD and percent mean changes from baseline. MD: mean difference, CI: confidence interval; *Significant p-value (p < 0.05) based on the two-way ANOVA within-group comparison; **significant p-value (p < 0.05) based on the two-way ANOVA between-groups comparison
Discussion
The purpose of the study was to investigate the effect of Pilates exercises on IBS severity scoring system assessed by IBS-SSS, the number of complete spontaneous bowel movements, fatigue assessed by MFIS, anxiety, and depression assessed by HADS, and body weight (BW) in women with constipation-predominant IBS. To our knowledge, this study is the first randomized control trial that investigates the effectiveness of Pilates exercises in IBS. The main findings of this study are: (i) women with constipation-predominant IBS who received Pilates exercises in addition to dietary advice for IBS showed significantly greater improvements in IBS symptoms and severity as assessed by the IBS-SSS, with a moderate effect size in its total score, than their counterparts who received dietary advice only; (ii) Pilates exercises in combination with dietary advice led to a significantly higher frequency of complete spontaneous bowel movements, less fatigue as assessed by MFIS, and lower anxiety and depression levels as assessed by HADS with moderate effect sizes than dietary advice alone in women with constipation-predominant IBS, (iii) body weight was reduced significantly only following Pilates exercises and dietary advice compared to the baseline value.
This study showed that pilates exercises, in addition to dietary advice, showed more significant improvement in the IBS symptoms/severity assessed by IBS-SSS (i.e., pain duration, pain severity, abdominal distension, defecation satisfaction, and general QoL) than dietary advice alone. In a similar context, Fani et al. (38) revealed that six weeks of aerobic exercises significantly improved the severity of IBS symptoms. Interestingly, the change scores in total IBS-SSS scores in the study and control groups were 208.64 and 108.6 points, respectively, representing clinically important changes, as a 95-point reduction in total IBS-SSS scores is clinically meaningful (23). However, there was a difference in clinical significance in the improvements of IBS-SSS between the two groups in favor of the study group. This is because all patients in the study group had mild symptoms after the interventions, in contrast to 16 patients with mild symptoms and 14 patients with moderate symptoms in the control group post-intervention. Moreover, there was a significant difference with a moderate effect size in the improvement of IBS-SSS total score between the groups in favor of the study group (i.e., Cohen d = 0.73).
Another finding in this study was that the self-reported frequency of complete spontaneous bowel movements per week increased by a significantly greater degree in patients who received Pilates exercises and dietary advice than in patients who received dietary advice alone. This finding complements the previous findings in this study (i.e., the improvement in IBS symptoms and severity). Also, this study reveals the effectiveness of Pilates exercises in treating symptoms of constipation in our patients who had constipation-predominant IBS. In a similar context, Daley et al. (39) showed that exercise can significantly improve constipation symptoms compared to usual care in patients with IBS. Additionally, Gao et al. (40), in their systematic review, concluded that exercise can have a major role in alleviating constipation symptoms. The mechanism underlying the constipation-relieving effect of Pilates exercises is that Pilates has the advantage of combining deep breathing with body movements, which can activate the vagal tone (13). Within this, Liu et al. (41) reported that 6 weeks of slow deep breathing exercises improved the number of bowel movements compared to the control group, which can be attributed to improvement in the parasympathetic activity in patients with constipation-predominant IBS. Worth noting is that Ai et al. (25) reported that a mean increase of ≥1.3 times/week in complete spontaneous bowel movement in patients with severe functional constipation treated with acupuncture suggests clinical significance. Given that the mean increases (change scores) in the frequency of complete spontaneous bowel movements were 2.4 and 1.4 times per week, the changes in this outcome may be of clinical importance in both groups. However, there was a significant difference with a moderate effect size in the improved frequency of complete spontaneous bowel movements between the groups in favor of the study group (Cohen d = 0.50).
The current study also showed that Pilates exercises and dietary advice improved overall fatigue symptoms (i.e., cognitive, physical, and psychosocial) compared to the baseline and dietary advice alone. In the present study, the mean changes (i.e., change scores) in total MFIS scores were 33.23 and 16.8 points in the study and control group, respectively. Alawami and Abdulla (42) reported that a mean change of 14.68 or more points in total MFIS score may indicate a minimal detectable change (MDC) in fatigue of clinical importance in patients with MS. Although this MDC in fatigue, assessed by MFIS, was investigated in MS, we think this threshold value may help interpret the changes in fatigue assessed by MFIS in response to our interventions. Nevertheless, there was a significant difference with a moderate effect size in the improvement of MFIS total score between groups in favor of the study group (Cohen d = 0.74).
Pilates exercises played a role in the enhancement of fatigue symptoms in patients with MS (12,43,44), healthy young female participants (45,46), post-menopausal women (14,47), and women with breast cancer (48). A recent meta-analysis reported that moderate aerobic exercises or combination training approaches for 2-10 weeks positively affected fatigue in subjects suffering from chronic conditions (49). In contrast, Johannesson et al. (50) demonstrated that moderate physical activity did not enhance fatigue symptoms in patients with IBS.
This study also showed that more significant improvements in anxiety and depression were found in the study group than in the control group. This finding can be supported by a recent systematic review by Ju et al. (15), which showed that Pilates exercises can be considered an additional treatment method for alleviating depression and anxiety symptoms in female patients. In addition, Pilates was effective in improving anxiety and depression symptoms in women with type 2 diabetes (51), middle-aged women with obesity (52), and post-menopausal women (53). On the other hand, some studies reported that Pilates exercises did not lead to any significant improvement in anxiety or depression in female patients with fibromyalgia (54) or dysmenorrhea (55). It is worth noting that changes in HADS anxiety symptoms of 1.17-2.13 points and in HADS depression symptoms of 1.48-2.54 points were considered clinically important in patients with chronic pain (30). The change scores in HADS anxiety and depression symptoms in both groups in the present study were greater than those cut-off values, suggesting clinically meaningful improvements. However, there were significant differences with moderate effect sizes in the improvement of HADS anxiety symptoms (Cohen d = 0.56) and HADS depression symptoms (Cohen d = 0.64) between groups in favor of the study group.
The positive effects of Pilates on IBS symptoms, fatigue, anxiety, and depression may be explained based on the fact that Pilates can activate the parasympathetic nervous system and optimize the function of the hypothalamic-pituitary-adrenal axis, which regulates several body processes, including digestion, mood, and emotions, energy storage, and production (52,56,57). It should also be noted that the control group, which received dietary advice, only showed significant improvement in IBS symptoms, frequency of complete spontaneous bowel movements, anxiety, and depression compared to baseline. This may be because the diet they received could have modulated gut flora composition and function, thus optimizing the gut-brain axis pathway and reducing the brain’s perception of abdominal pain, discomfort, and anxiety [58]. As such, it may be unsurprising that the patients who received both Pilates exercises and dietary advice experienced greater improvements in their IBS symptoms than those who received dietary advice alone, owing to the combined effects of both interventions.
The last finding in this study was that the study group showed a significant reduction in body weight compared to the baseline value. Pilates effectively reduced body weight in subjects with overweight or obesity (59,60), MS (44), young women (46), women with type 2 diabetes (51), and post-menopausal women (53). On the contrary, a study by Park et al. (52) reported that Pilates exercises did not cause any change in body weight in female participants with obesity. Also, the meta-analysis by Cavina et al. (61) reported that mat Pilates had no advantage over the control condition for reducing body weight in the general population. Interestingly, the mean percent change in body weight from baseline in the study group was approximately 4.91%, and this reduction could be of clinical relevance. It was shown that a weight reduction of 5% from baseline is “clinically meaningful” (62) and is associated with a decline of 13% in intra-hepatic triglycerides (63). Elevated triglyceride levels were found to exaggerate IBS symptoms (64).
Finally, this study has limitations, and its findings should be interpreted in that context. There was a lack of control over potential hormonal factors (e.g., effects of menstrual cycles or use of contraceptive pills). Also, the current study only included women with overweight and grade I obesity suffering from constipation-predominant IBS, which may limit the generalization of the results. Moreover, this study did not include abdominal circumference or other metrics of obesity. Nevertheless, the current study has several strengths. This study is the first to investigate the effectiveness of Pilates exercises in women with IBS. Additionally, a variety of patient-reported outcomes were used in this study to produce an extensive assessment of the patients at baseline and in response to the interventions. Moreover, the results of this study may have practical applications for physiotherapists and healthcare providers interested in the complementary treatment of IBS.
Conclusion
When used in tandem with dietary advice, Pilates exercises may be an effective therapeutic intervention that could significantly reduce IBS symptoms and severity, increase the frequency of complete spontaneous bowel movements, reduce fatigue, and relieve anxiety and depression to a more moderate extent than dietary advice alone in women with IBS. However, dietary advice alone may also improve these outcomes in these patients.
Disclosures
Financial support: No funding was received for this research.
Conflict of interest: The authors declare no conflict of interest.
References
- 1. Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99-114.e3. CrossRef PubMed
- 2. Kim YS, Kim N. Sex-gender differences in irritable bowel syndrome. J Neurogastroenterol Motil. 2018;24(4):544-558. CrossRef PubMed
- 3. Galica AN, Galica R, Dumitrascu DL. Epidemiology of irritable bowel syndrome in Albania. J Gastrointestin Liver Dis. 2021;30(3):334-338. CrossRef PubMed
- 4. Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393-1407. CrossRef PubMed
- 5. Frändemark Å, Jakobsson Ung E, Törnblom H, et al. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017;29(1):e12898. CrossRef PubMed
- 6. Tang HY, Jiang AJ, Wang XY, et al. Uncovering the pathophysiology of irritable bowel syndrome by exploring the gut-brain axis: a narrative review. Ann Transl Med. 2021;9(14):1187. CrossRef PubMed
- 7. Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome. Mol Psychiatry. 2023;28(4):1451-1465. CrossRef PubMed
- 8. Ford AC, Lacy BE, Talley NJ. Irritable bowel syndrome. N Engl J Med. 2017;376(26):2566-2578. CrossRef PubMed
- 9. Ford AC, Sperber AD, Corsetti M, et al. Irritable bowel syndrome. Lancet. 2020;396(10263):1675-1688. CrossRef PubMed
- 10. D’Silva A, MacQueen G, Nasser Y, et al. Yoga as a therapy for irritable bowel syndrome. Dig Dis Sci. 2020;65(9):2503-2514. CrossRef PubMed
- 11. Portincasa P, Bonfrate L, de Bari O, et al. Irritable bowel syndrome and diet. Gastroenterol Rep (Oxf). 2017;5(1):11-19. CrossRef PubMed
- 12. Fleming KM, Coote SB, Herring MP. Home-based Pilates for symptoms of anxiety, depression and fatigue among persons with multiple sclerosis: an 8-week randomized controlled trial. Mult Scler. 2021;27(14):2267-2279. CrossRef PubMed
- 13. Yoo KT. Effects of mat Pilates on the autonomic nervous system in the elderly women. J Korean Soc Phys Med. 2022;17(4):27-35. CrossRef
- 14. Aibar-Almazán A, Hita-Contreras F, Cruz-Díaz D, et al. Effects of Pilates training on sleep quality, anxiety, depression and fatigue in post-menopausal women: a randomized controlled trial. Maturitas. 2019;124:62-67. CrossRef PubMed
- 15. Ju M, Zhang Z, Tao X, et al. The impact of Pilates exercise for depression symptoms in female patients: a systematic review and meta-analysis. Medicine (United States). 2023;102(41): E35419. CrossRef
- 16. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. J Pharmacol Pharmacother. 2010;1(2):100-107. CrossRef PubMed
- 17. Hadjivasilis A, Tsioutis C, Michalinos A, et al. New insights into irritable bowel syndrome: from pathophysiology to treatment. Ann Gastroenterol. 2019;32(6):554-564. CrossRef PubMed
- 18. Pickett-Blakely O. Obesity and irritable bowel syndrome: a comprehensive review. Gastroenterol Hepatol (N Y). 2014;10(7):411-416. PubMed
- 19. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150(6):1262-1279. CrossRef
- 20. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920-924. CrossRef PubMed
- 21. Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395-402. CrossRef PubMed
- 22. Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50(3):117-128. CrossRef PubMed
- 23. Spiegel B, Bolus R, Harris LA, et al. Measuring irritable bowel syndrome patient-reported outcomes with an abdominal pain numeric rating scale. Aliment Pharmacol Ther. 2009;30(11-12):1159-1170. CrossRef PubMed
- 24. Cao H, Wang Y, Su J, Zhao H, Han M, Liu JP. Acupuncture for chronic constipation. Cochrane Database Syst Rev. 2023;2023(4):CD004117. PubMed
- 25. Ai YK, Liu ZS, Liu BY, et al. Minimal clinically important difference of the frequency of bowel movement for patients with chronic severe functional constipation treated with acupuncture. Zhongguo Zhenjiu. 2022;42(11):1247-1250. Chinese. PubMed
- 26. Fatigue guidelines development panel of the Multiple Sclerosis Council for clinical practice guidelines. Fatigue and multiple sclerosis. Evidence-based management strategies for fatigue in multiple sclerosis. Paralyzed Veterans of America; 1998. Online
- 27. Khalil H, Al-Shorman A, Alghwiri AA, et al. Cross cultural adaptation and psychometric evaluation of an Arabic version of the modified fatigue impact scale in people with multiple sclerosis. Mult Scler Relat Disord. 2020;39:101878. CrossRef PubMed
- 28. Terkawi AS, Tsang S, AlKahtani GJ, et al. Development and validation of Arabic version of the Hospital Anxiety and Depression Scale. Saudi J Anaesth. 2017;11(5)(suppl 1):S11-S18. CrossRef PubMed
- 29. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983Jun;67(6):361-70. CrossRef PubMed
- 30. Grönkvist R, Vixner L, Äng B, et al. Measurement error, minimal detectable change, and minimal clinically important difference of the Short Form-36 Health Survey, Hospital Anxiety and Depression Scale, and Pain Numeric Rating Scale in patients with chronic pain. J Pain. 2024;25(9):104559. CrossRef PubMed
- 31. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348(mar07 3):g1687. CrossRef PubMed
- 32. Jayasinghe M, Karunanayake V, Mohtashim A, et al. The role of diet in the management of irritable bowel syndrome: a comprehensive review. Cureus. 2024;16(2):e54244. CrossRef PubMed
- 33. National Institute for Health and Clinical Excellence (NICE). Irritable bowel syndrome in adults. Diagnosis and management of irritable bowel syndrome in primary care. Clinical Guideline 61 Update 2017. Online (Accessed July 2024)
- 34. McKenzie YA, Bowyer RK, Leach H, et al. IBS Dietetic Guideline Review Group on behalf of Gastroenterology Specialist Group of the British Dietetic Association. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016;29(5):549-575. CrossRef PubMed
- 35. Vasant DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214-1240. CrossRef PubMed
- 36. Silva HJA, Lins CAA, Nobre TTX, et al. Mat Pilates and aquatic aerobic exercises for women with fibromyalgia: a protocol for a randomized controlled blind study. BMJ Open. 2019;9(2):e022306. CrossRef PubMed
- 37. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Routledge; 1988. CrossRef
- 38. Fani M, Mostamand J, Fani M, et al. The effect of aerobic exercises among women with mild and moderate irritable bowel syndrome: a pilot study. J Bodyw Mov Ther. 2019;23(1):161-165. CrossRef PubMed
- 39. Daley A, Grimmett C, Roberts L, et al. The effects of exercise upon symptoms and quality of life in patients diagnosed with irritable bowel syndrome: a randomized controlled trial. J Sci Med Sport. 2010;12(2):E49. CrossRef
- 40. Gao R, Tao Y, Zhou C, et al. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scand J Gastroenterol. 2019;54(2):169-177. CrossRef PubMed
- 41. Liu J, Lv C, Wang W, et al. Slow, deep breathing intervention improved symptoms and altered rectal sensitivity in patients with constipation-predominant irritable bowel syndrome. Front Neurosci. 2022;16:1034547. CrossRef PubMed
- 42. Alawami AS, Abdulla FA. Psychometric properties of an Arabic translation of the modified fatigue impact scale in patients with multiple sclerosis. Disabil Rehabil. 2021;43(22):3251-3259. CrossRef PubMed
- 43. Miri H, Mehrabian H, Peyvandi MG, et al. Effect of pilates training on balance, muscular endurance, fatigue, and quality of life among women with multiple sclerosis. Health, Sport. Rehabilitation (Stuttg). 2023;9(4):73-84. Online
- 44. Eftekhari E, Etemadifar M. Impact of clinical mat Pilates on body composition and functional indices in female patients with multiple sclerosis. View project. Crescent J Med Biol Sci. 2018;5(4):297-305. Online
- 45. Amzajerdi A, Keshavarz M, Ezati M, et al. The effect of Pilates exercises on sleep quality and fatigue among female students dormitory residents. BMC Sports Sci Med Rehabil. 2023;15(1):67. CrossRef PubMed
- 46. Akbaş E, Ünver B. A six-week pilates exercise protocol for improving physical and mental health-related parameters. Malaysian J Movement. Healthc Exec. 2018;7(2):65-79.
- 47. Mohamed DMA, Hussien AMN, Kamel HEDH, et al. Effect of Pilates exercises on fatigue in post-menopausal women. Bull Fac Phys Ther. 2023;28(1):4-9. CrossRef
- 48. Eyigor S, Karapolat H, Yesil H, et al. Effects of pilates exercises on functional capacity, flexibility, fatigue, depression and quality of life in female breast cancer patients: a randomized controlled study. Eur J Phys Rehabil Med. 2010;46(4):481-487. PubMed
- 49. Barakou I, Sakalidis KE, Abonie US, et al. Effectiveness of physical activity interventions on reducing perceived fatigue among adults with chronic conditions: a systematic review and meta-analysis of randomized controlled trials. Sci Rep. 2023;13(1):14582. CrossRef PubMed
- 50. Johannesson E, Simrén M, Strid H, et al. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2011;106(5):915-922. CrossRef PubMed
- 51. Alizadeh R, Zolfaghari Z, Nosratzehi S, et al. Effect of Pilates on anxiety, depression, and anthropometric indices of women with type 2 diabetes. Medical-Surgical Nursing Journal. 2023;12(2):e143695. CrossRef
- 52. Park HY, Jung K, Jung WS, et al. Effects of online Pilates and face-to-face Pilates intervention on body composition, muscle mechanical properties, cardiometabolic parameters, mental health, and physical fitness in middle-aged women with obesity. Healthcare (Basel). 2023;11(20):2768. CrossRef PubMed
- 53. Farzaneh A, Koushkie Jahromi M, Salesi M, Rostami R. The ameliorating impact of pilates training on anxiety and body mass index in menopausal symptoms. Womens Health Bull. 2020;7(4):46-53. Online
- 54. Komatsu M, Avila MA, Colombo MM, et al. Pilates training improves pain and quality of life of women with fibromyalgia syndrome. Rev Dor. 2016;17(4):274-278. CrossRef
- 55. Song BH, Kim J. Effects of Pilates on pain, physical function, sleep quality, and psychological factors in young women with dysmenorrhea: a preliminary randomized controlled study. Healthcare (Basel). 2023;11(14):2076. CrossRef PubMed
- 56. Najafi P, Hadizadeh M, Cheong JPG, et al. Effects of Tele-Pilates and Tele-Yoga on biochemicals, physical, and psychological parameters of females with multiple sclerosis. J Clin Med. 2023;12(4):1585. CrossRef PubMed
- 57. Robayo A. Hypotalamus-Pituitary-Adrenal (HPA) Axes and Their Relationship with Stress, Mood, Personality, and Neurocognitive Functioning. In: Lopez-Soto T, Garcia-Lopez A, Salguero-Lamillar FJ, eds. The Theory of Mind Under Scrutiny: Psychopathology, Neuroscience, Philosophy of Mind and Artificial Intelligence. Springer Nature Switzerland; 2024:341-365.
- 58. Ribeiro G, Ferri A, Clarke G, et al. Diet and the microbiota - gut - brain-axis: a primer for clinical nutrition. Curr Opin Clin Nutr Metab Care. 2022;25(6):443-450. CrossRef PubMed
- 59. Hushmandi K, Jamali J, Saghari S, et al. The effect of eight weeks of pilates exercises on anthropometric indices and subjective well-being in obese middle-aged women. Open Public Health J. 2023;16(1):1-8. CrossRef
- 60. Wang Y, Chen Z, Wu Z, et al. Pilates for overweight or obesity: a meta-analysis. Front Physiol. 2021;12:643455. CrossRef PubMed
- 61. Cavina APS, Pizzo Junior E, Machado AF, et al. Effects of the mat Pilates method on body composition: systematic review with meta-analysis. J Phys Act Health. 2020;17(6):673-681. CrossRef PubMed
- 62. Williamson DA, Bray GA, Ryan DH. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity (Silver Spring). 2015;23(12):2319-2320. CrossRef PubMed
- 63. Magkos F, Fraterrigo G, Yoshino J, et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016 Apr 12;23(4):591-601. CrossRef PubMed
- 64. Xu M, Liu D, Tan Y, et al. A Mendelian randomization study on the effects of plasma lipids on irritable bowel syndrome and functional dyspepsia. Sci Rep. 2024;14(1):78. CrossRef PubMed