 |
Arch Physioter 2025; 15: 1-8 ISSN 2057-0082 | DOI: 10.33393/aop.2025.3188 REVIEW |
 |
Coronavirus Disease 2019 (COVID-19) and pelvic floor signs and symptoms: a scoping review of the literature
ABSTRACT
Introduction: The Coronavirus Disease 2019 (COVID-19) pandemic presents a substantial global health challenge. While the disease is known to impact multiple systems, leading to long-term consequences that require monitoring and rehabilitation, its effects on the pelvic floor remain unclear.
This study aims to explore COVID-19-related signs and symptoms affecting pelvic floor functions through a scoping review.
Methods: We conducted a scoping review following the Arksey and O’Malley framework. A systematic search was performed in PubMed, CINAHL, and Embase databases up to March 19, 2024, to identify studies examining pelvic floor-related signs and symptoms in COVID-19 patients. Two independent reviewers extracted the study and participant characteristics, areas involved (e.g., anorectal, sexual, urogenital), and signs and symptoms using an ad-hoc data extraction form. Signs and symptoms were classified as direct (e.g., directly impacting the pelvic floor) or indirect (e.g., indirectly affecting the pelvic floor with potential long-term consequences).
Results: We included 104 studies, primarily a systematic review (N = 40; 38.46%) and focused on adult populations (N = 80; 76.92%), investigating 140 signs and symptoms from various regions worldwide. Most (N = 124; 88.57%) were indirect signs and symptoms, while the minority were direct (N = 16; 11.43%). The most prevalent indirect symptom was diarrhea (n = 81; 70,43%) in the anorectal bowel area (n = 115). The most prevalent direct were lower urinary tract symptoms (LUTS) (n = 16; 84.21%) in the urogenital area (n = 19).
Conclusion: This study highlights the significant prevalence of both direct and indirect pelvic floor symptoms in COVID-19 patients. Clinicians should be aware of the potential link between COVID-19 and pelvic floor dysfunction.
Keywords: Anorectal bowel symptoms, COVID-19, Lower urinary tract symptoms, Pelvic floor, Sexual dysfunction
Received: July 1, 2024
Accepted: December 20, 2024
Published online: January 20, 2025
This article includes supplementary material
Corresponding author:
Arianna Bortolami
email: arianna.bortolami@gmail.com
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2025 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What is already known about this topic:
- The COVID-19 pandemic has resulted in death or temporary, permanent, or progressively worsening consequences for many people. Although the disease is known to affect many systems, its effects on the pelvic floor remain unclear.
What does the study add:
- This review maps the literature on the prevalence of COVID-19 symptoms affecting pelvic floor functions. Clinicians should be aware of the potential link between COVID-19 and pelvic floor dysfunction.
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has determined, in addition to the death of many people, temporary, permanent, or progressively worsening consequences (1,2). An abundance of literature exists on respiratory system affections after COVID-19, but more information on other physiologic complications has yet to be published so far. It has been reported that the COVID-19 virus uses the angiotensin-converting enzyme 2 (ACE2) as a host cell receptor, impacting not only the respiratory system but also the digestive system and the bladder (3). The respiratory symptoms of COVID-19, such as coughing and shortness of breath, cause an increase in intra-abdominal pressure that might develop pelvic floor under activity, contributing to the onset or worsening of urinary or fecal incontinence and/or pelvic organ prolapse. Furthermore, surviving people after a long-term hospitalization due to COVID-19 with a post-intensive care syndrome might have consequences on sexual, bowel, and bladder functioning (4). Thus, there could be signs and symptoms directly or indirectly related to the pelvic floor: the muscular and connective part that coincides with the genito-urinary-anal area, such as urinary and fecal incontinence and urgency, difficulty emptying of bladder and rectum, pelvic organ prolapse, sexual dysfunction and chronic pelvic pain (5,6).
The pathophysiological hypothesis for DIRECT symptoms correlates to a condition of systemic inflammation characterized by a cytokine cascade that amplifies the flogosis of pelvic structures (7). This inflammatory process can lead to specific symptoms of pelvic floor dysfunction, such as lower urinary tract symptoms (LUTS). These symptoms may manifest as difficulties in urination, urgency, and pain, highlighting the significant impact that the infection can have on urogenital health (8,9). Additionally, patients who have contracted COVID-19 may suffer from musculoskeletal or neuropathic pain or have had their chronic pain symptoms exacerbated by the virus. This can also include the pelvis, pelvic floor, and pudendal nerve (10).
For INDIRECT symptoms, the pathophysiology is related to: (a) cough and dyspnea of inducing incontinence, symptoms of the bladder and rectal filling phase (9), alterations of pelvic statics (12); (b) sexual dysfunctions (13); and (c) alterations of intestinal functionality, such as diarrhea that can generate anal incontinence and fecal urgency, and constipation with involvement of the pelvic floor. Additionally, the presence of inflammation and consequent pelvic pain, along with neuropathy of the pudendal nerve, contribute to these indirect symptoms.
However, health professionals often underestimate these signs and symptoms. Nevertheless, pelvic floor dysfunctions also have a significant role in worsening the quality of life of people, leading to sensations such as embarrassment, anxiety, depression, loneliness, alteration of the body pattern, lack of freedom due to the frequent need for the toilet, unsatisfactory sexuality, impossibility of procreation, impossibility of sitting position and fear of movement as in the case of pelvic pain chronic (14). Women and men affected by pelvic floor dysfunctions could represent an economic burden for the health system, both from direct financial costs derived from healthcare assistance, complications, psychological assistance, and the use of hygiene devices (e.g., pads), as well as indirect costs, derived from absenteeism and lost productivity (15,16,17).
During the COVID-19 pandemic, hospitals and clinics were particularly affected by a massive reduction of outpatient investigations, which reduced the access to care for patients suffering from pelvic floor dysfunctions (18). Therefore, signs and symptoms might not have been adequately reported due to the organizational limitations posed by the pandemic. Thus, given the insufficient literature on this topic, our scoping review aimed to fill the gap, mapping what was published on the topic and exploring possible direct and indirect signs correlated to the pelvic floor to investigate with research.
This information could benefit health professionals, particularly physiotherapists, specializing in the pelvic floor, encouraging them to investigate, during anamnesis and physical examination, the potential consequence of COVID-19 on pelvic floor functions in terms of direct and indirect symptoms in the genito-urinary-area. We hypothesize that this evidence could inform physiotherapists’ clinical reasoning and decision-making process, guiding the adoption of appropriate treatments (e.g., manual therapy, therapeutic exercise, pelvic floor devices, and behavioral education) to properly address these issues.
Objectives
This scoping review aimed to investigate the prevalence of signs and symptoms of COVID-19 impacting directly or indirectly on pelvic floor function, to identify a population at risk of developing or worsening pelvic floor-related symptoms, and to inform clinicians of reasoning and decision-making.
Methods
Study design
The scoping review was conducted following the Joanna Bridge Institute methodology for scoping review (19) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA ScR) Checklist for reporting (20).
The protocol information relating to this review is stored in the OSF repository at the following link: Online.
Defining the research question
This scoping review aimed to identify and describe the extent of the scientific evidence available that investigates whether the signs and symptoms of COVID-19 may have directly or indirectly led to the onset or worsening of pelvic floor symptoms related to different areas: urological, ano-rectal-bowel, urogynecological, and sexual.
Specific objectives were:
– to identify the extent of research available in relation to study characteristics;
– to map and summarize findings related to signs and symptoms of pelvic floor in COVID-19 patients;
– to discover and describe any gaps in the literature.
Eligibility criteria
We used the Population, Concept, Context (PCC) framework according to Joanna Bridge Institute methodology for scoping reviews to identify useful studies for our research (19). Specifically, we included studies published in any language focusing on:
(i) Population: pediatric, adolescent, and adult subjects (including elderly) or mixed population (e.g., presence of adults and children) regardless of sex. Pediatric subjects were included because it’s important to identify as early as possible during life symptoms that may involve the intimate area of the person, thus also determining significant dysfunction in adulthood (21,22). Elderly subjects were involved in this study to analyze how their quality of life may have been changed in relation to the onset of the pelvic floor consequences caused by COVID-19 (23).
(ii) Concept: studies that describe signs and symptoms of the pelvic floor in the following categories: anorectal bowel (e.g., constipation), urogynecological (e.g., urinary incontinence, pelvic organ prolapse), sexual diseases (e.g., dyspareunia). In COVID-19 (including long-COVID);
(iii) Context: Any clinical context (patients who complain of urological, ano-rectal-bowel, gynecological, sexual, symptoms pelvic floor related) and/or organizational context during COVID-19;
(iv) Type of Evidence sources: systematic review, observational or experimental study published in English excluding other publication types such as letter, editorial, news, comment, case series, case report, and narrative review. Studies focusing on non-human populations and studies that referred to conditions related to the vaccine or with the title referring to the use of drugs or vaccine conditions were excluded. We have also decided to exclude all studies in which the manifestation of symptoms was linked to the contextual situation of the isolation induced by the pandemic as, for example, studies related to sexual activity limited by the forty: we have also decided to exclude all studies in which the manifestation of symptoms was linked to the contextual situation of the isolation induced by the pandemia.
Information sources
We used keywords and terminology referring to the international standards of the Scientific Societies and their reference Guidelines in this topic (6,24,25,26). We searched PubMed, Cumulated Index to Nursing and Allied Health Literature (CINAHL), and Embase by Mesh terms and free text words. Additional articles were handpicked from reference lists of included articles. We launched the search strategy on November 16, 2022. The full search strategy is reported in the Supplementary File.
Screening and study selection
After detecting the duplicates, two authors (VDT, MR) independently screened all publications by titles and abstract. A third author (AB) was consulted in case of disagreement. We used Rayyan software (27) to manage the study selection phase.
Charting the data
Two authors (VDT, MR) developed a data collection form to extract the characteristics of the included studies by piloting a small sample of ten records. The final data collection form was shared among review authors, reaching a consensus to collect and chart data. Finally, the two authors (VDT, MR) extracted data from the title and abstract of eligible studies and discussed any conflict.
We extracted the following data: name of the first author, year of publication, journal of publication, study design, aim (e.g., prevalence, intervention, prognosis), general characteristics of the population, including signs and symptoms directly or indirectly related to the pelvic-floor impacting on anorectal bowel, urogenital and sexual area. We defined direct signs or symptoms (as new onset or worsened) when they ranged from bladder or rectal emptying or filling symptoms, pelvic static alterations, chronic pelvic pain, and sexual dysfunction from pelvic floor dysfunction, as classified by International Scientific Societies of pelvic floor dysfunctions during COVID-19 (3,4). Indirect signs or symptoms are those symptoms developed during COVID-19 which can have consequences on the pelvic floor if continued over time, such as a persistent condition of bowel movement alteration, pelvic organ inflammation, pain and musculoskeletal dysfunction, sexual dysfunction, anxiety, depression, cough, dyspnea, neuropathies, and fatigue.
Summarizing and reporting results
The results were summarized in relation to the research questions with descriptive reporting. In addition, to identify the extent of research available in relation to study characteristics, we tabulated the main findings, whereas to map and summarize findings related to signs and symptoms of the pelvic floor in COVID-19 patients, we reported findings using figures. The symptomatology was categorized according to the anatomical area involved: urogenital area, sexual area, and anorectal bowel area.
Results
Selection of sources of evidence
After removing duplicates, we identified and screened 5323 references. A total of 577 references did not meet the inclusion criteria and have been excluded. Finally, 104 articles were included (Figure 1; references in Supplementary File).
Characteristics of sources of evidence
Among the 104 articles included, the main represented study designs were systematic reviews (N = 40; 38.46%) and retrospective studies (N = 39; 37.50%), followed by cross-sectional studies (N = 14; 13.46%) and prospective (N = 11; 10.58%) The majority (N = 80; 76.92%) were focused on the adult population, 13 (12.50%) on children and 11 on both (10.58%) (Table 1). Most studies had corresponding authors from the American region (N = 33; 31.73%), 29 from Northwestern Asia (27.88%), 20 from Europe (19.23%), and 22 from Southeast Asia (21.15%) (Figure 2). The graph was created with Excel to obtain data from the studies and create a table with the numbers of publications by countries of origin of the corresponding authors.
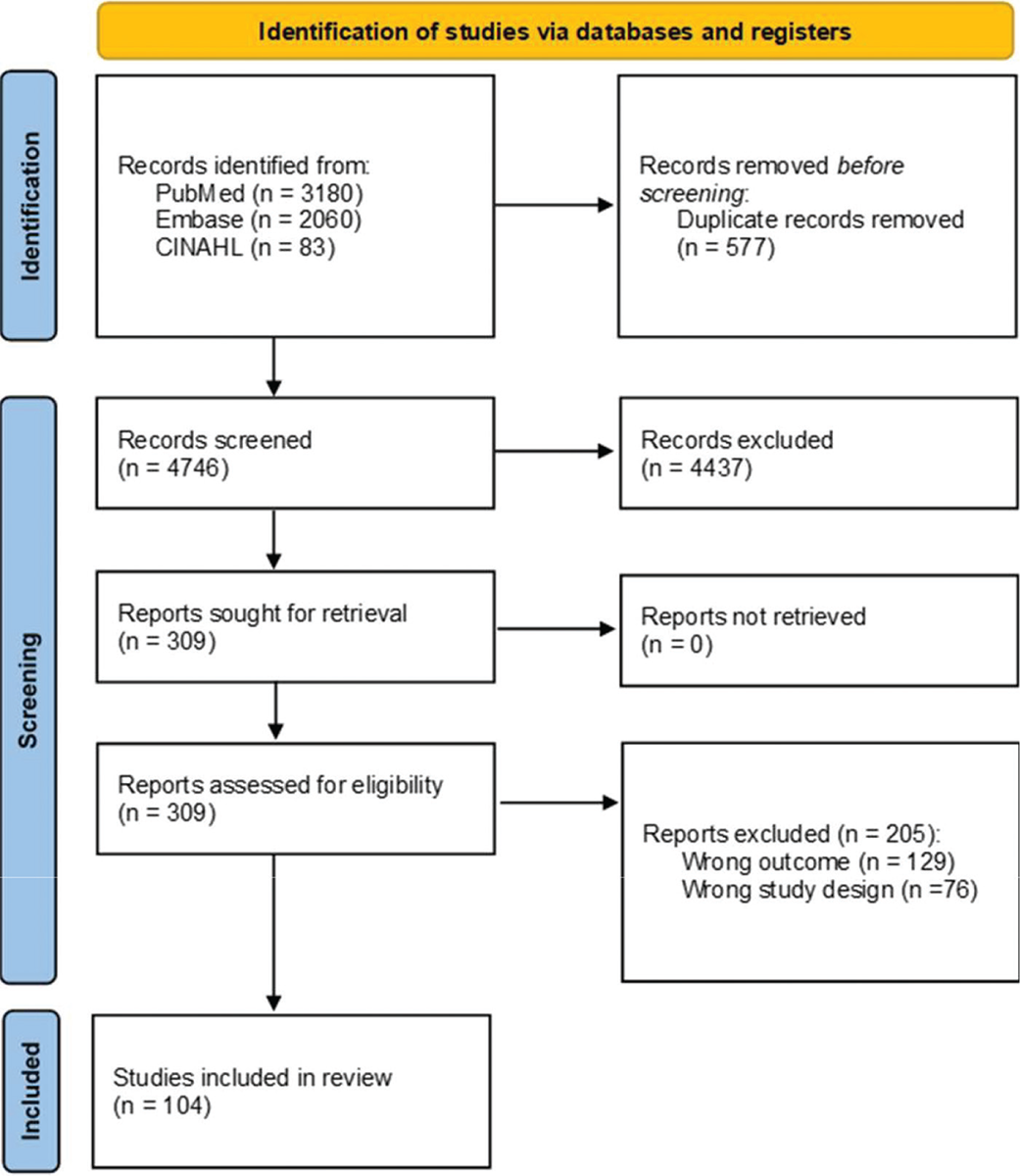
FIGURE 1 - Flow chart of study selection.
Identification of studies via databases and registers. After removing duplicates, 5323 references were identified and screened. A total of 3324 references did not meet the inclusion criteria and have been excluded. Finally, 104 articles were included.
| Characteristics | N (%) |
|---|---|
| Population | |
| Adults | 76 (73.08) |
| Adults women* | 1 (0.96) |
| Adults men* | 3 (2.88) |
| Children | 13 (12.50) |
| Mixed^ | 11 (10.58) |
| Study design | |
| Systematic review | 40 (38.46) |
| Randomized controlled trial | 0 (0.00) |
| Prospective | 11 (10.58) |
| Retrospective | 39 (37.50) |
| Cross-sectional | 14 (13.46) |
| Focus of study | |
| Prevalence | 57 (54.81) |
| Prognosis | 22 (21.15) |
| Intervention | 0 (0.00) |
| Prevalence and Prognosis | 25 (24.04) |
| Type of Covid-19 | |
| Acute | 85 (81.73) |
| Long covid | 11 (10.57) |
| Post covid | 4 (3.85) |
| Mixed$ | 4 (3.85) |
Legend: *studies specifically focusing on women or men; ^both adults and children; $acute, long or post-COVID-19; N, number; % percentage. Percentages in brackets are calculated out of the 104 overall included studies.
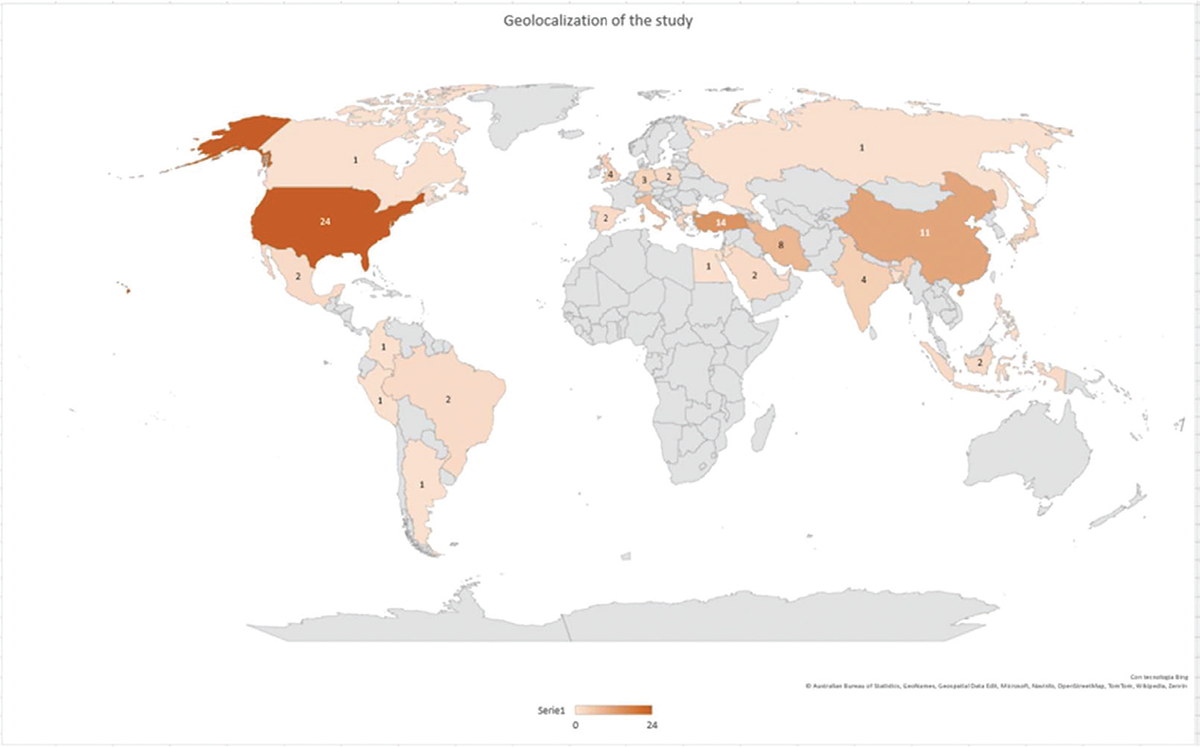
FIGURE 2 - Global prevalence of the studies analyzed.
The map represents the distribution of articles published in various countries. The intensity of the color progressively increases with the number of publications.
Symptoms classification
Overall, in 104 studies investigated, we analyzed 140 signs and symptoms. In particular, we found 16 (11.43%) signs and symptoms in 16 studies classified as direct and 124 (88.57%) signs and symptoms in 88 studies classified as indirect.
As reported in Table 2, the prevalent area was anorectal bowel (N = 115 signs and symptoms out of 140; 82,14%), followed by urogenital (N = 19 out of 140; 13,57%) and sexual area (N = 6 out of 140; 4,29%).
The prevalent symptoms in the urogenital area were LUTS (n = 16; 84.21%), while in the ano-rectal-bowel area was diarrhea (N = 81; 70.43%), and in the sexual area was erectile dysfunction (N = 4; 66.67%).
Figure 3 shows the signs and symptoms categorized based on whether their influence was direct or indirect on the symptomatic areas considered.
Among direct symptoms, the prevalent area was urogenital with LUTS, with the symptoms always presented (n = 16 out of 16; 100%). No studies reported direct symptoms for ano-rectal-bowel and sexual areas.
On the contrary, among the indirect symptoms, the prevalent reported signs and symptoms were anorectal bowel ones (n = 115; 92.74%), with diarrhea the most reported symptom (n = 81 out of 115; 71.7%)
| Signs and symptoms area
(n = 140) |
N | Area | Symptoms | N (%) |
| 115 | Ano-rectal-bowel | Diarrhea | 81 (70.43) | |
| Abdominal pain | 25 (21.74) | |||
| Constipation | 9 (7.83) | |||
| 19 | Uro-genital | LUTS | 16 (84.21) | |
| Symptoms related to endometriosis | 1 (5.26) | |||
| Uro-genital inflammation and injections | 2 (10.53) | |||
| 6 | Sexual | Erectile dysfunction | 4 (66.67) | |
| Sexual desire | 2 (33.33) |
Legend: LUTS, Lower Urinary Tract Symptoms; n, numbers; %, percentage. In brackets, we reported percentages of the overall number of symptoms in each category.
Discussion
This scoping review, including 104 articles, covers anorectal, sexual, and urogenital signs and symptoms linked to the pelvic floor in all age populations resulting from COVID-19 disease. As a main finding, we found a high prevalence of both direct and indirect symptoms affecting pelvic floor function in COVID-19 patients. Indirect symptoms were more common, particularly in the anorectal and bowel area, with diarrhea being the main symptom. In fact, diarrhea could be a significant risk factor for fecal incontinence, suggesting that its presence, combined with SARS-CoV-2 infection, might have severe consequences for the pelvic floor (28,29).
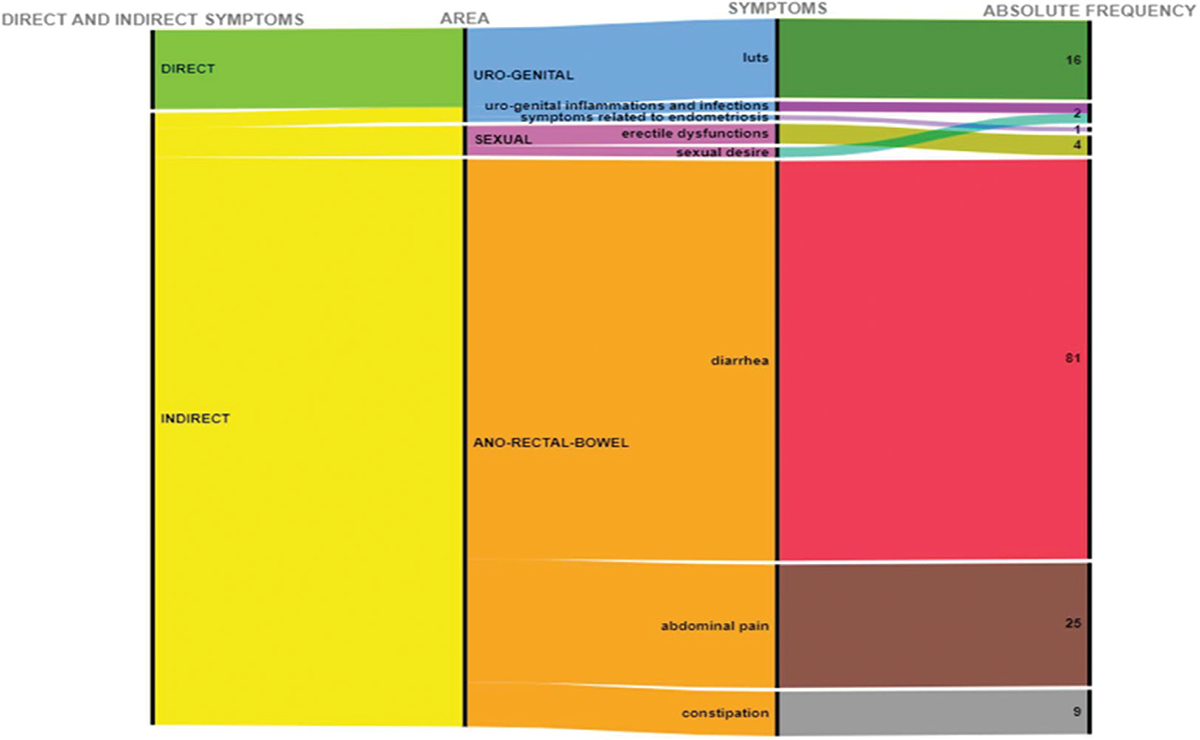
FIGURE 3 - Direct and indirect symptoms according to clinical area.
Direct and indirect symptomsrelated to the pelvic floor caused or worsened by COVID-19 displayed according to the clinical area: the prevalent area among direct symptoms was urogenital with LUTS (upper part of the light blue color), and among indirect symptoms was anorectal bowel with diarrhea (upper part of orange color).
Direct symptoms were primarily reported in the urogenital area, with LUTS being the most frequent issue. The severity of COVID-19 was found to correlate with an increase in LUTS. Sexual dysfunctions, though less common, were also reported, including erectile dysfunction and altered sexual desire, which can affect pelvic floor muscle function. In fact, male and female sexual dysfunction can cause and support symptoms involved in disability of pelvic floor muscles in their function (30,31).
Comparison with literature
To the best of our knowledge, this is the first scoping review investigating the reporting of direct and indirect signs and symptoms affecting urogenital, sexual, and anorectal bowel areas in COVID-19 patients, thereby limiting the comparison with existing evidence.
Another scoping review reported a relationship between gastrointestinal symptoms and COVID-19 infection in the pediatric population, with diarrhea being the most prevalent symptom (32). In fact, ACE1 and ACE2 are more expressed at the intestinal level in children than in adults, which explains why the pediatric population presents more evident gastrointestinal symptoms compared to adults (33).
Other scoping reviews focused on the effects of lockdowns, reporting a broad impact on sexual health (34) and, considering different biomedical fields, an increased risk of developing musculoskeletal (MSK) disorders due to working from and at non-ergonomic home environments, sedentariness, and the limited access to a healthcare facility (35).
Clinical Implications
The findings of this scoping review constitute a valuable resource to guide the clinical reasoning and decision-making of clinicians working with pelvic floor dysfunctions, emphasizing the need for comprehensive evaluation and management strategies in post-COVID care to enhance patient quality of life. Given the high prevalence of direct and indirect pelvic floor symptoms in COVID-19 patients, physiotherapists should also consider inquiring about COVID-19 history during anamnesis, and when detected by clinical examination (36), they should implement multimodal and multiprofessional treatment. Physiotherapists should educate the patient and, through the application of hands-on (e.g., manual therapy (37,38) and hands-off techniques (e.g., therapeutic exercises (39), address pelvic floor-related symptoms to improve the function of the pelvic-floor muscles. Additionally, physiotherapists should collaborate synergistically with other healthcare professionals, such as urologists, gastroenterologists, and internist physicians, to manage the systemic symptoms of COVID-19 with targeted treatments, implement preventive measures to mitigate virus-related damage and identify high-risk patients for chronification.
Research Implications
Our scoping review highlights the need for further research worldwide on the direct and indirect impacts of COVID-19 on the pelvic floor. Most studies have been conducted in the Americas and Asia. Adult populations (>18 years of age) have been predominantly studied. Retrospective studies were the most common, followed closely by systematic reviews, with fewer observational, prospective, and cross-sectional studies. Considering the limitations of the existing literature, future studies should explore under-researched areas such as pelvic floor symptoms in pediatric populations and mixed-age groups. Moreover, research should involve patients from other regions (e.g., Africa, Europe, and Oceania). Qualitative studies (e.g., focus groups and interviews) could also inform clinicians about the lived experiences of patients with pelvic floor impairments related to COVID-19. Finally, longitudinal studies are required to understand the long-term impact of COVID-19 on pelvic health.
Strengths and Limitations
This review is the first to map the literature on the prevalence of COVID-19 symptoms affecting pelvic floor functions. It establishes a basis for hypothesizing the virus’s impact beyond the respiratory system. However, some limitations must be acknowledged. Firstly, the relationship between exposure and disease development could not be established due to limited primary research. Secondly, confounding factors may have influenced symptom presentation. Thirdly, methodological quality and critical appraisal of included studies were not assessed, as the focus was on the breadth of evidence. Fourthly, symptom prevalence percentages were not extracted, aligning with the scoping review’s purpose of mapping existing literature rather than detailed inspection (12). Lastly, only English-language articles were included. Additionally, the reduction in outpatient services during the pandemic may have led to underreporting and undertreatment of pelvic floor dysfunction, suggesting that current prevalence estimates might be underestimated.
Conclusions
COVID-19 is known to have multiple systemic implications, and our study demonstrates a significant prevalence of direct and indirect symptoms affecting pelvic floor functions, which can compromise patients’ quality of life. Clinicians should be vigilant about the potential link between COVID-19 and pelvic floor symptoms to identy high-risk patients and develop effective treatment programs, enhancing clinical practice from initial assessment to comprehensive treatment.
Disclosures
Conflicts of Interest: The authors declare no conflicts of interest.
Funding: This research received no external funding.
Informed Consent Statement: Not applicable.
Author contributions: Conception and design: AB, SG, GR, SB, GC; Acquisition of data: VDT, MR; Analysis and interpretation of data: VDT, MR; Drafting the article: AB, SG, SB, GC, VDT, MR, GR; Review and editing the article: VDT, MR, SB; Final approval for the completed article: AB, SG, SB, GC, VDT, MR, GR; All authors have read and agreed to the published version of the manuscript.
Data Availability Statement: Data sharing is not applicable. No new data were created or analyzed in this study, or the data presented in this study are available as supplementary material to this article.
References
- 1. Khan M, Adil SF, Alkhathlan HZ, et al. COVID-19: a global challenge with old history, epidemiology and progress so far. Molecules. 2020;26(1):39. CrossRef PubMed
- 2. Leung TYM, Chan AYL, Chan EW, et al. Short- and potential long-term adverse health outcomes of COVID-19: a rapid review. Emerg Microbes Infect. 2020;9(1):2190-2199. CrossRef PubMed
- 3. Zheng L, Zhang L, Zheng Y, et al. Digestive system infection by SARS-CoV-2: entry mechanism, clinical symptoms and expression of major receptors (Review). Int J Mol Med. 2023;51(3):19. CrossRef PubMed
- 4. Siracusa C, Gray A. Pelvic floor considerations in COVID-19. J Womens Health Phys Therap. 2020;44(4):144-151. CrossRef PubMed
- 5. D’Ancona C, Haylen B, Oelke M, et al. Standardisation Steering Committee ICS and the ICS Working Group on terminology for male lower urinary tract & pelvic floor symptoms and dysfunction. The International Continence Society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38(2):433-477. CrossRef PubMed
- 6. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5-26. CrossRef PubMed
- 7. Silva Andrade B, Siqueira S, de Assis Soares WR, et al. Long-COVID and post-COVID health complications: an up-to-date review on clinical conditions and their possible molecular mechanisms. Viruses. 2021;13(4):700. CrossRef PubMed
- 8. Zachariou A, Sapouna V, Kaltsas A, et al. Evaluation of overactive bladder symptoms in patients recovering from post-acute COVID-19 syndrome. J Multidiscip Healthc. 2022;15:2447-2452. CrossRef PubMed
- 9. Dhawan A, Ganduboina R, Dutta P, et al. COVID-associated cystitis: the culprit behind the bladder woes post-COVID infection? A review. Int Urol Nephrol. 2023;55(10):2367-2372. CrossRef PubMed
- 10. Lam CM, Sanderson M, Vu DT, et al. Musculoskeletal and neuropathic pain in COVID-19. Diagnostics (Basel). 2024;14(3):332. CrossRef PubMed
- 11. Thomaz RP, Colla C, Darski C, et al. Influence of pelvic floor muscle fatigue on stress urinary incontinence: a systematic review. Int Urogynecol J. 2018;29(2):197-204. CrossRef PubMed
- 12. Fitz FF, Bortolini MAT, Pereira GMV, et al. PEOPLE: Lifestyle and comorbidities as risk factors for pelvic organ prolapse-a systematic review and meta-analysis PEOPLE: Pelvic Organ Prolapse Lifestyle comorbidities. Int Urogynecol J. 2023;34(9):2007-2032. CrossRef PubMed
- 13. Yelin D, Daitch V, Kalfon T, et al. Long COVID sexual dysfunction among both genders: evaluation of a cohort of COVID-19 recoverees. Infect Dis Now. 2023;53(7):104750. CrossRef PubMed
- 14. Kalata U, Jarkiewicz MM, Barcz EM. Depression and anxiety in patients with pelvic floor disorders. Ginekol Pol. 2023;94(9):748-751. CrossRef PubMed
- 15. Coyne KS, Wein AJ, Tubaro A, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009;103(s3)(suppl 3):4-11. CrossRef PubMed
- 16. Felde G, Ebbesen MH, Hunskaar S. Anxiety and depression associated with urinary incontinence. A 10-year follow-up study from the Norwegian HUNT study (EPINCONT). Neurourol Urodyn. 2017;36(2):322-328. CrossRef PubMed
- 17. Irwin DE, Mungapen L, Milsom I, et al. The economic impact of overactive bladder syndrome in six Western countries. BJU Int. 2009;103(2):202-209. CrossRef PubMed
- 18. Sacco E, Gandi C, Li Marzi V, et al. Italian Society of Urodynamics (SIUD). Extensive impact of COVID-19 pandemic on pelvic floor dysfunctions care: a nationwide interdisciplinary survey. Neurourol Urodyn. 2021;40(2):695-704. CrossRef PubMed
- 19. Peters MDJGC, McInerney P, Munn Z, et al. Chapter 11: Scoping Reviews. Aromataris E, Munn Z (Editors). JBI Man. Evid. Synth. JBI, 2020. CrossRef.
- 20. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and Explanation. Ann Intern Med. 2018;169(7):467-473. CrossRef PubMed
- 21. Bolia R, Goel AD, Badkur M, et al. Gastrointestinal Manifestations of pediatric coronavirus disease and their relationship with a severe clinical course: a systematic review and meta-analysis. J Trop Pediatr. 2021;67(2):fmab051. CrossRef PubMed
- 22. Tiryaki S, Egil O, Birbilen AZ, et al. COVID-19 associated lower urinary tract symptoms in children. J Pediatr Urol. 2022;18(5):680.e1-680.e7. CrossRef PubMed
- 23. Can O, Erkoç M, Ozer M, et al. The effect of COVID-19 on lower urinary tract symptoms in elderly men. Int J Clin Pract. 2021;75(6):e14110. CrossRef PubMed
- 24. Abrams P, Cardozo L, Fall M, et al. Standardisation Sub-Committee of the International Continence Society. The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Urology. 2003;61(1):37-49. CrossRef PubMed
- 25. Sultan AH, Monga A, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int Urogynecol J. 2017;28(1):5-31. CrossRef PubMed
- 26. Basson R, Leiblum S, Brotto L, et al. Revised definitions of women’s sexual dysfunction. J Sex Med. 2004;1(1):40-48. CrossRef PubMed
- 27. Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. CrossRef PubMed
- 28. Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009 Aug;137(2):512-517.e1-2. CrossRef
- 29. Bharucha AE, Knowles CH, Mack I, et al. Faecal incontinence in adults. Nat Rev Dis Primers. 2022;8(1):53. CrossRef PubMed
- 30. Seehuus M, Fertig M, Handy AB, et al. The impact of COVID-19 and long COVID on sexual function in cisgender women. J Sex Med. 2024;21(2):129-144. CrossRef PubMed
- 31. Salar R, Erbay G, Şanlı A, et al. Effect of COVID-19 infection on the erectile function. Andrology. 2023;11(1):10-16. CrossRef PubMed
- 32. Desconsi D, Araujo JP, Furtado MD, et al. Relationship between gastrointestinal symptoms and COVID-19 infection in the pediatric population: a scoping review. Rev Esc Enferm USP. 2024;58:e20230365. CrossRef PubMed
- 33. Canani RB, Comegna M, Paparo L, et al. Age-related differences in the expression of most relevant mediators of SARS-CoV-2 infection in human respiratory and gastrointestinal tract. Front Pediatr. 2021;9:697390. CrossRef PubMed
- 34. Toldam NE, Graugaard C, Meyer R, et al. Sexual health during COVID-19: a scoping review. Sex Med Rev. 2022;10(4):714-753. CrossRef
- 35. Gebrye T, Niyi-Odumosu F, Lawoe J, et al. The impact of COVID-19 related lockdown restrictions on musculoskeletal health: a systematic review. Rheumatol Int. 2023;43(11):2011-2019. CrossRef PubMed
- 36. Frawley H, Shelly B, Morin M, et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn. 2021;40(5):1217-1260. CrossRef PubMed
- 37. Farra FD, Aquino A, Tarantino AG, et al. Effectiveness of myofascial manual therapies in chronic pelvic pain syndrome: a systematic review and meta-analysis. Int Urogynecol J. 2022;33(11):2963-2976. CrossRef PubMed
- 38. Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS, et al. A systematic review and meta-analysis of the efficacy of manipulative therapy in women with primary dysmenorrhea. Explore (NY). 2017;13(6):386-392. CrossRef PubMed
- 39. Alouini S, Memic S, Couillandre A. Pelvic floor muscle training for urinary incontinence with or without biofeedback or electrostimulation in women: a systematic review. Int J Environ Res Public Health. 2022;19(5):2789. CrossRef PubMed