 |
Arch Physioter 2024; 14: 96-104 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3092 ORIGINAL RESEARCH ARTICLE |
 |
The Italian version of the Postural Assessment Scale for Stroke Patients (PASS): transcultural translation and validation
ABSTRACT
Introduction: The Postural Assessment Scale for Stroke Patients (PASS) is commonly used by health professionals in Italy in several different translations. This study aimed to provide a validated version in Italian. The main focus is on the evaluator, to guarantee a uniform application and interpretation of the statements and scoring for each item in the Italian context.
Methods: A standardized protocol was used for the translation and cross-cultural adaptation. A pilot study conducted using the first draft of the scale led to a revised version, PASS-IT. A principal component analysis (PCA) was performed. The correlation with the Trunk Control Test (TCT) was examined for concurrent validity. In addition, the relationship with the Barthel Index (BI) and the Functional Ambulation Categories (FAC) was tested. Patients with recent stroke were tested for intra-rater (N = 49) and inter-rater agreement (N = 30). Cronbach’s alpha, item-to-total correlation, corrected inter-item correlation, the intraclass correlation coefficient (ICC), and measurement error were used to evaluate internal consistency and intra-/inter-rater reliability.
Results: The PCA showed a two-dimensional structure, with high reliability in both subsections (“non-weight-bearing” α = 0.865; “weight-bearing” α = 0.949). A strong correlation (ρ > 0.80) was found with the TCT, the BI, and the FAC. The PASS-IT showed high internal consistency, intra-rater (ICC = 0.942) and inter-rater reliability (ICC = 0.940).
Conclusions: The PASS-IT is a recommended scale, suitable for clinical practice and research in the acute and subacute stage. The introduction of operating instructions resulted in the uniform application. A different order of the items allows faster administration, reducing changes of posture.
Keywords: Cross-cultural adaptation, Outcome assessment, Postural balance, Postural control, Reproducibility of results, Stroke.
Received: April 14, 2024
Accepted: November 11, 2024
Published online: December 3, 2024
This article includes supplementary material
Corresponding author:
Elena Lora
email: elena.lora@aosp.bo.it
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What’s already known about this topic?
- The PASS is among the most recommended scales for the assessment of postural control in patients with stroke. Although it is extensively used in Italy in several different translations, a validated version is not available.
What does the study add?
- This study aimed to provide an Italian version of the PASS, going through a cross-cultural validation process, adding operating instructions to promote a uniform application and interpretation of the scale among Italian health professionals.
Introduction
Stroke is currently one of the most common causes of disability and dependence among the older adult population in developed countries (1-3). In the European Union, there are over 9.5 million stroke survivors and a 27% increase is expected in the next three decades, due to population aging and improved survival rates (4).
In addition to compromising the limb mobility in the affected side, a stroke causes an alteration of postural control and balance (5, 6). The ability to maintain balance in the sitting position, standing, and in postural variations is essential for the recovery of independence, and the close correlation between postural control of the trunk in the acute phase and future functional ability is recognized (6-10).
Being able to predict the degree of recovery at an early stage after the stroke onset allows the medical and rehabilitation team to optimize time, tools, and resources in planning goals and treatment (7, 8, 11). Hence the need to identify valid and adequate assessment tools. The Trunk Control Test (TCT) (12, 13) is probably the most used and feasible in the acute stage. Of the four scales for trunk control compared in 2019 by Fil Balkan et al (14), the TCT was found to be the most time-efficient and with a better predictive value, but showed a floor effect. In clinical practice a ceiling effect is also frequently observed within the first weeks (15). Other scales proposed in the literature, for example, the Fugl-Meyer (16, 17), require a long time and demanding training for their use (18). Others, such as the Trunk Impairment Scale (TIS) (5), evaluate trunk control only in a sitting position.
The Postural Assessment Scale for Stroke Patients (PASS), conceived by Benaim et al and published in 1999 (19), evaluates the ability to maintain stable postures and balance during positional changes. It can be applied to all patients with stroke, even those with minimal postural control, in the first 3 months. The validation studies confirmed the structural validity of the PASS, excellent inter- and intra-operator reliability, high internal consistency (19), and the absence of floor/ceiling (F/C) effects when applied to the target population in the first weeks post-stroke (19, 20). A ceiling effect has been found for patients with high functional ability (21, 22).
Recent studies showed that, compared to the Berg Balance Scale, the PASS is better able to detect balance improvements in patients with severe balance deficits (23), and that it is a valid instrument to assess balance at an early stage (20) but also in the subacute and chronic phase (24, 25). It is an excellent early predictor for autonomy in both basic activities of daily living (ADLs) and instrumental ADLs (IADLs) (7, 19, 26), consistent with the results detected at 3 months with the Functional Independence Measure (FIM) (19) or at 6 months with the Barthel Index (BI) and the Frenchay Activities Index (19, 27). The predictive power is greater than the Fugl-Meyer’s (7), even in foreseeing the patient’s walking ability after discharge (28). Because of its properties and short evaluation time, the PASS is used worldwide and validated versions have been produced in Portuguese (29), Swedish (30), Spanish (31), Norwegian (32), and Turkish (33).
Moreover, the PASS is among the 14 highly recommended outcome measures selected in 2013 by the American Physical Therapy Association for individuals with stroke (34).
It is therefore advisable to use this tool in the clinical context. Although the PASS is commonly used in Italy, there is no cross-culturally validated version in this language. This study aimed to provide an Italian version of the PASS, going through a cross-cultural validation process, assessing its validity and intra-/inter-rater reliability.
Methods
The study was conducted in two phases (Fig. 1): (1) translation and cross-cultural adaptation of the first version of the Italian PASS (PASS-IT), followed by a pilot study to resolve possible critical issues; (2) a psychometric evaluation, assessing the validity and reliability of the PASS-IT.
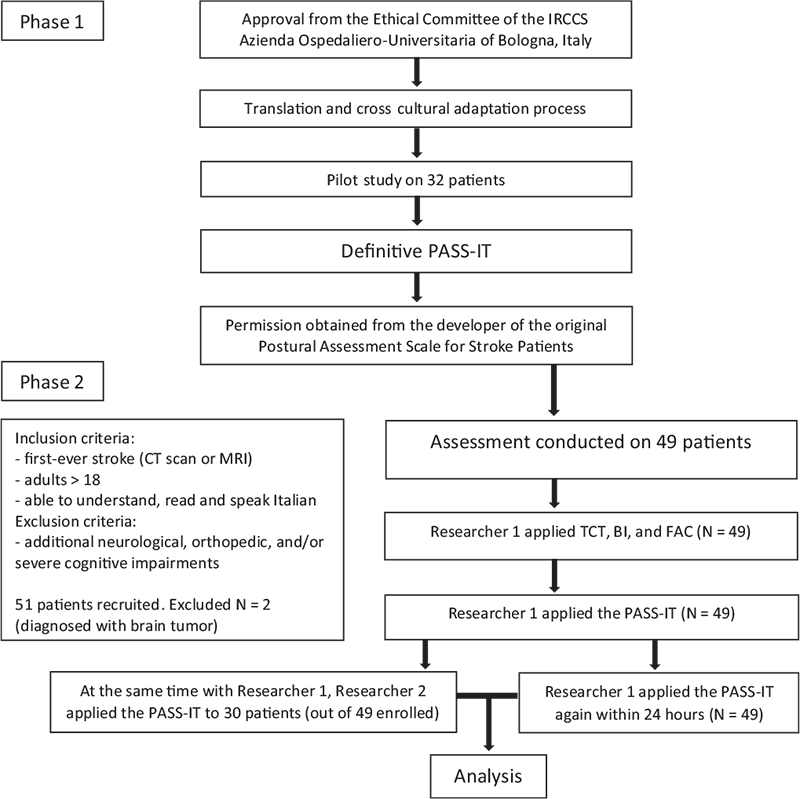
FIGURE 1 - Flowchart of the study.
Translation and cross-cultural adaptation
The translation and cross-cultural adaptation were conducted following the six-step method proposed by Beaton et al (35). Initially, two native Italian physiotherapists produced their own translations separately. Comparing the two translations, a synthesis was produced in agreement. Two back-translations were performed by native English translators, without clinical experience and not familiar with the original scale. The comparison between the original version and the back-translations revealed no substantial differences. Subsequently an expert committee (composed of a methodologist, all the translators involved in the previous phases, a physiotherapist not involved in the translation, a physiatrist, a geriatrician, a stroke unit doctor, a rehabilitation coordinator, and a nursing coordinator, all knowledgeable in English) analyzed the semantic, idiomatic, experiential, and conceptual areas of the scale, choosing the most suitable expression for each item. The changes made at this stage led to the first draft of the PASS-IT.
For a preliminary evaluation of the tool, this version was administered to a sample of 32 patients with recent stroke, admitted to the Stroke Unit and to the Unit of Physical Medicine and Rehabilitation of the IRCCS University Hospital of Bologna. The participants were informed about the study and gave written consent.
Twenty-one physiotherapists were invited to use the PASS-IT for 3 months. A questionnaire was then handed out, investigating clearness of the items, problems encountered, perception of confusing or missing features, and time needed to administer the scale. The results were reported in a focus group discussion, involving some of the authors, a methodologist doctor, and the physiotherapists, seeking terms which could guarantee the best univocal interpretation. Critical issues were highlighted and resolved by consensus.
Psychometric evaluation
Participants
The sample size of the psychometric evaluation study was determined combining the results of the pilot study (average total score 27.78 ± 8.19 in patients on day 14 ± 3 from stroke onset) and those reported by Koçak et al (average score 17.70 ± 10.08) (33). Since the current study involves patients in a more acute stage, an expected average score of 24 was estimated. Aiming for a statistical power of 80% (β = 0.20) and a significance level of 0.05 (α = 0.05), it was determined that 20 subjects would be necessary to ensure reliable and valid results. A larger sample size was enrolled, in order to offset potential dropouts, provide increased statistical power, and improve the generalizability of the results to a broader population, enhancing the external validity.
The study was conducted on a group of 49 consecutive patients (30 for the inter-rater reliability) admitted to the Stroke Unit of the IRCCS University Hospital of Bologna between February and July 2022. All patients were in the acute or early subacute phase after a stroke onset (mean: 5 ± 2.68 days; range: 1 to 12 days after the event).
The study included patients with a first-ever stroke, confirmed by a cerebral computed tomography (CT) scan or magnetic resonance imaging (MRI); adults ≥ 18; able to understand, read and speak the Italian language.
The study excluded patients with additional neurological, orthopedic, and/or severe cognitive impairments, which could compromise postural control or cooperation.
Data collection
Data were collected by two physiotherapists, both with experience with patients affected by neurological diseases. Researcher 1 was familiar with the PASS-IT, while Researcher 2, who had never used it before, received a short but detailed training session (≈1 hour).
For the intra-rater reliability investigation, the PASS-IT was tested twice by Researcher 1 within 24 hours. During the retest, Researcher 1 had no access to scores collected the first time. For the inter-rater reliability investigation, 30 patients were assessed at the same time by Researchers 1 and 2. No discussion or comparison was allowed between raters. All assessments were conducted bedside in the Stroke Unit, with the bed in a low position and without side rails, using a stopwatch and a PASS-IT form with operating instructions. To assess concurrent validity, Researcher 1 applied to the 49 patients the following test and scales:
– Postural Assessment Scale for Stroke Patients: specially designed for individuals with stroke, it evaluates both aspects of postural control: maintaining a posture and changing posture. It has good sensitivity, since it uses 12 items with increasing levels of difficulty in the three fundamental positions (lying, sitting, standing) and in postural variations, with four response options for each item (0 to 3; 3 = best performance), and a total score ranging from 0 to 36. It does not require specific training, nor equipment, except for a stopwatch. It can be safely administered by doctors and physiotherapists; the administration time varies from 1 to 10 minutes (19).
– Trunk Control Test: one of the best known and easiest to administer tools to assess trunk control in stroke (12, 13), it evaluates the patient in the lying and sitting position. It consists of four items with three response options (0 = unable to perform movement without assistance; 12 = able to perform movement, but in an abnormal style, e.g., pulls on bed clothes; 25 = able to complete movement normally), and a total score ranging from 0 (minimum) to 100 (maximum, indicating better performance) (12).
– Barthel Index: an ordinal scale developed in 1965 for use in rehabilitation patients with stroke and other neuromuscular or musculoskeletal disorders (36), it measures the degree of functional independence or need of assistance of an individual, evaluating 10 common activities of daily living (ADLs) with item scores ranging from 0 to 15, and a total score ranging from 0 (minimum) to 100 (maximum, indicating that no assistance is required to complete the activities). A validated Italian translation was used (37).
– Functional Ambulation Categories: developed in 1984, it is a 6-point scale that evaluates how much human support the patient requires when walking, considering different settings. The score ranges from 0 (patient cannot walk) to 5 (independent ambulation on any surface) (38).
Statistical analysis
Data were entered into a dedicated database, arranged by variables and finally analyzed using the Statistical Package for the Social Sciences (SPSS) 28.0 for Windows. Demographic data were analyzed using descriptive statistical tests.
The structural validity of the PASS-IT was evaluated with the explorative factor analysis.
The oblique (Varimax) rotation was used. The appropriateness of the factor analysis was evaluated using the Kaiser-Meyer-Olkin (KMO) test (39) and Bartlett’s test. Sampling was considered adequate if KMO was higher than 0.6. Additionally, the result of Bartlett’s test of sphericity must be less than 0.05 to indicate validity and suitability of the responses collected for the purpose of the study. The number of factors was determined using the scree plot, the overall variance, and the pattern matrix. Two-tailed p-values less than 0.05 were considered statistically significant.
The internal consistency of the PASS-IT was assessed using the Cronbach’s alpha coefficient (α); α ≥ 0.70 indicates high inter-item correlation and good homogeneity of the scale. Item-to-total correlation, corrected inter-item correlation, and Cronbach’s α when the item is deleted were evaluated. Item-to-total correlation represents the correlation between an individual item’s score and the total score of all other items in a scale, indicating how well a particular item aligns with the overall construct being measured. A common cutoff for an acceptable item-to-total correlation is 0.30 or higher, suggesting that the item contributes well to the overall reliability of the scale. Corrected inter-item correlation is the correlation between each item and the sum of the other items, excluding itself, which helps to avoid inflating the correlation value. It indicates how similar an item is to the rest of the items in a scale. Ideally, corrected inter-item correlations should be between 0.20 and 0.50, ensuring that items are related but not redundant. Values below 0.20 suggest the item might not fit well, while values above 0.50 might indicate redundancy. Cronbach’s α when the item is deleted represents the internal consistency reliability of a scale after the hypothetical removal of a specific item. Values that increase significantly upon deletion suggest that the item may be negatively contributing to the homogeneity of the scale, whereas minimal changes imply that the item is well-aligned with the overall construct being measured.
For construct validity, the PASS-IT was compared with the TCT. Since previous studies (20, 40) demonstrated the strong positive correlation between the PASS and the level of independence in ADLs and walking, a correlation analysis was also performed to explore the relationship with the BI and the FAC. The correlation was examined using the Spearman’s rho (ρ), whose value varies between −1 (perfect negative association) and 1 (perfect positive association), with 0 indicating no association. A correlation of 0.70 or higher, which is considered a strong association, was expected.
F/C effect, occurring when the score does not change from minimum or maximum despite clinical change, is defined as the proportion of participants scoring the lowest (floor) or highest (ceiling) possible score. It is considered to be present if 15% or more achieve the lowest or highest score. It indicates low reliability and limited responsiveness of the scale, since a change of performance in these participants cannot be measured (41).
The intra- and inter-rater reliability was assessed with the intraclass correlation coefficient (ICC) and 95% confidence interval (CI). ICC values of 0.70-0.89 indicate high agreement, 0.90-0.99 very high agreement, 1.00 perfect agreement.
To assess the significance of changes observed in our measurements, the Standard Error of Measurement (SEM) and the Minimal Detectable Change (MDC) were calculated. The SEM was computed to quantify the variability inherent in our measurement process, ensuring an understanding of the precision of our data. The SEM was calculated using the formula: SEM = SD*√ (1 – ICC), where SD represents the standard deviation of the baseline measurement.
The MDC was then derived to determine the smallest unit of change that can be detected by the instrument beyond measurement error. The MDC was calculated using the formula: MDC = SEM × Z1-α/2 x, where Z1-α/2 is the z-value corresponding to the desired confidence level (typically 1.96 for a 95% confidence level), and the factor adjusts for the two measurements being compared. This ensures that any observed change equal to or greater than the MDC is unlikely to be due to random measurement error, but rather reflects a true change in the underlying phenomenon being measured.
Since the PASS and the TCT have different ranges (PASS 0-36, TCT 0-100), direct comparison of the SEM and MDC values could lead to misleading interpretations. Larger ranges naturally produce higher absolute values for SEM and MDC, which might not reflect a true difference in the relative precision or variability of the scales. To allow for meaningful comparison, the normalized SEM and normalized MDC were calculated, dividing each value by the respective scale range and expressing the result as a percentage: normalized SEM = (SEM/Range) × 100; normalized MDC = (MDC/Range) × 100. This normalization process enables us to compare the relative error and detectability of changes across both scales, independent of their absolute range, allowing for a more accurate evaluation of the precision and reliability of the two tests.
Results
Translation and cross-cultural adaptation
The focus group with 21 physiotherapists highlighted difficulties related to the interpretation of ambiguous terms. For example, “support” can have several translations in Italian (Appoggio, Sostegno, Supporto, or Assistenza) with different meanings, confusing the active participation of the patient with the help provided by an external operator. We chose the terms that enjoyed the broadest understanding.
Critical issues were resolved by consensus. To overcome them, a final version was produced (Appendix 1, Supplementary Material), with operating instructions and a different order of the items (Fig. 2). The PASS-IT was submitted to the developers of the original PASS (19), receiving their approval.
Psychometric evaluation
Fifty-one patients had been initially recruited; two were excluded at a later time because they were also diagnosed with a brain tumor. The characteristics of the participants are presented in Table 1.
Further information about participants’ sensory disorders, unilateral spatial neglect (USN), upper/lower limb spasticity and function, as well as frequency distributions and percentage of the scores collected for each item are provided in the Supplementary Material (Table S1 and S2, respectively).
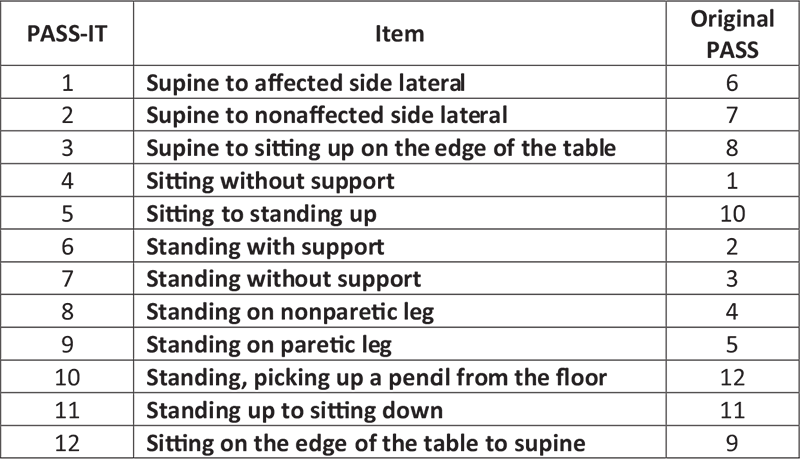
FIGURE 2 - New order of the items.
| Validity and intra-rater reliability study N = 49 | Inter-rater reliability study N = 30 | ||
|---|---|---|---|
| Age (in years) | Mean ± SD | 71.96 ± 12.46 | 68.57 ± 13.02 |
| Median (range) | 75 (41-89) | 69 (41-89) | |
| Gender | Women | 21 (42.86%) | 14 (46.67%) |
| Men | 28 (57.14%) | 16 (53.33%) | |
| Diagnosis | Ischemic | 40 (81.63%) | 24 (80%) |
| Hemorrhagic | 9 (18.37%) | 6 (20%) | |
| Brain injuries | Right | 24 (48.98%) | 14 (46.67%) |
| Left | 25 (51.02%) | 16 (53.33%) | |
| Days between date of ictus and date of testing | Mean ± SD | 5 ± 2.68 | 5 ± 2.59 |
| Median (range) | 4 (1-11) | 5 (1-12) |
SD = standard deviation.
N = 49 patients included in the validity and intra-rater reliability study;
N = 30 patients included in the inter-rater reliability study.
A principal component analysis was performed. The KMO test (0.880, p < 0.01) confirmed the appropriateness of the factor analysis and of the sample size. Bartlett’s test of sphericity was < 0.001. The scree plot (Figure S1 in Supplementary Material), the overall variance, and the pattern matrix showed a two-dimensional structure. The two components were studied with a Varimax rotation with Kaiser normalization (Table S3 in Supplementary Material). In factor analysis, items are allocated to factors according to the highest factor loadings, typically using a threshold of 0.3 or 0.4. Two unexpected groups of items were identified: items 1-4 plus 12 (activities performed in lying/sitting position, “non-weight-bearing”) and items 5-11 (activities standing, “weight-bearing”). High reliability was found for both subsections: “non-weight-bearing” (ICC = 0.865; 95% CI: 0.795-0.917) and “weight-bearing” (ICC = 0.949; 95% CI: 0.924-0.968). These two subsections, which were not further investigated in this study, do not coincide with those of the original PASS (“maintaining a posture” and “changing posture”).
Table 2 shows the scores for the four scales administered by Researcher 1 on the same test occasion: PASS-IT, TCT, BI, and FAC. Spearman’s rho (ρ) showed high concurrent validity between the PASS-IT and the TCT (ρ = 0.845, p < 0.001) and a strong correlation with the BI (ρ = 0.884, p < 0.001) and the FAC (ρ = 0.889, p < 0.001).
| Median (IQR) | Minimum | Maximum | Concurrent validity/correlation with the PASS-IT | |
|---|---|---|---|---|
| PASS-IT | 27 (18) | 3 | 36 | --- |
| TCT | 100 (38) | 0 | 100 | ρ = 0.845, p < 0.001 |
| BI | 45 (80) | 0 | 100 | ρ = 0.884, p < 0.001 |
| FAC | 1 (4) | 0 | 5 | ρ = 0.889, p < 0.001 |
BI = Barthel index; FAC = Functional Ambulation Categories; IQR = interquartile range; PASS-IT = Postural Assessment Scale for Stroke Patients, Italian; TCT = Trunk Control Test.
Table 3 shows the internal consistency results. For each item the median score with Interquartile Range (IQR) is shown, together with the item-to-total correlation, corrected inter-item correlation, and Cronbach’s α when the item is deleted. The item-to-total correlation shows a value of 0.390 for the first item, while the others range from 0.663 to 0.939. The corrected inter-item correlation shows a value of 0.363 for the first item, with the others ranging from 0.617 to 0.921. Cronbach’s α coefficient, regardless of which item is deleted, is always > 0.90 (range 0.929-0.947).
| Intra-rater | ||||
|---|---|---|---|---|
| Median (IQR) | Item-to-total correlation | Corrected inter-item correlation | Cronbach’s α when item is deleted | |
| 1. Supine to affected side lateral | 3 (0) | 0.390 | 0.363 | 0.947 |
| 2. Supine to the nonaffected side lateral | 3 (0) | 0.663 | 0.628 | 0.941 |
| 3. Supine to sitting up on the edge of the table | 3 (1) | 0.800 | 0.771 | 0.937 |
| 4. Sitting without support | 3 (0) | 0.734 | 0.686 | 0.938 |
| 5. Sitting to standing up | 3 (3) | 0.939 | 0.921 | 0.929 |
| 6. Standing with support | 3 (3) | 0.922 | 0.897 | 0.930 |
| 7. Standing without support | 3 (3) | 0.933 | 0.911 | 0.930 |
| 8. Standing on nonparetic leg | 0 (1) | 0.703 | 0.643 | 0.940 |
| 9. Standing on paretic leg | 0 (1) | 0.680 | 0.617 | 0.940 |
| 10. Standing, picking up a pencil from the floor | 2 (3) | 0.882 | 0.843 | 0.933 |
| 11. Standing up to sitting down | 3 (3) | 0.929 | 0.907 | 0.930 |
| 12. Sitting on the edge of the table to supine | 3 (1) | 0.804 | 0.779 | 0.938 |
IQR = interquartile range.
In the intra-rater reliability study, the mean total score for the PASS-IT is 24.15 ± 10.14 for the first assessment and 24.29 ± 10.16 for the second assessment made by Researcher 1. The mean interval between assessments was 9h43’ (SD = 6h54’; range 3h30’ to 21h30’). There is high reliability between total scores (ICC = 0.942; 95% CI: 0.914-0.963; p < 0.001) and for each item between first and second assessment, with ρ ranging from 0.817 to 0.991.
In the inter-rater reliability study, the mean total score for the PASS-IT is 26.00 ± 9.60 for Researcher 1 and 26.03 ± 9.60 for Researcher 2. The assessments are highly consistent for total scores (ICC = 0.940; 95% CI: 0.903-0.968; p < 0.001) and for single items, with ρ ranging from 0.988 to 1.000.
The SEM is 1.72 points for the intra-rater, and 1.63 points for the inter-rater reliability. The MDC95% is 4.76 based on intra-rater reliability data.
In the PASS-IT, five patients (10.20%) reached the maximum score (mean 24.22/36; range 3 to 36). Nine patients (18.37%) scored between 34 and 36/36. No one scored 0. In the TCT, 29 patients (59.18%) received the highest score (mean 77.63/100; range 0 to 100). The zero score was given to two patients (4.08%).
With the new sequence of items, the time of administration decreased (pilot study, mean 12′14″, range 5 to 20 minutes; psychometric study, mean: 7′55 ″, range 4′35 ″ to 15′25 ″).
Discussion
The PASS-IT, with concise operating instructions, showed a high intra- and inter-rater reliability, reflecting a uniform application and interpretation of the scale. The involvement of a large group of physiotherapists, together with the rigorous method followed for the cross-cultural translation, can be considered a strength of this study.
The modified sequence of the items, chosen also for the Swedish (Swe-PASS) (30) and Norwegian versions (Swe-PASS-NV) (32), allowed a quicker and smoother administration, avoiding repeated unnecessary changes of posture. The clear distinction between the original two sections of the scale (“Maintaining a posture” and “Changing posture”) is not featured, but the total score of the test does not change.
Although the PASS requires no training for use, the pilot study highlighted the need for operating instructions, consisting of concise and pragmatic indications, shown before each item in the evaluation form, aiming to increase the uniformity both in the administration (setting, instruction given to the patient) and in the interpretation of the results. For example, for items 4, 7, 8, 9 (sitting without support, standing without support, standing on the nonparetic/paretic leg) it is essential to use a stopwatch, as planned by the authors of the PASS (20). Underestimating its use in the pilot study led to imprecise scores.
In items 1-3, 5, 10-12, different scores are expected based on the amount of help received (“much help,” “little help,” “without help”) (19). There are no tools to quantify numerically the help provided, which is subjectively affected by age, technique, experience, build, and physical training of the operator. The Swe-PASS replaced “much help” with “support from two persons” and “little help” with “support from one person” (30). After extensively discussing this aspect, the original definition was preferred for the PASS-IT.
The original PASS describes a setting with a Bobath-type plane 50 cm in height, with the person’s feet resting on the floor. For short people, it is difficult to touch the ground from this height, except by moving dangerously forward on the edge of the couch. For taller people, excessive bending of the lower limbs leads to unfavorable leverage. A sitting position with hips and knees bent at 90° is therefore advisable, as recommended by the new instructions for items 4 and 5. When the patient rests on an anti-decubitus mattress, it is essential that the mattress be maximally inflated, to allow stability. Items in standing were tested wearing shoes, for greater safety and hygiene, even if the original PASS doesn’t specify whether the patient should be wearing shoes or be barefoot.
While other cross-cultural validation studies evaluated the patients at a chronic stage, or through a video-recorded performance (31, 32), our study was carried out in an acute setting, when a wide variety of factors (functional improvement, caution, fatigue, fear, disorientation) can produce sudden changes. For this reason, like in the Swedish validation study (30), we chose a short interval (< 24 hours) between the intra-rater observations, despite this representing a weakness of the study because of recall bias. A longer interval could result in higher grades at the second assessment, due to the functional recovery of the patient, or because posture changes had been practiced with the physiotherapist or the ward staff.
The value of verbal indications for carrying out the activity was also questioned. To standardize the application of the scale, it is important that no verbal indications be provided that are useful for its performance. Should they become necessary, the verbal indications would be considered as “little help,” like in the TCT (12).
The operating instructions emphasize that the PASS, for each of the 12 items, evaluates the ability to perform the activity, without considering its quality. They also draw attention to the fact that only one attempt is allowed for each item.
The PASS does not evaluate the ability to perform activities while seated. When this aspect is essential, it is advisable that more specific tools be used, such as the TIS (5), of which the validated translation in Italian is available (42), or the Function in Sitting Test (43).
No patient scored zero in item 1 (Supine to affected side lateral), and only one patient scored zero in item 2 (Supine to nonaffected side lateral). This can be partially explained by our exclusion criteria. Breistein et al (32) discussed the possibility that score 0 might be redundant for this item, since even patients with little to no functional independence can be turned on one side with help from one or two persons. We agreed that a zero be scored when medical conditions contraindicate rolling the patient to one side, but also when the patient shows no participation or involvement in the action.
In item 7, the highest score is given if the person “can stand without support for more than one minute and at the same time perform arm movement above the shoulder level.” It is important to select specific movements, with a predefined number of repetitions, to obtain comparable results. Persson et al (30) indicate the act of moving “hand/s from the forehead to the neck (like pulling your fingers through your hair)” and bringing the arm back, relaxed along the trunk, without however specifying the number of repetitions. We recommend at least five repetitions of this movement.
As shown in Table S2, at first assessment 59.2% of patients were not able to stand on the non-paretic leg (item 8), 63.3% were not able to stand on the paretic leg (item 9), and 46.9% were not able to pick up a pencil from the floor (item 10). These findings are in line with those of the Swe-PASS (30) and with the results described by Benaim et al (19) for the group of patients evaluated on day 30 after a stroke. In items 8 and 9 it is not clear whether the foot which is not bearing the weight must be lifted off the ground, or whether bending the hip and/or the knee is required. During the pilot study, these items had the worst inter-rater agreement. It was therefore specified that the foot must be lifted off the ground, with the opposite one entirely bearing the weight.
We consider the two-dimensional structure identified by the principal component analysis an unexpected and interesting finding. There is a clear division between items “non-weight-bearing” (1-4 plus 12), where the patients show much better performance, and the “weight-bearing” section (items 5-11), with a floor effect for some tasks. Nothing changes in the way the scale is administered and scored, but we believe that a “non-weight-bearing” and “weight-bearing” subdivision can be relevant to better comprehend the patient’s improvement and need for rehabilitation.
The present study confirmed a good correlation with the TCT (ρ = 0.845, p < 0.001) and the FAC (ρ = 0.889, p < 0.001), which had not been tested before. Our findings of a good correlation with the BI (ρ = 0.884, p < 0.001) are consistent with the values reported by Mao et al (20) and Chien et al (40).
The PASS-IT showed very high reliability, in line with Benaim et al (19) and other transcultural validations (30-33).
Considering that our patients were in the acute or early subacute phase after a stroke, and nine of them (18.37%) scored between 34 and 36/36, we agree with Chinsongkram et al (21) and with Wang et al (22) that a ceiling effect is plausible already in the first weeks for patients with high functional ability. The TCT showed a significant ceiling effect, with 29 patients (59.18%) earning the highest score. Considering this, the SEM (PASS = 1.72, normalized 4.77; TCT = 11.30), and the MDC (PASS = 4.76, normalized 13.22; TCT = 31.34), in our clinical practice the PASS-IT is more advisable, being more responsive to slight changes (e.g., going from “with much help” to “with little help”). Moreover, it evaluates the patients also in the standing position and single-leg stance.
The original PASS does not report an MDC value. Hsueh et al (44) indicate an MDC of 1.8 ± 1.7 for acute stroke, but their assessment was conducted at 14 and 30 days from onset. Breistein et al (32) calculated smallest detectable difference (SDD) = 1.9 points (intra-rater) and 2.7 points (inter-rater), but attested that “the measurement error may be considered to be artificially low” due to the use of video recorded assessment, without a real change in the participants’ performance.
Since different statistical methods were employed, a direct comparison of the results is often impossible.
Conclusion
The PASS-IT is a valid and reliable tool, suitable for clinical and physiotherapy practice in the acute and subacute stage. The final version of the cross-cultural translation, which includes short operating instructions and a different sequence for the 12 items, overcame critical issues encountered during the pilot study. It serves the purpose of promoting a uniform application and interpretation of the scale among Italian health professionals and researchers. Further study is needed to investigate the potential information provided by considering the scale in its two dimensions, “weight-bearing” and “non-weight-bearing.”
Acknowledgments
The authors wish to thank the patients who participated in this study and the physiotherapists of the Unit of Physical Medicine and Rehabilitation of the IRCCS Azienda Ospedaliero-Universitaria di Bologna for their help in thoroughly discussing every critical aspect, and for being such a committed and passionate work team.
A sincere appreciation goes to the reviewers who, with their competence and attention, provided valuable guidance.
Disclosures
Conflict of interest: The authors declare that there is no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval: The study was approved by the Ethical Committee of the IRCCS University Hospital of Bologna (Reference N. 216/2017/O/Sper).
Authors contribution: EL: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Resources, Supervision, Validation, Visualization, Writing – Original Draft, Writing – Review & Editing; NG: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Software, Supervision, Validation, Visualization, Writing – Original Draft, Writing – Review & Editing; AB: Conceptualization, Data Curation, Investigation, Project Administration, Supervision, Validation, Writing – Review & Editing; AB: Conceptualization, Investigation, Project Administration, Resources, Supervision, Validation; LG: Conceptualization, Data Curation, Formal Analysis, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – Original Draft, Writing – Review & Editing; MR: Conceptualization, Data Curation, Formal Analysis, Resources, Software, Validation, Visualization, Writing – Original Draft, Writing – Review & Editing; DG: Conceptualization, Data Curation, Formal Analysis, Methodology, Resources, Software, Supervision, Validation, Writing – Review & Editing.
Data Availability Statement: The data presented in this study and the printable Italian Version of the PASS are available on request from the corresponding author.
References
- 1. Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? J Stroke Cerebrovasc Dis. 2004;13(4):171-177. CrossRef PubMed
- 2. Hankey GJ. Stroke. Lancet. 2017;389(10069):641-654. CrossRef PubMed
- 3. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153-e639. CrossRef PubMed
- 4. Wafa HA, Wolfe CDA, Emmett E, Roth GA, Johnson CO, Wang Y. Burden of stroke in Europe: thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke. 2020;51(8):2418-2427. CrossRef PubMed
- 5. Verheyden G, Nieuwboer A, Mertin J, Preger R, Kiekens C, De Weerdt W. The Trunk Impairment Scale: a new tool to measure motor impairment of the trunk after stroke. Clin Rehabil. 2004;18(3):326-334. CrossRef PubMed
- 6. Jijimol G, Fayaz RK, Vijesh PV. Correlation of trunk impairment with balance in patients with chronic stroke. NeuroRehabilitation. 2013;32(2):323-325. CrossRef PubMed
- 7. Hsieh CL, Sheu CF, Hsueh IP, Wang CH. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002;33(11):2626-2630. CrossRef PubMed
- 8. Kim TJ, Seo KM, Kim DK, Kang SH. The relationship between initial trunk performances and functional prognosis in patients with stroke. Ann Rehabil Med. 2015;39(1):66-73. CrossRef PubMed
- 9. Kong KH, Ratha Krishnan R. Truncal impairment after stroke: clinical correlates, outcome and impact on ambulatory and functional outcomes after rehabilitation. Singapore Med J. 2021;62(2):87-91. CrossRef PubMed
- 10. Martins LG, Molle da Costa RD, Alvarez Sartor LC, et al. Clinical factors associated with trunk control after stroke: A prospective study. Top Stroke Rehabil. 2021;28(3):181-189. CrossRef PubMed
- 11. Lesser M, Borst J, Dekerlegand J. Use of the Postural Assessment Scale for Stroke Patients in determining acute care discharge recommendations. J Acute Care Phys Ther. 2017;8(3):79-85. CrossRef
- 12. Collin C, Wade D. Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990;53(7):576-579. CrossRef PubMed
- 13. Franchignoni FP, Tesio L, Ricupero C, Martino MT. Trunk control test as an early predictor of stroke rehabilitation outcome. Stroke. 1997;28(7):1382-1385. CrossRef PubMed
- 14. Fil Balkan A, Salcı Y, Keklicek H, Çetin B, Adın RM, Armutlu K. The trunk control: which scale is the best in very acute stroke patients? Top Stroke Rehabil. 2019;26(5):359-365. CrossRef PubMed
- 15. Verheyden G, Vereeck L, Truijen S, et al. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clin Rehabil. 2006;20(5):451-458. CrossRef PubMed
- 16. Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13-31. CrossRef PubMed
- 17. Cecchi F, Carrabba C, Bertolucci F, et al. Transcultural translation and validation of Fugl-Meyer assessment to Italian. Disabil Rehabil. 2021;43(25):3717-3722. CrossRef PubMed
- 18. Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther. 1993;73(7):447-454. CrossRef PubMed
- 19. Benaim C, Pérennou DA, Villy J, Rousseaux M, Pelissier JY. Validation of a standardized assessment of postural control in stroke patients: the Postural Assessment Scale for Stroke Patients (PASS). Stroke. 1999;30(9):1862-1868. CrossRef PubMed
- 20. Mao HF, Hsueh IP, Tang PF, Sheu CF, Hsieh CL. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke. 2002;33(4):1022-1027. CrossRef PubMed
- 21. Chinsongkram B, Chaikeeree N, Saengsirisuwan V, Viriyatharakij N, Horak FB, Boonsinsukh R. Reliability and validity of the Balance Evaluation Systems Test (BESTest) in people with subacute stroke. Phys Ther. 2014;94(11):1632-1643. CrossRef PubMed
- 22. Wang CH, Hsueh IP, Sheu CF, Hsieh CL. Discriminative, predictive, and evaluative properties of a trunk control measure in patients with stroke. Phys Ther. 2005;85(9):887-894. CrossRef PubMed
- 23. Huang YJ, Lin GH, Lee SC, Hsieh CL. A comparison of the responsiveness of the Postural Assessment Scale for Stroke and the Berg Balance Scale in patients with severe balance deficits after stroke. J Geriatr Phys Ther. 2020;43(4):194-198. CrossRef PubMed
- 24. Estrada-Barranco C, Cano-de-la-Cuerda R, Abuín-Porras V, Molina-Rueda F. Postural Assessment Scale for Stroke Patients in acute, subacute and chronic stage: a construct validity study. Diagnostics (Basel). 2021;11(2):365. CrossRef PubMed
- 25. Liaw LJ, Hsieh CL, Lo SK, Chen HM, Lee S, Lin JH. The relative and absolute reliability of two balance performance measures in chronic stroke patients. Disabil Rehabil. 2008;30(9):656-661. CrossRef PubMed
- 26. Di Monaco M, Trucco M, Di Monaco R, Tappero R, Cavanna A. The relationship between initial trunk control or postural balance and inpatient rehabilitation outcome after stroke: a prospective comparative study. Clin Rehabil. 2010;24(6):543-554. CrossRef PubMed
- 27. Schuling J, de Haan R, Limburg M, Groenier KH. The Frenchay Activities Index. Assessment of functional status in stroke patients. Stroke. 1993;24(8):1173-1177. CrossRef PubMed
- 28. Huang YC, Wang WT, Liou TH, Liao CD, Lin LF, Huang SW. Postural Assessment Scale for Stroke Patients Scores as a predictor of stroke patient ambulation at discharge from the rehabilitation ward. J Rehabil Med. 2016;48(3):259-264. CrossRef PubMed
- 29. Yoneyama SM, Roiz R de M, Oliveira TM, Oberg TD, Lima NMFV. Validação da versão brasileira da Escala de Avaliação Postural para pacientes após acidente vascular encefálico. Acta Fisiatr. 2008;15(2):96-100. CrossRef
- 30. Persson CU, Hansson P-O, Danielsson A, Sunnerhagen KS. A validation study using a modified version of Postural Assessment Scale for Stroke Patients: Postural Stroke Study in Gothenburg (POSTGOT). J Neuroeng Rehabil. 2011;8(1):57. CrossRef PubMed
- 31. Cabanas-Valdés R, Girabent-Farrés M, Cánovas-Vergé D, Caballero-Gómez FM, Germán-Romero A, Bagur-Calafat C. [Spanish translation and validation of the Postural Assessment Scale for Stroke Patients (PASS) to assess balance and postural control in adult post-stroke patients]. Rev Neurol. 2015;60(4):151-158. PubMed
- 32. Breistein K, Gjelsvik BEB, Jørgensen L. The Postural Assessment Scale for Stroke Patients: translation into Norwegian, cultural adaptation, and examination of reliability. Eur J Physiother. 2017;19(4):207-214. CrossRef
- 33. Koçak FA, Kurt EE, Koçak Y, Erdem HR, Tuncay F, Benaim C. Validity and interrater/intrarater reliability of the Turkish version of the postural assessment scale for stroke patients (PASS-Turk). Top Stroke Rehabil. 2019;26(5):373-381. CrossRef PubMed
- 34. Sullivan JE, Crowner BE, Kluding PM, et al. Outcome measures for individuals with stroke: process and recommendations from the American Physical Therapy Association neurology section task force. Phys Ther. 2013;93(10):1383-1396. CrossRef PubMed
- 35. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186-3191. CrossRef PubMed
- 36. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61-65. PubMed
- 37. Castiglia SF, Galeoto G, Lauta A, et al. The culturally adapted Italian version of the Barthel Index (IcaBI): assessment of structural validity, inter-rater reliability and responsiveness to clinically relevant improvements in patients admitted to inpatient rehabilitation centers. Funct Neurol. 2017;22(4):221-228. CrossRef PubMed
- 38. Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys Ther. 1984;64(1):35-40. CrossRef PubMed
- 39. Yaşar M. Attitudes toward statistics scale: validity and reliability study. Pamukkale University Journal of Education. 2014;02:59-75. Online
- 40. Chien CW, Lin JH, Wang CH, Hsueh IP, Sheu CF, Hsieh CL. Developing a Short Form of the Postural Assessment Scale for people with stroke. Neurorehabil Neural Repair. 2007;21(1):81-90. CrossRef PubMed
- 41. Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34-42. CrossRef PubMed
- 42. Lombardi B, Orioli A, Casavola D, Paci M. The Italian version of the Trunk Impairment Scale: development and psychometric properties. Eur J Phys Rehabil Med. 2017;53(4):516-520. CrossRef PubMed
- 43. Gorman SL, Radtka S, Melnick ME, Abrams GM, Byl NN. Development and validation of the Function In Sitting Test in adults with acute stroke. J Neurol Phys Ther. 2010;34(3):150-160. CrossRef PubMed
- 44. Hsueh I-P, Chen K-L, Chou Y-T, Wang Y-H, Hsieh C-L. Individual-level responsiveness of the original and short-form postural assessment scale for stroke patients. Phys Ther. 2013;93(10):1377-1382. CrossRef PubMed