 |
Arch Physioter 2024; 14: 29-46 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3063 REVIEW |
 |
Hip microinstability and its association with femoroacetabular impingement: A scoping review
ABSTRACT
Introduction: Hip microinstability has become a recognized cause of non-arthritic hip pain and disability in young patients. However, its pathophysiology remains unclear. We want to (1) present an overview of the evidence of hip microinstability and of its association with femoroacetabular impingement (FAI), (2) map out the type of evidence available, and (3) make recommendations for future research.
Methods: A deductive analysis and extraction method was used to extract information. In addition, diagnostic accuracy statistics were extracted or calculated.
Results: Of the 2,808 identified records, 123 were eligible for inclusion. Different definitions for microinstability exist. A standardized terminology and clear diagnostic criteria are lacking. FAI and microinstability may be associated and may aggravate each other. Conservative treatment strategies for FAI and microinstability are similar. The reported prevalence of microinstability in combination with FAI ranges from 21% to 42% in adults undergoing hip arthroscopy or magnetic resonance arthrography (MRA) of the hip.
Conclusion: Hip microinstability and FAI may be associated, occur together, or exacerbate each other. To better address this topic, a standardized terminology for microinstability is essential. Achieving consensus on physical examination and diagnosis is also necessary. Initial efforts to establish uniform diagnostic criteria have been made, but further work is needed. Specifically, randomized controlled trials are required to evaluate the effectiveness of training programmes aimed at reducing symptoms in individuals with microinstability, with or without FAI. Such studies will enable clinicians to manage microinstability with greater confidence within this context.
Keywords: Femoroacetabular impingement (FAI), Hip impingement, Hip microinstability, Scoping review
Received: March 13, 2024
Accepted: July 8, 2024
Published online: August 1, 2024
This article includes supplementary material
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What is already known about this topic:
- Hip microinstability became increasingly recognized as a cause of non-arthritic hip pain and disability in young and active people, just as it is the case with femoroacetabular impingement (FAI). There is no consensus on the diagnostic criteria for hip microinstability. Treatments very similar to those for FAI are proposed. However, studies on the efficacy of conservative treatment for hip microinstability are lacking.
What does the study add:
- This study clarifies the concept of hip microinstability and elucidates the relationship between microinstability and FAI. An overview of the evidence on the definition, diagnosis, aetiology, prevalence, and treatments of hip microinstability, and of its broader association with FAI are presented.
Introduction
Hip microinstability is a relatively new diagnosis and not yet well established (1). Recently, this condition has received increasing interest as a medical picture responsible for non-arthritic hip pain and disability, particularly in young and active people (2,3). Another condition found in young and active people is FAI syndrome (4).
At the International Hip-related Pain Research Network meeting in Zürich, Switzerland, in 2018 (4), three categories for hip-related pain were proposed: (1) FAI syndrome, (2) acetabular dysplasia and/or hip instability, and (3) other conditions causing hip-related pain (including labrum, cartilage, and ligamentum teres lesions without a specific bony morphology). However, there is no consensus on the diagnostic criteria for hip microinstability (4,5).
The hip was believed to be a stable joint through his bony architecture (6). As the understanding of hip mechanics improved, it appeared that some hips are not as stable as thought (7). Hip stability is ensured by the bony, as well as the soft-tissue and muscle structures (1). Thus, bone abnormalities constitute anatomic risk factors for microinstability (8). On imaging, many patients with hip microinstability showed signs of dysplasia, but also of FAI morphologies (3,9). Thus, FAI and microinstability may not be mutually exclusive and may coexist.
The management of hip microinstability lacks clear establishment (6). Researchers propose surgical and conservative therapy strategies, which include strengthening exercises for the hip and core muscles, as well as activity modification (6,8). Thus, these treatments closely resemble those for FAI. However, researchers lack high-level studies on the efficacy of conservative treatment for hip microinstability (6). The effect of conservative care for FAI has been investigated in four randomized controlled trials (RCTs) (10-13). The surgical treatments aim to correct the underlying deformity in each case. However, they may differ substantially between the two diagnoses.
To the best of our knowledge, no systematic or scoping reviews highlighting microinstability in the context of hip impingement have been published to date.
There is a clear need to investigate the relation between microinstability and FAI, especially in the context of diagnosis and understanding of nonsurgical treatments of these two conditions.
This scoping review aims to: (1) present an overview of the evidence on the definition, diagnosis, aetiology, prevalence, and potential treatments of hip microinstability, and of its broader association with FAI, (2) map out the type of evidence available, and (3) make specific recommendations for future research.
Methods
Protocol and registration
The protocol for this scoping review was published on osf.io (DOI: CrossRef). The review was conducted according to recommendations of the JBI (formerly known as Joanna Briggs Institute) group (14,15). The authors wrote the manuscript according to the extension of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) checklist (16).
Eligibility criteria
All types of study design were included in the review. No language or publication date restrictions were applied. Articles about hip microinstability and people with or suspected of having pincer or cam morphology were included. Studies about instability after total hip arthroplasty, hip dislocation, traumatic instability, developmental dysplasia; studies including infants/toddlers; studies comparing different surgical techniques; as well as cadaveric and animal studies were excluded.
Search
Electronic searches were performed in MEDLINE (Ovid), CINAHL, and EMBASE from inception up to 12 July 2023. Reference lists of included articles were also screened for additional articles.
The full search strategy for each database is presented in the Supplementary Appendix A1.
Selection of sources of evidence
Reviewer 1 and reviewer 2 screened half of the abstracts and full texts, reviewer 1 and reviewer 3 screened the other half of the abstracts and full texts. A fourth reviewer was contacted in case of disagreement to determine a final decision. The flow diagram of study selection is shown in Figure 1.
Data charting process and data items
A data charting form (Supplementary Appendix A2) was developed and used to extract general source information (type of evidence, author, publication year) as well as key messages from each study on the following topics: definition, diagnosis, aetiology, prevalence, and treatment. Data extraction was not linear, but an iterative process. A deductive analysis and extraction method was used to extract contextual information from each study, extracted as text and grouped into separate sheets in Excel. Quantitative data (description of sample, group differences, etc.) was extracted in a further Excel form. For the diagnostic tests, true-positive, false-positive, false-negative, and true-negative frequencies were extracted or calculated.
Synthesis of results
A cross-table presenting the design of the studies and the topics covered was created, with an overlayed heat map (Fig. 2). A thematic construction was used to provide an overview of key concepts regarding definition, aetiology, diagnosis, treatment, and prevalence. Key messages were analysed chronologically. For the diagnostic tests, sensitivity, specificity, as well as positive and negative diagnostic likelihood ratios were extracted or calculated and presented with forest plots (Fig. 3 and Supplementary Tab. A2).
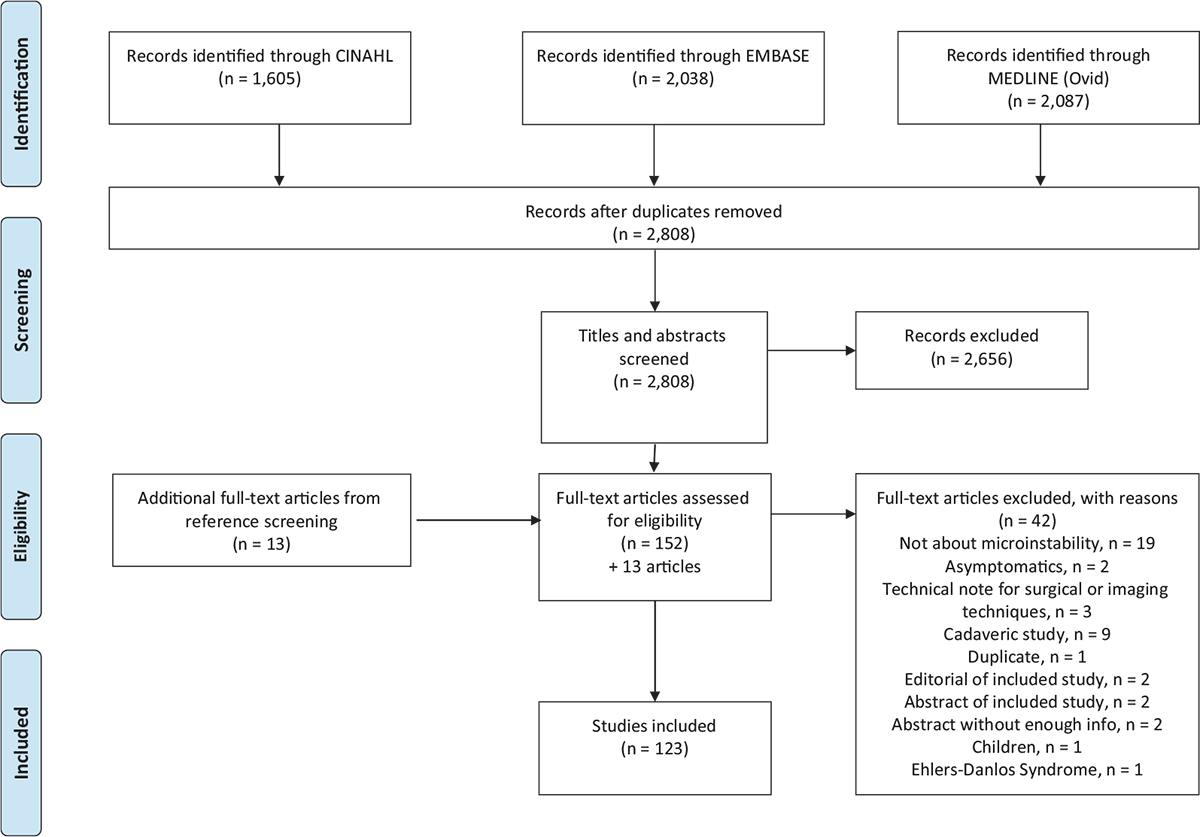
FIGURE 1 - Flow diagram.
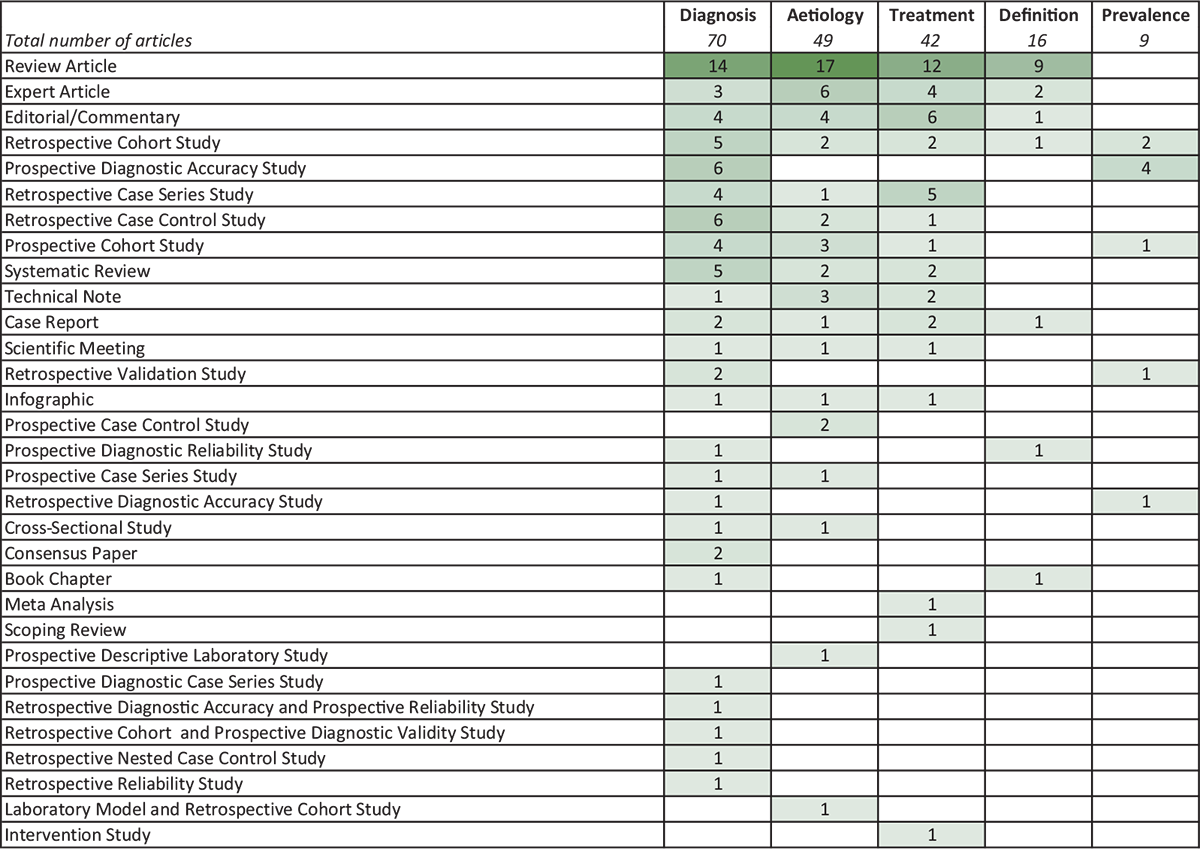
FIGURE 2 - Heat map of topic by study type.
Results
Selection of sources of evidence
The electronic search yielded a total of 2,808 records, after removal of duplicates. After additional reference screening, 123 articles met the inclusion criteria (Fig. 1). General study description, together with information about which topic is addressed in each study are listed in Supplementary Tab. A1.
Characteristics of sources of evidence
A heat map (Fig. 2) gives an overview of the different study types by topic. There were 31 types of evidence.
Synthesis of results
Definition
The most frequently cited definition of hip microinstability is the one by Shu and Safran (17): “Hip instability can be defined as extra-physiologic hip motion that causes pain with or without the symptom of hip joint unsteadiness. The cause can be traumatic or atraumatic and is related to both bony and soft-tissue abnormality. Gross instability is caused by trauma or iatrogenic injury. Subtle microinstability, from microtraumatic or atraumatic causes, is an evolving concept.” Notably, the authors did not make any distinction between hip instability and microinstability definition, except for the causes leading to instability.
Another frequently quoted definition is the one by Cerezal et al (18): “Hip microinstability is the inability to keep the femoral head centred within the acetabular fossa, without complete luxation or marked subluxation of the joint. Microinstability is laxity with the presence of symptoms. Asymptomatic hip joint laxity is not microinstability.”
Table 1 summarizes all studies presenting a definition of microinstability, with the respective sources.
| First author Year | Title | Definition of microinstability | Citation of definition |
|---|---|---|---|
| Shu 2011 (17) | Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability | “Hip instability is uncommon because of the substantial conformity of the osseous femoral head and acetabulum. It can be defined as extra-physiologic hip motion that causes pain with or without the symptom of hip joint unsteadiness. The cause can be traumatic or atraumatic, and is related to both bony and soft tissue abnormality. Gross instability caused by trauma or iatrogenic injury has been shown to improve with surgical correction of the underlying deficiency. Subtle microinstability, particularly from microtraumatic or atraumatic causes, is an evolving concept with early surgical treatment results that are promising.” | |
| Cerezal 2012 (18) | Emerging topics on the hip: ligamentum teres and hip microinstability | “Hip microinstability is the inability to keep the femoral head centered within the acetabular fossa, without complete luxation or marked subluxation of the joint. Hip laxity is not equivalent to microinstability. The difference is the presence of symptoms associated with laxity when we classified as microinstability. Only when symptoms are present in the context of laxity can it be classified as microinstability. An asymptomatic patient that is able to subluxate a joint has laxity, but not microinstability. Patients with microinstability often have laxity in both hips; only the symptomatic is classified as having microinstability.” | |
| Kalisvaart 2015 (8) | Microinstability of the hip – it does exist: etiology, diagnosis and treatment |
“Hip instability is generally defined as extraphysiologic hip motion that causes pain with or without symptoms of hip joint unsteadiness” “Symptomatic hip microinstability, however, has not received as much attention [as dislocation and traumatic subluxation], as it is more poorly defined, has a less dramatic clinical presentation, lacks consistent objective evaluative criteria, and it has only recently emerged as a significant cause of pain and disability in younger patients and athletes.” |
Shu 2011 (17) |
| Suter 2015 (19) | MR findings associated with positive distraction of the hip joint achieved by axial traction | “Atraumatic instability of the hip, also known as microinstability, is defined by two elements. The first element is laxity of the hip joint with the inability to keep the femoral head centered within the acetabular fossa, typically without complete luxation or marked subluxation of the joint. The second element is the presence of symptoms, such as pain or unsteadiness.” | Cerezal 2012 (18), Shu 2011 (17) |
| Bolia 2016 (20) | Microinstability of the hip: a previously unrecognized pathology | “Unlike other joints in the anatomy, hip instability is generally defined as extra-physiologic hip motion that causes pain with or without symptoms of hip joint instability. This entity is not well defined, as no objective criteria has been proposed to characterise hip microinstability.” | Shu 2011 (17), Kalisvaart 2015 (8) |
| Dangin 2016 (1) | Microinstability of the hip: a review | “It is generally defined as a painful supra-physiological mobility of the hip, associating architectural and functional abnormalities that impair hip stability. Microinstability is distinguished from hyperlaxity by its painful nature, and from traumatic (macro-) instability by its progressive onset and chronicisation following repeated microtrauma concerning at-risk patients. The typical patient is a young female adult with sports activity requiring suppleness and extensive ranges of motion, such as dancing or gymnastics. Microinstability is difficult to identify and thus probably underestimated.” “Microinstability is represented by excessive femoral head movement within the acetabulum.” |
Jackson 2016 (21), Domb 2013 (22), Kalisvaart 2015 (8), Cerezal 2012 (18) |
| Harris 2016 (23) | Microinstability of the hip and the splits radiograph | “The spectrum of hip instability ranges from subtle microinstability to traumatic dislocation. Microinstability may be either a cause or an effect of several other hip pathologies.” “Dance, gymnastics, figure skating, yoga, and cheerleading are among the sports and activities that may predispose to microinstability (symptomatic) over simple hyperlaxity or hypermobility (asymptomatic).” |
|
| d’Hemecourt 2019 (24) | Can dynamic ultrasonography of the hip reliably assess anterior femoral head translation? | “Hip microinstability is defined as painful supraphysiological mobility of the hip with associated architectural and functional abnormalities that impair joint stability.” | Bolia 2016 (20), Dangin 2016 (1), Kalisvaart 2015 (8), Jackson 2016 (21) |
| Harris 2019 (25) | Hypermobile hip syndrome | “Hypermobile hip syndrome may be defined as a triad of symptoms (patient’s unwanted or undesired subjective complaints), signs (physical examination abnormalities with excessive motion that provoke the inciting symptoms), and imaging findings (plain radiographs, magnetic resonance imaging [MRI], computed tomography [CT], or ultrasound) consistent with instability. A patient with hypermobile hip syndrome may exhibit a constellation of symptom severity, from microinstability to frank dislocation.” “The key distinction between laxity and instability is the absence (former) or presence (latter) of symptoms. Thus, ‘microinstability’, by definition, mandates the presence of symptoms.” |
Harris 2016 (23) Bellabarba 1998 (26) |
| Safran 2019 (6) | Microinstability of the hip – gaining acceptance | “Microinstability of the hip is defined as extraphysiologic hip motion that causes pain with or without symptoms of hip joint unsteadiness and may be the result of bony deficiency and/or soft-tissue damage or loss.” | Shu 2011 (17) |
| Mascarenhas 2020 (27) | Hip, pelvis and sacro-iliac joints | “The concept of microinstability is based on symptomatic hip laxity without marked subluxation. Aetiology may be either (1) traumatic (single or repetitive trauma) or (2) atraumatic (generalised laxity or developmental dysplasia of the hip (DDH)). Patients may feel hip unsteadiness, snapping, and/or pain during sports. Diagnosis is problematic, due to no established criteria.” | Cerezal 2012 (18) |
| Parvaresh 2021 (28) | Hip instability in the athlete: anatomy, etiology, and management | “The concept of hip microinstability emerged more recently as a clinical entity characterised by extraphysiologic motion resulting in hip pain or dysfunction with or without gross symptomatic instability. A diagnosis of instability may be challenging, because there are no objective criteria that are universally accepted for microinstability.” | Bolia 2016 (20), Safran 2019 (6), Kalisvaart 2015 (8) |
| Vera 2021 (29) | Hip instability in ballet dancers: a narrative review | “The difference between laxity and instability is the absence or presence of symptoms, respectively. Hip instability may present across a diverse spectrum from microinstability to frank dislocation. Thus, ‘microinstability,’ by definition, mandates the presence of symptoms.” “The nebulous term ‘microinstability’ may be better termed ‘the hypermobile hip syndrome’. Hypermobile hip syndrome may be defined as a triad of symptoms (unwanted or undesired subjective complaints), signs (physical examination abnormalities with excessive motion that provoke the inciting symptoms), and imaging findings (plain radiographs, magnetic resonance imaging [MRI], computed tomography [CT], or ultrasound) consistent with instability.” |
Mitchell 2016 (30), Harris 2016 (23), Harris 2015 (31), Kalisvaart 2015 (8) |
| Rosinsky 2022 (32) | Editorial commentary: hip joint laxity, microinstability, or instability require precise definition: no matter what you call it, it’s here to stay! | “The more common, and often interchangeable terms, are instability and microinstability … ‘instability’ has the advantage of conveying the significant impact the condition has on a patient’s life. On the other hand, ‘microinstability’ may more accurately reflect the vague clinical presentation that we often encounter in the average hip patient with instability. Most patients do not complain of symptoms commonly seen in other joints with ‘instability’, complaints such as giving way, subluxation, and recurrent dislocations. In the hip, the symptoms are generally less tangible, and hence, the term ‘microinstability’ may be more appropriate.” | Kalisvaart 2015 (8) |
| Martin 2022 (33) | Pre- and intraoperative decision-making challenges in hip arthroscopy for femoroacetabular impingement | “Hip instability or microinstability, defined as extraphysiologic hip movement causing pain, is now widely recognised as a cause of morbidity and dysfunction, particularly in young patients and athletes, and can co-exist in patients with FAI.” | Kalisvaart 2015 (8), Shu 2011 (17) |
| Wong 2022 (34) | Physical examination of the hip: assessment of femoroacetabular impingement, labral pathology, and microinstability | “Microinstability of the hip is defined as supraphysiologic hip motion that causes pain or discomfort with or without subjective unsteadiness of the joint, and it is believed to be caused by soft tissue injury or loss and/or bony deficiency related to developmental dysplasia of the hip, connective tissue disorders, trauma, idiopathic causes, and iatrogenic causes.” | Kalisvaart 2015 (8) |
FAI = femoroacetabular impingement; MR = magnetic resonance.
Diagnosis
Diagnosis of microinstability is rather straightforward if significant bony abnormalities or underlying connective tissue disorders are present that can explain the instability (8). However, diagnosis can be much more challenging in the case of idiopathic microinstability (6,8,35). There is no imaging modality, diagnostic or physical test alone that can be used to make a definitive diagnosis (6,8,19,,35). The diagnosis is more a pattern recognition of several clinical, radiological, and intraoperative signs. However, an international expert panel has developed a diagnostic tool comprising 34 criteria, which are categorized into “history”, “examination”, and “imaging” and hold diagnostic value (36).
Patients’ history. Patients’ history may provide helpful information for the diagnosis of microinstability (37). Patients may describe a painful pop (20,26,38), feeling of instability (1,38-40), pain, “hip giving away”, apprehension, snapping, clicking and catching, with or without hip impingement symptoms (6,8,20,23,25,28,29,36,38,40-44). The main symptom is mild to severe hip or groin pain and instability, with the typical “C-sign” pain location by making a “C” with the thumb and hand and placing it at the front and side of the hip (6,8,23,25,29,41,45) or pain located in the inguinal fold (1,46). Patients report activity-related pain, especially after end of range motion (29,44). Pain onset is either atraumatic and progressive, or after an acute trauma (44). Sports or other activities can sustain the symptoms and lead to persistent, constant pain (1,8,23,,25). After subluxation or dislocation, the capsuloligamentous structures may lose their stabilizing function and lead to microinstability (23).
People with connective tissue disorders (e.g. Ehlers-Danlos, Down syndrome) are at greater risk of microinstability (8,20,23,25,29,36). Clinicians need to ask about previous injuries and especially previous surgery (e.g. for dysplasia, cam osteoplasty, pincer resection, capsulotomy, labral tear, ligamentum teres tear, iliopsoas surgery), as there is possibility of iatrogenic instability (8,25,36). The probability of microinstability is higher in females (36,47) and in athletes involved in sports that require a large range of motion (ROM), such as gymnastics, dancing or martial arts (25). No study has been done to see what outcomes measure is best to identify hip microinstability. The two validated outcomes measures for non-arthritic hip pain in active patients are the International Hip Outcome Tool (iHOT) (48) and the Copenhagen Hip and Groin Outcome Score (HAGOS) (49).
Clinical examination. Sixteen studies were found reporting the diagnostic accuracy of different tests and radiological signs. Seven studies evaluated seven clinical tests (5,39,50-54) and eight studies reported on six radiological signs (2,3,55-60). One study presented an intraoperative pull test (7). Figure 3 depicts an overview of diagnostic accuracy.
People with hip microinstability show a higher prevalence of the following signs and symptoms: generalized ligamentous laxity (Beighton’s Physical Examination Criteria) (1,6,8,20,23,25,26,28,29,34,36,42-44,61), antalgic or abnormal gait patterns, or Trendelenburg sign (23,25,26,29,38,42).
Other tests to diagnose hip microinstability, such as increased ranges of motion (often increased rotation) (34,53,54,,61), the log roll test (external rotation recoil or hip dial test) (1,6,8,19,20,23,25,28,29,34,36,38,39,43,44,50,62), easy distraction of the joint (with apprehension) (6,19,20,25,28,29,34,38,44,63), internal rotation with over pressure (IROP) (63), pain with flexion, adduction, and internal rotation (FADIR), and posterior apprehension test (FADIR plus posterior force applied) have also been proposed (34,44). However, they usually lack the specificity to rule in microinstability (1,6,8,26,29). However, the hip dial test seems to be highly specific for the diagnosis of anterior capsular insufficiency in patients with FAI syndrome reporting a feeling of instability (39). The ROM threshold of hip flexion + rotation arc of ≥200° may help identify microinstability (53,54) (Fig. 3 and Supplementary Tab. A2).
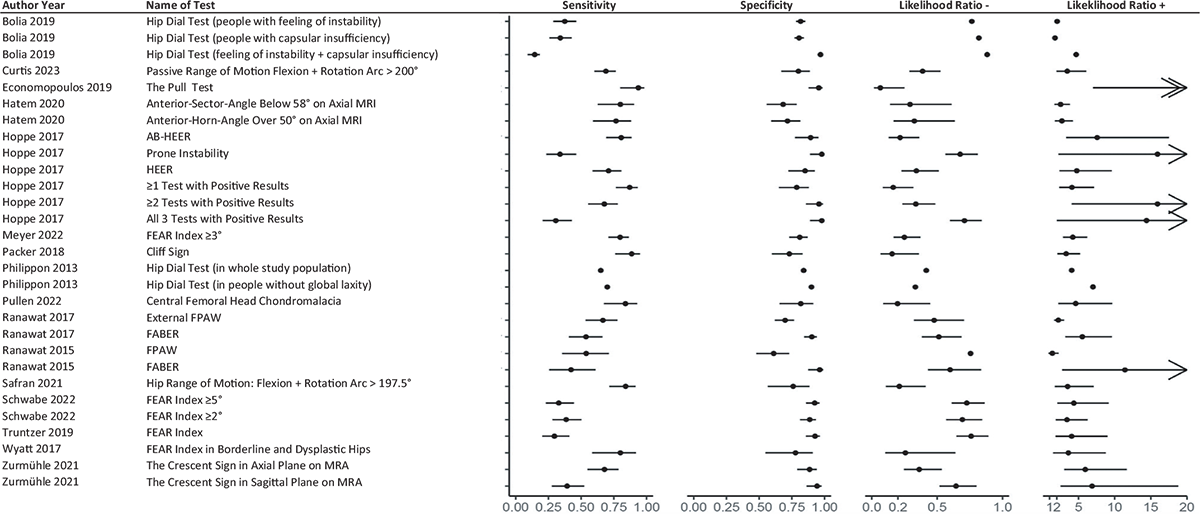
FIGURE 3 - Forest plots of diagnostic accuracy for clinical tests and radiological signs to detect hip microinstability. AB-HEER = abduction hyperextension external rotation; AI = acetabular index; AP = anterior posterior; CT = computed tomography; DDH = developmental dysplasia of the hip; FABER = flexion abduction external rotation; FEAR = femoro-epiphyseal acetabular roof; FPAW = foot progression angle walking; HEER = hyperextension external rotation; LCEA = lateral centre-edge angle; MRA = magnetic resonance arthrography; MRI = magnetic resonance imaging.
Additional special tests that have been described are: the posterior impingement test (hyperextension-external rotation [HEER], anterior apprehension) (1,5,6,8,19,20,28,29,34,36,38,42-44,47,61), FABER (flexion, abduction, and external rotation test with increased amount of external rotation compared with the unaffected side) (29,51,52,,64), FPAW (foot progression angle walking test) (51,52), hip pivot shift (25), and the posterior relocation test (65).
The abduction-hyperextension-external rotation (AB-HEER), the prone external rotation (5,6,8,34,37,44), and the HEER (anterior apprehension) test are well studied (5,33,44) and show small to substantial shifts in probability of having hip instability, especially when combined (Fig. 3 and Supplementary Tab. A2) (5,66,67). The Prone Apprehension Relocation Test (PART) is proposed to diagnose an anterior acetabular undercoverage, which may lead to anterior instability (68). Interrater reliability has been shown to be excellent (kappa 0.81, 95% confidence interval [CI] 0.69-0.93) (69). But this test was not validated against a gold standard that confirms hip instability.
Altered muscle activation patterns are typical in patients with microinstability of the hip (37,41). A useful clinical sign for hip microinstability is a reactive spasm of the secondary stabilizing muscles, such as the iliopsoas or the iliotibial (IT) band, which may be tender on palpation (43). Weakness may be present in those muscles, as well as in the abductor muscles (20,25,29,,37). The strength of the core, pelvic, hip, and lower extremity should be assessed (23).
Imaging
Radiography: X-ray/computed tomography (CT). Proposed X-ray views are anteroposterior pelvis view, standing false-profile view, supine Dunn (45°, 90°) or frog-leg lateral view, and hip splits view (8,23,29).
Subluxation is observed with manual traction on an anterior-posterior (AP) traction view (6,26,30,36,38) or in a splits position (6,20,30,,62). Subluxation is influenced by any dysplastic changes, larger alpha angle, and smaller femoral neck shaft angle (20,30).
Radiographic images are to be screened for significant acetabular and femoral abnormalities, such as dysplasia and FAI (decreased centre-edge angle [CEA] or lateral centre-edge angle [LCEA] <20-25°, Tönnis angle, acetabular inclination [AI] >13°, aspherical femoral head, higher alpha angle, coxa valga, coxa vara, anteversion of the femoral neck, retroversion of the acetabulum), all of which are regarded as risk factors for microinstability (1,6,8,19,27,29,33,36,38,42,43,47,59,62). Cam and pincer morphologies would create a levering effect and posterior translation (19,25). The hypermobile hip crevasse and anterior vertical chondro-osseous lesions can be observed (25), as well as a broken Shenton line, a positive crescent sign, and a distal femoral neck sclerosis (6,57,62,,70).
Three variables were associated with instability in borderline hip dysplasia (LCEA 20-25°) (71): AI, anterior centre-edge angle (ACEA), and maximum alpha angle. Odds ratio estimates and 95% CI limits were 1.50 (1.28-1.76), 0.92 (0.86-0.99), and 0.94 (0.90-0.98), respectively.
Several imaging markers are signs of hip instability and should be used in the context of each other: borderline acetabular dysplasia, increased femoral anteversion (>15°), a laterally oriented femoro-epiphyseal acetabular roof (FEAR) index, and anterior wall deficiency (2,6,33,36,44,45,56,58-60,62,72-75). They predicted worse outcomes (iHOT12) of hip femoral osteoplasty with or without labral repair for FAI in female patients (72). However, the optimal cut-off for the FEAR index remains to be established (60,74). A vacuum sign and a femoral head cliff sign are also described as diagnostic tools for instability (3,6,28,33,36,44,62).
A new score was developed for the prediction of instability in people with borderline dysplastic hips (BDH) (71): The Borderline Hip Instability Score (BHIS), considering four radiological and clinical signs (AI, ACEA, maximum alpha angle, and internal rotation in 90 degrees of flexion), demonstrated excellent predictive (discriminatory) ability with an area under the receiver operating characteristic (ROC) curve of 0.89 in the study population. In a population for external validation, the BHIS maintained an excellent area under the ROC curve of 0.92.
A FEAR index ≥4° is able to detect patients at risk of failure of arthroscopy for cam impingement combined with mild to moderate hip dysplasia, with 96% specificity (76).
People with FAI syndrome show a hip translation between neutral and FABER positions in CT images of a mean of 0.84 mm, mainly in the posterior inferior medial direction (77). Femoral anteversion must be considered; if there is more than 10-25° of femoral anteversion, FAI may arise, which is an additional factor for instability (1).
Magnetic resonance imaging (MRI)/Magnetic resonance arthrography (MRA). MRI or MRA helps to identify an increased femoral anteversion (44) or hip capsule laxity (6,20,28,,44). Muscle problems, iliopsoas and IT band tendonitis, labral tears, and chondral or ligamentum lesions can be observed (1,8,28,33,37,43,44,78). A traction view can demonstrate the vacuum sign, indicating abnormal distraction (8), with larger or easier widening of the hip joint during traction, suggesting hip laxity (27). Patients suspected to have hip microinstability may also have a thickened iliofemoral ligament with irregularities on the undersurface of the anterior capsule, and an increased capsular volume (27). Other findings associated with positive joint distraction were higher alpha angle, higher neck-shaft angle, smaller acetabular depth, and hypertrophy of the ligamentum teres (19,27,78). Widening of the anterior joint recess (>5 mm) and thinning of the anterior capsular (<3 mm), as well as accumulation of contrast in the posterior-inferior joint in ≥2 planes (6,33) can be seen. Increased intracapsular volume and anterosuperior capsular changes were found in iatrogenic instability after arthroscopy (79).
Dynamic ultrasound. Dynamic ultrasound showed excellent intra- and inter-rater reliability to measure anterior femoral head translation in participants with no hip pathology or functional limitation (intra-rater Intraclass Correlation Coefficients [ICCs] from 0.794 to 0.945, inter-rater ICCs from 0.725 to 0.846) (24). However, in order to achieve good clinical results and outcomes it is important to clarify whether that technique is truly valid for symptomatic patients with microinstability, and whether the magnitude of instability can be precisely measured and integrated into a treatment algorithm (80). In patients with hip pain and clinical suspicion of either instability or impingement, the inter-rater reliability to measure anterior femoral head translation of ≥2 mm provoked by either the figure of 4 or AB-HEER manoeuvres for the diagnosis of microinstability was substantial (kappa 0.606, 95%CI 0.221-0.991) (81).
Intraoperative testing. Anterior capsular insufficiency is shown in patients with FAI without generalized laxity or dysplasia (39). Widening of the anterior joint recess (>5 mm) and anterior capsular thinning (<3 mm) lateral to the zona orbicularis are associated with capsular laxity (6,64,82). However, the correlation of anterior joint recess width (>5 mm) with hip laxity is not yet proven (82). Hip laxity can be confirmed with displacement of the hip with minimal amount of traction force (6,7,33,36,40,64,82-85) or if there is no hip reduction after release of negative intra-articular pressure and traction prior to the start of hip arthroscopy (82,83). Labrum separation, chondral damage, and ligamentum teres tears or hypertrophy can be seen intraoperatively (6,85), with typical inside-out chondral wear of the acetabulum and central femoral head wear (33,85). In patients with FAI who have labral hypertrophy, the hypertrophy is a significant clinical indicator of subtle hip dysplasia and hip microinstability; hence there can be an overlap of FAI and dysplasia characteristics (86).
One study (87) proposed the “Divot” sign as a useful arthroscopic sign of hip microinstability. Of 690 cases of primary hip arthroscopy, 14 hips had a “Divot” sign, and all had risk factors for hip microinstability.
Miscellaneous. To complete the physical examination, before any further investigations are made, an intra-articular hip injection of local anaesthetics can help to confirm a diagnosis of intra-articular pathology (8,44). However, no differentiation can be made between hip microinstability and FAI. In both conditions synovial inflammation has been found (88). Despite this, synovitis scores were lower in the hip microinstability group compared with the FAI group, which also had cartilage damage (88). The presence of synovial inflammation in both groups supports an inflammatory component in the pathogenesis of non-arthritic hip pathology (88).
In patients with femoral head chondromalacia undergoing hip arthroscopy for FAI and/or instability, central head chondromalacia was associated with 84% sensitivity, 82% specificity, 81% positive predictive value, and 84% negative predictive value for a diagnosis of microinstability (89). Hip microinstability was defined as patients with symptoms of intra-articular hip pain with concomitant intraoperative laxity of the symptomatic joint.
As hip microinstability leads to an excessive translation of the femur in the acetabulum, changes in the dynamic loading of the hip can be observed (41). The magnitude of acceleration during gate cycle shows that the axial, anteroposterior, and mediolateral accelerations differ significantly in people with hip instability compared with healthy asymptomatic controls (41). The axial and mediolateral acceleration values were higher, and the anteroposterior acceleration was lower in the microinstability group compared with the FAI group.
Prevalence
Eleven articles presented or enabled calculation of the prevalence of microinstability with or without signs of hip impingement (2,3,5,7,51,52,56,59,60,90,91) (Supplementary Tab. A3). The prevalence of microinstability with FAI was in the range of 21%-42%, in adults undergoing hip arthroscopy or MRA of the hip. The prevalence of instability without FAI was in the range 27% (in patients with unilateral hip or groin pain) to 57% (in patients with suspicion of microinstability who underwent hip arthroscopy), except in a sample with borderline acetabular dysplasia, where it was 62.9%. Population size range was 39-953 hips investigated. All subjects were people with hip pain or who had undergone hip arthroscopy.
Aetiology
A total of 49 articles reported on contributing or risk factors for the development of hip microinstability. In general, it is stated that hip microinstability is a multifactorial disorder. It can be a cause for, or a consequence of, multiple pathological conditions of the hip. These may be osseous, chondrolabral, capsuloligamentous, musculotendinous, or neuromuscular dysfunctions of the kinetic chain (23,25,29).
Aetiologies are classified into six categories: (i) significant bony abnormalities, such as developmental dysplasia of the hip (DDH), (ii) connective tissue disorders, (iii) post-traumatic, (iv) microtraumatic, (v) iatrogenic, and (vi) idiopathic (6,8,28). In the absence of significant bony abnormalities, the pathology originates primarily in the supporting soft tissue (26).
FAI may induce instability in the following four ways (23): (1) excessive acetabular anteversion, resulting in posterior acetabular rim impingement and anterior hip instability; (2) excessive acetabular retroversion, resulting in anterior impingement and posterior instability; (3) excessive femoral anteversion, resulting in posterior acetabular rim impingement and anterior hip instability; and (4) excessive femoral retroversion, resulting in anterior impingement and posterior instability. The combination of borderline dysplasia and FAI with an increased femoral anteversion leads to worse instability in extension (92).
FAI may lead to instability and, vice versa, the excessive femoral head translation relative to the acetabulum may contribute to the FAI pathomechanism, with a potential mechanical overloading of the hip structures, leading to pain (67,93), central femoral head wear, and subluxation (89). In addition, an increasingly frequent indication for revision arthroscopy for FAI is capsular complication and subsequent hip instability (61,94,95).
Table 2 gives an overview of all mentioned risk factors or contributing factors for hip microinstability.
| Risk factors or contributing factors for hip microinstability | Details |
|---|---|
| Overuse | Microtrauma caused by repetitive axial loading (with external rotation or abduction) with motion to or beyond the limits, such as in hockey, golf, football, ballet or gymnastics, leads to repeated injury or elongation of the capsule and to labral tears (8,18-20,22,23,28,33,37,38,42,96). This increases the forces on the other static stabilizers. Injury of the ilio-, pubo- and ischiofemoral ligament, and the ligamentum teres may contribute to microinstability (8,20,29,37,38,42,44,97). Disruption of the soft tissue affects the stability because of loss of coupling force (98). Labral tears may induce loss of suction seal effect and worsen instability through subluxation (42,44,63). In addition, the labrum has a nociceptive and a proprioceptive function. When injured, the altered sensory information may affect joint stability (20). The labrum is constantly stressed in the dancer’s hip and the hip capsule is frequently thinner (29). With a torn labrum and a thin capsule, the hip may show instability (29,33). |
| FAI | Cam or pincer morphology can also induce microinstability, by excessive acetabular anteversion (advanced posterior bone contact and anterior instability), acetabular retroversion (advanced anterior bone contact and posterior instability), excessive femoral anteversion (posterior cam effect and anterior instability), or excessive femoral retroversion (anterior cam effect and posterior instability), and thus increase the risk of subluxation (1,23,63,67,92,98,99). |
The osseous impingement at end of motion positions may lead to levering of the femoral head out of the socket (8,30) and to posterior chondral and capsular-labral junction injury (“contrecoup” injury), and therefore, to secondary subluxation or dislocation (1,6,17,19,28,30,99-101), especially in the athlete with FAI, where the functional ROM required is often greater than the limited physiological motion allowed by the cam and/or rim impingement lesions (23,99,101). In end of range movements, a FAI occurs that leads to subluxation, even without pincer or cam morphology, seen in ballet dancers (29,30,102). Women show greater subluxation than men during the “grand écart facial” position, with increasing subluxation with larger alpha angles and smaller neck-shaft angles (30). Increased flexion and internal rotation may lead to impingement between the cam and the anterior acetabulum and levering of the femoral head posteriorly (23,99), with posterior acetabular rim fracture and posterior capsulolabral tear, analogous to a posterior bony Bankart lesion of the shoulder (19,101). In addition, the repetitive abutment of the femur head-neck junction against the acetabulum may lead to trauma of the anterior labrum and stretch of the capsule and capsular ligaments (6). This increases the movement of the femoral head and may result in subluxation (38,103). Furthermore, there is risk of a primary anteroinferior impingement through abutment of the prominence of the medial femoral metaphysis and/or anteroinferior border of the acetabulum in extension and internal rotation (104). A posterior extra-articular ischiofemoral impingement can cause secondary anterior instability of the femur in extension (104). These patients show anteroinferior abrasion of the cartilage with rupture and degeneration of the labrum, similar to a posteroinferior contrecoup lesion that can be seen with anterior pincer impingement (104). In extreme end of range motions, for example, in ballet dancers, an insufficient femoral version leads to a posterior impingement of the femoral neck on the acetabulum that results in anterior subluxation (29). FAI causes migration of the femoral head, thus the relation of the head and the acetabulum alters. This increases shear forces and leads to microinstability (105). |
|
| Hip arthroscopy | Hip arthroscopy may lead to microinstability (20). Excessive resection of the acetabular bone while managing pincer morphology may induce subluxation or migration of the femoral head out of the acetabulum (23,28,97). Also, overcorrection of cam morphologies can lead to instability (23,28,98,106,107). Overzealous capsulotomy without repair after arthroscopy for FAI or capsulectomy can result in iatrogenic instability (6,8,20,22,23,28,61,94,95,98,100,108-111). Excessive labrum or ligamentum teres resection or psoas tenotomy may also be an iatrogenic cause (1,23,28). In general, previous arthroscopy may lead to increased distractibility of the hip joint compared with the native hip (84). |
| PAO | Acetabular retroversion and high to normal femoral version treated with anteverting PAO can lead to anterior instability (92). |
| Special osseous morphologies | Lack of acetabular coverage/dysplasia or borderline dysplasia may lead to atraumatic instability (1,6,8,19,28,29,33,38,42,44,63,112). An increased femoral anteversion and a coxa valga will contribute to further instability, even more in case of a borderline hip, while a decreased femoral version would contribute to increasing impingement (1,33,113). Extra-articular bone impingement, especially between the greater trochanter and pelvis (1). A coxa vara demonstrates ischiofemoral/greater trochanter impingement, particularly with abduction/side splits in ballet dancers, with subluxation of the femoral head (29). |
| Ligamentous laxity, soft-tissue disorders, capsular laxity/thin capsule | Soft-tissue disorders (e.g. Ehlers-Danlos syndrome), ligamentous and capsular laxity, or a thin capsule may result in atraumatic instability (1,8,19,23,26,28,29,33,38,42,44,114). Abnormal joint forces are the result of capsular laxity that may lead to labral injuries and femoral neck impingement at high flexion “secondary impingement” (18). |
| Legg-Calvé-Perthes disease | Legg-Calvé-Perthes disease leads to significant impingement that develops secondary dysplasia and thus instability (38). |
| Increased translational motion in the hip joint | Instability leads to an increased movement of the femoral head in the hip joint potentially causing cartilage wear, degenerative changes, and capsular stress. It also places the labrum at risk of shear injury and microtrauma, further contributing to pathological articular changes (45,97). |
| Deep hip muscle weakness | Weakness of deep hip muscles results in instability and overactivation of secondary movers. This may result in an anterior gliding of the femoral head and exaggerate anterior joint loading (44,93). FAI morphologies may enhance this loading and result in labrum alterations (93). |
| Ligamentum teres tears | There is a possible interrelationship between FAI, labral tears, and ligamentum teres pathology (115,116). Trauma, overuse at end of range motion, FAI, and other osseous risk factors for instability, such as borderline dysplasia, may result in ligamentum teres injury (112,115). Ligamentum teres tears contribute to microinstability and damage of the labrum and the cartilage with sporting activities (18,117,118). People with complete tears are more likely to exhibit capsular laxity (115). In patients with chondrolabral dysfunctions associated with FAI, approximately 90% had a partially or completely torn ligamentum teres and they were 3.6 times more likely to have capsular laxity (116). Thus, torn ligamentum teres may lead to microinstability (116). Of 20 subjects with complete ligamentum teres ruptures all had labral pathology and evidence of FAI, with 19 cam and 1 pincer. Of these, five out of nine subjects contacted for follow-up noted instability (117). |
FAI, femoroacetabular impingement; PAO = periacetabular osteotomy; ROM, range of motion.
Treatment
There is consensus that the first-line treatment for hip microinstability is conservative management based on modifiable factors. Strengthening, sensorimotor training, activity modification, and education are proposed. In addition, non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections can be used. There is a lack of RCTs evaluating the effectiveness of different treatment modalities in patients with hip microinstability. Surgical management is indicated if conservative treatment of 3-6 months fails and symptoms last for at least 6 months (6,8,25,28,33,43,119,120). Surgical procedures are performed either by arthroscopy or open surgery. They target redirectional osteotomies, capsular and labral management, and address intra-articular bony pathology with acetabuloplasty for pincer and femoral osteoplasty for cam morphology. It is essential to determine why the hip is unstable before considering surgery of the capsule, bones, or soft tissue. Additionally, intraoperative hip testing and re-testing can help uncover additional causes of impingement or instability once the primary causes are addressed. Table 3 gives an overview of treatment options for hip microinstability.
A retrospective case series study showed that two-thirds of patients with microinstability were able to avoid surgery and had improved clinical outcome scores after hip and core strengthening exercises two times a week for 6 weeks plus home exercises (121).
Different non-RCT intervention studies showed clinical improvement after surgical intervention. In a pre-post cohort study of 25 patients without dysplasia undergoing periacetabular osteotomy (PAO) because of hip pain and/or instability after failure of arthroscopy (128), 18 patients (72%) reached the minimal clinically important improvement in the modified Harris hip score (mHHS) and in the iHOT-33 at 6 months follow-up. Favourable and significant pre-post improvements were also shown for patient-reported outcomes (mHHS, visual analogue scale [VAS] for pain, Hip Outcome Score – Sport-Specific Score, Non-Arthritic Hip Score) in 65 high-level athletes after primary arthroscopy in the setting of borderline dysplasia and hip microinstability (131). In addition, high rates of return to sports were achieved (80.7%). In 140 patients undergoing hip arthroscopy for FAIS with a standard post-operative rehabilitation protocol, 19 patients had hip instability (FEAR index ≥2°), whereas 121 patients did not (FEAR index <2°). Both groups had similar improvement in 2-year outcomes (132). Another 32 females with atraumatic microinstability, with anterior labral and cartilage pathology, were treated with arthroscopy and capsular plication without any bony resections (133). There was significant clinical pre-post improvement in pain and function. However, in a retrospective case series study of 27 hips with microinstability treated with combined arthroscopy and open capsular plication in the absence of acetabular dysplasia or severe femoral anteversion, 45% had reoperation (arthroscopy, femoral osteotomy, or PAO) and persistent symptoms (129).
Poor surgical prognostic factors for patients with dysplastic hip microinstability are a broken Shenton’s line, a femoral neck-shaft angle >140°, a lateral CEA <19°, and a body mass index (BMI) >23 kg/m2 (28).
| Treatment options | In detail | References |
|---|---|---|
| Conservative management | ||
| Strengthening | Iliopsoas, hip abductors, adductors, external rotators, gluteus maximus, core muscles, low back, iliocapsularis, rectus femoris, TFL, hamstrings | (1,6,8,20,23,29,33,43-45,93,121) |
| Stretching | Iliotibial band, hamstrings, rectus femoris, abdominal muscles | (1,23) |
| Sensorimotor training | Neuromuscular rehabilitation to address functional deficits | (28,29,93) |
| Activity modification | Education, relative rest, activity modification (avoidance of provocative manoeuvres), adaptive sport activities | (1,6,8,20,25,28,29,33,38,43,44) |
| Medication/injection | Non-steroidal anti-inflammatory drugs, oral non-opioids, corticosteroid injections in conjunction with local anaesthetic | (1,6,8,18,20,23,25,28,29,37,38,43,44) |
| Physical therapy | Multimodal rehabilitation exercises | (18,23,25,28,37,38,120,122) |
| Surgical management | ||
| Capsular management | Capsular closure after arthroscopy, repair, suture, reduction of capsular volume by plication or capsulorrhaphy, as well as capsular management in the setting of revision arthroscopy | (1,6,8,18,20,23,25,29,33,37,38,42-46,61,96,97,120,123-126) |
| Iliofemoral ligament | Ligament repair, length restoration | (42,97,123) |
| Ligamentum teres | Reconstruction | (1,23,29,75,120) |
| Labrum | Labral repair, refixation, reconstruction, debridement, graft (to recreate suction seal effect) | (1,6,8,20,25,33,37,38,44,127) |
| Osteotomy, osteoplasty | Periacetabular osteotomy, femoral osteotomy, acetabuloplasty, femoral osteoplasty, address FAI morphologies | (1,6,8,20,23,25,28,29,33,37,43,75,92,128-130) |
FAI = femoroacetabular impingement; TFL = tensor fasciae latae.
Two case series studies showed substantial improvement in function for patients after revision surgery with capsular repair, who had iatrogenic hip microinstability after a first arthroscopy (134,135).
Cam and pincer morphology, as well as hip dysplasia may lead to labrum and adjacent acetabular cartilage damage (136,137). In a cohort of 75 patients, 55% failed conservative treatment and needed surgical procedure (118). The best predictor for failure of conservative treatment was a tear of the ligamentum teres (118). The authors claimed that people with a torn ligamentum teres develop subtle hip instability.
Special case borderline dysplasia and FAI. Borderline dysplasia might lead either to instability or to impingement of the hip (113). Decision-making for the optimal surgical treatment in case of borderline dysplasia is extremely difficult (130), especially if there is excessive femoral anteversion (138). No clinical standards exist to decide if there is significant structural instability, or FAI and microinstability, or no instability (130). Instability related to acetabular dysplasia or retroversion would be treated with PAO, while FAI (with or without instability) could be treated with arthroscopy, via capsulotomy during PAO, or with an open surgical hip dislocation (130). Arthroscopy could potentially replace PAO for soft-tissue related instability and FAI in patients with borderline dysplasia (139). Modern PAO, however, is done with additional arthroscopy, such as acetabular resection or femoral head-neck offset decompression, to address bony morphologies leading to FAI (113,130).
Discussion
This scoping review included 123 studies and collected evidence on five main topics: definition, diagnosis, aetiology, prevalence, and treatment of hip microinstability. There are numerous types of evidence reporting on the concept of hip microinstability and its context with FAI. The main findings of this review are described below.
Different definitions for hip microinstability exist. A standardized terminology should be established (80). Supraphysiological motion or excessive motion of the femoral head is mentioned, but the term “hip microinstability” should be used only when the centre of rotation of the femoral head is not stable in the acetabulum, that is, when there is excessive femoral head movement within the acetabulum (1,18). However, there is no objective quantification and cut-off for excessive movement. A classification system should be established to facilitate future clinical studies (32,80).
Diagnosis is a puzzle of history, clinical examination, radiographic and intraoperative signs. An international expert panel published a consensus study for the diagnosis of microinstability (36). They propose a diagnostic tool in a tabular format with 34 criteria deemed to have diagnostic value. Another international expert consensus conference showed strong agreement on eight operating room criteria to confirm hip microinstability (85). The experts propose using this list as a basis for further research to build a scoring or weighting system for the diagnosis of hip instability. Data relating to the items should be recorded prospectively, so that the relative importance of the items to symptoms and treatment response could be stratified.
Hip microinstability and FAI may be associated, they can occur in combination, and they may aggravate each other (1). Cam and pincer seem to predispose the hip joint to instability by a multifactorial mechanism, consisting of abnormal osseous morphologies, weakened static stabilizers, and dynamic factors (140).
The static and dynamic stabilizers of the hip joint are well described, for example, the role of the capsule or the deep hip muscles. However, there is no data regarding dynamic or static hip instability and its contributors. There are some mechanical factors that may lead to a dynamic instability, such as cam and pincer morphology or femoral retroversion (141). Other mechanical factors, such as hip dysplasia and femoral anteversion, may lead to static instability (141). This topic requires further exploration.
Symptomatic hip microinstability with additional FAI morphologies is present in 21%-42% of adults undergoing hip arthroscopy or MRA of the hip. The main symptom in both conditions is pain. Both conditions require symptoms to be diagnosed, but not all patients with radiographic signs of instability or FAI morphologies are symptomatic (91,142,143). Therefore, it should be investigated why some people develop symptoms and others do not.
Researchers suggest the same conservative treatment strategies for hip microinstability and FAI patients. They conducted several RCTs to show the effectiveness of conservative versus surgical treatment in FAI (10-13). However, they do not explain the treatment propositions in detail, and the frequencies of treatment vary greatly. Consequently, researchers lack a clear description of an appropriate non-operative treatment for hip microinstability and FAI. Casartelli et al (93) proposed active physical therapy aimed at improving hip neuromuscular function. If the passive stability mechanisms are inadequate, the muscular system needs to augment stability (144). To enhance joint stability, deep hip stabilizing muscles should be retrained, following the same rationale as strengthening the local muscles before the more superficial ones at the spine and shoulder (144). There is evidence that the local stabilizing muscles can improve function, reduce pain, and restore normal feedforward response in other joints, such as the knee, the lumbar and the cervical spine (145-147). The dynamic stability of the hip joint needs to be improved and the anterior gliding of the femoral head minimized in people with hip microinstability. Hence, hip flexor and abductor muscles and the deep hip external rotators need to be strengthened (144). Feedforward mechanisms are needed for normal postural activity, and they can be trained by repeated voluntary activation of a muscle (146). Attention and motor imagery are important for improved motor performance and greater transfer to task performance (146).
The surgical treatment of hip microinstability differs considerably between pure instability and pure FAI. Often there is a combination of both problems, especially in the case of BDH. Intra-articular pathologies, such as ligamentum teres tears, pincer or cam morphologies, should be addressed, because, if not treated, they may further create hip instability (75). If the instability part is overseen and surgical intervention is only made to correct the bony impingement, the risk of increasing the instability is high. To differentiate whether a BDH has instability or impingement characteristics they propose using the FEAR index. However, there is no absolute consensus for the cut-off value of the FEAR index (73). Hence, an in-depth analysis of the situation before choosing the surgical intervention is crucial. There is large consensus that the capsule should be repaired after arthroscopic surgery for FAI, to avoid iatrogenic microinstability.
Limitations and strengths
The difficulty of clear diagnostic criteria and definition of hip microinstability may have led to under- or over-inclusion of papers in this review. The scientific rigour of the included studies was not investigated, therefore there is no grading of evidence. Overall, there is a lack of high-quality RCTs for the management of patients with hip microinstability.
A sensitive search was performed, resulting in a large number of papers being included in this study. This allowed a comprehensive overview of the topic and resulted in sensibilization of the association between hip microinstability and FAI.
Conclusions and implications for research and practice
Microinstability of the hip lacks consistent objective evaluative criteria. A standardized terminology should be established. Furthermore, consensus is necessary regarding physical examination, diagnostic criteria, and a classification system of hip microinstability. Only with consistent, quantitative, and valid diagnostic criteria can clinicians and researchers start to examine target populations and build high-quality research projects with clear research questions. Hip microinstability and FAI may be associated; they can occur in combination and may aggravate each other. There is a lack of evidence regarding the feasibility and effectiveness of effective training in reducing symptoms in people with hip microinstability with or without FAI. We need RCTs in this population with targeted training to assess the effectiveness of the interventions under evaluation. Furthermore, we need larger studies on sports performance and long-term outcomes for athletes. Further research is necessary to enable clinicians to confidently manage hip microinstability, also in the context of FAI.
Disclosures
Conflict of interest: The authors have no conflicts of interest to disclose.
Funding and financial support: The authors have no funding and financial support to disclose.
Authors’ contributions: CR contributed to the conception of the work, undertook the literature review, prepared figures and tables, authored and reviewed drafts of the article, and approved the final draft. DB authored or reviewed drafts of the article and approved the final draft. JT authored or reviewed drafts of the article and approved the final draft. JMS authored or reviewed drafts of the article and approved the final draft. TR undertook the literature review, prepared figures, reviewed drafts of the article, and approved the final draft. QB undertook the literature review, prepared figures, reviewed drafts of the article, and approved the final draft. RH contributed to the conception of the work, undertook the literature review, prepared figures and tables, authored or reviewed drafts of the article, and approved the final draft.
Data Availability Statement: Data sharing not applicable: No new data was created or analysed in this study and more data is available as supplementary material to this article.
References
- 1. Dangin A, Tardy N, Wettstein M, May O, Bonin N. Microinstability of the hip: a review. Orthop Traumatol Surg Res. 2016;102(8S):S301-S309. CrossRef PubMed
- 2. Truntzer JN, Hoppe DJ, Shapiro LM, Safran MR. Can the FEAR index be used to predict microinstability in patients undergoing hip arthroscopic surgery? Am J Sports Med. 2019;47(13):3158-3165. CrossRef PubMed
- 3. Packer JD, Cowan JB, Rebolledo BJ, et al. The Cliff Sign: a new radiographic sign of hip instability. Orthop J Sports Med. 2018;6(11):2325967118807176. CrossRef PubMed
- 4. Reiman MP, Agricola R, Kemp JL, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54(11):631-641. CrossRef PubMed
- 5. Hoppe DJ, Truntzer JN, Shapiro LM, Abrams GD, Safran MR. Diagnostic accuracy of 3 physical examination tests in the assessment of hip microinstability. Orthop J Sports Med. 2017;5(11):2325967117740121. CrossRef PubMed
- 6. Safran MR. Microinstability of the hip – gaining acceptance. J Am Acad Orthop Surg. 2019;27(1):12-22. CrossRef PubMed
- 7. Economopoulos KJ, Kweon CY, Gee AO, Morris ST, Hassebrock JD, Chhabra A. The pull test: a dynamic test to confirm hip microinstability. Arthrosc Sports Med Rehabil. 2019;1(1):e67-e74. CrossRef PubMed
- 8. Kalisvaart MM, Safran MR. Microinstability of the hip – it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2(2):123-135. CrossRef PubMed
- 9. Duncan ST, Bogunovic L, Baca G, Schoenecker PL, Clohisy JC. Are there sex-dependent differences in acetabular dysplasia characteristics? Clin Orthop Relat Res. 2015;473(4):1432-1439. CrossRef PubMed
- 10. Griffin DR, Dickenson EJ, Wall PDH, et al; FASHIoN Study Group. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225-2235. CrossRef PubMed
- 11. Hunter DJ, Eyles J, Murphy NJ, et al. Multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapist-led care for femoroacetabular impingement (FAI) syndrome on hip cartilage metabolism: the Australian FASHIoN trial. BMC Musculoskelet Disord. 2021;22(1):697. CrossRef PubMed
- 12. Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med. 2018;46(6):1306-1314. CrossRef PubMed
- 13. Palmer AJR, Ayyar Gupta V, Fernquest S, et al; FAIT Study Group. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ. 2019;364:l185. CrossRef PubMed
- 14. Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3-10. CrossRef PubMed
- 15. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. CrossRef PubMed
- 16. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. CrossRef PubMed
- 17. Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30(2):349-367. CrossRef PubMed
- 18. Cerezal L, Arnaiz J, Canga A, et al. Emerging topics on the hip: ligamentum teres and hip microinstability. Eur J Radiol. 2012;81(12):3745-3754. CrossRef PubMed
- 19. Suter A, Dietrich TJ, Maier M, Dora C, Pfirrmann CW. MR findings associated with positive distraction of the hip joint achieved by axial traction. Skeletal Radiol. 2015;44(6):787-795. CrossRef PubMed
- 20. Bolia I, Chahla J, Locks R, Briggs K, Philippon MJ. Microinstability of the hip: a previously unrecognized pathology. Muscles Ligaments Tendons J. 2016;6(3):354-360. CrossRef PubMed
- 21. Jackson TJ, Peterson AB, Akeda M, et al. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2016;44(3):689-695. CrossRef PubMed
- 22. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162-173. CrossRef PubMed
- 23. Harris JD, Gerrie BJ, Lintner DM, Varner KE, McCulloch PC. Microinstability of the hip and the splits radiograph. Orthopedics. 2016;39(1):e169-e175. CrossRef PubMed
- 24. d’Hemecourt PA, Sugimoto D, McKee-Proctor M, et al. Can dynamic ultrasonography of the hip reliably assess anterior femoral head translation? Clin Orthop Relat Res. 2019;477(5):1086-1098. CrossRef PubMed
- 25. Harris JD. Hypermobile hip syndrome. Oper Tech Sports Med. 2019;27(3):108-118. CrossRef
- 26. Bellabarba C, Sheinkop MB, Kuo KN. Idiopathic hip instability. An unrecognized cause of coxa saltans in the adult. Clin Orthop Relat Res. 1998;(355):261-271. PubMed
- 27. Mascarenhas VV, Castro MO, Afonso PD. Hip, pelvis and sacro-iliac joints. In: Vanhoenacker FM, Maas M, Gielen JL, eds. Imaging of orthopedic sports injuries. Medical radiology. Springer, Cham 2020; 353-422. CrossRef
- 28. Parvaresh KC, Rasio J, Azua E, Nho SJ. Hip instability in the athlete: anatomy, etiology, and management. Clin Sports Med. 2021;40(2):289-300. CrossRef PubMed
- 29. Vera AM, Nho SJ, Mather RC, Wuerz TH, Harris JD. Hip instability in ballet dancers: a narrative review. J Dance Med Sci. 2021;25(3):176-190. CrossRef PubMed
- 30. Mitchell RJ, Gerrie BJ, McCulloch PC, et al. Radiographic evidence of hip microinstability in elite ballet. Arthroscopy. 2016;32(6):1038-1044.e1. CrossRef PubMed
- 31. Harris JD, Slikker W, Abrams GD, Nho SJ. Atraumatic instability and surgical technique. In: Nho S, Leunig M, Larson C, Bedi A, Kelly B, eds. Hip arthroscopy and hip joint preservation surgery. New York: Springer 2015; 1001-1014. CrossRef
- 32. Rosinsky PJ. Editorial commentary: hip joint laxity, microinstability, or instability require precise definition: no matter what you call it, it’s here to stay! Arthroscopy. 2022;38(10):2850-2851. CrossRef PubMed
- 33. Martin H, Robinson PG, Maempel JF, et al. Pre- and intraoperative decision-making challenges in hip arthroscopy for femoroacetabular impingement. Bone Joint J. 2022;104-B(5):532-540. CrossRef PubMed
- 34. Wong SE, Cogan CJ, Zhang AL. Physical examination of the hip: assessment of femoroacetabular impingement, labral pathology, and microinstability. Curr Rev Musculoskelet Med. 2022;15(2):38-52. CrossRef PubMed
- 35. Jean PO, Safran MR, Ayeni OR. Hip microinstability: fact or fiction? Knee Surg Sports Traumatol Arthrosc. 2023;31(1):1-3. CrossRef PubMed
- 36. Khanduja V, Darby N, O’Donnell J, et al; International Microinstability Expert Panel. Diagnosing hip microinstability: an international consensus study using the Delphi methodology. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):40-49. CrossRef PubMed
- 37. Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25(2):309-326, ix-x. ix-x. CrossRef PubMed
- 38. Boykin RE, Anz AW, Bushnell BD, Kocher MS, Stubbs AJ, Philippon MJ. Hip instability. J Am Acad Orthop Surg. 2011;19(6):340-349. CrossRef PubMed
- 39. Bolia I, Briggs KK, Philippon MJ. High specificity of the hip dial test to diagnose anterior capsular insufficiency in patients with FAI-related microinstability of the hip. Arthrosc - J Arthrosc Relat Surg. 2019;35:e29-e. CrossRef
- 40. Parvaresh KC. Editorial commentary: axial stress examination under anesthesia provides a highly reliable test for measurement of hip distraction. Arthroscopy. 2022;38(5):1478-1479. CrossRef PubMed
- 41. Neira A, Amenabar T, Cristi-Sánchez I, et al. Evaluation of atraumatic hip instability measured by triaxial accelerometry during walking. J Hip Preserv Surg. 2019;6(2):134-139. CrossRef PubMed
- 42. Philippon MJ, Zehms CT, Briggs KK, Manchester DJ, Kuppersmith DA. Hip instability in the athlete. Oper Tech Sports Med. 2007;15(4):189-194. CrossRef
- 43. Smith MV, Sekiya JK. Hip instability. Sports Med Arthrosc Rev. 2010;18(2):108-112. CrossRef PubMed
- 44. Curtis DM, Murray IR, Money AJ, Pullen WM, Safran MR. Hip microinstability: Understanding a newly defined hip pathology in young athletes. Arthroscopy. 2022;38(2):211-213. CrossRef PubMed
- 45. Lall AC, Walsh JP, Maldonado DR, et al. Teamwork in hip preservation: the ISHA 2019 annual scientific meeting. J Hip Preserv Surg. 2020;7(suppl 1):2-21. CrossRef PubMed
- 46. Cohen D, Jean PO, Patel M, et al. Hip microinstability diagnosis and management: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):16-32. CrossRef PubMed
- 47. Curtis DM, Pullen WM, Murray IR, Money AJ, Segovia N, Safran MR. Female gender, decreased lateral center edge angle and a positive hyperextension-external rotation test are associated with ease of hip distractability at time of hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2188-2194. CrossRef PubMed
- 48. Mohtadi NG, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595-605; quiz 606-10.e1. CrossRef PubMed
- 49. Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45(6):478-491. CrossRef PubMed
- 50. Philippon MJ, Briggs KK, Goljan P, Peixoto LP. The hip dial test to diagnose symptomatic hip instability. Arthroscopy. 2013;29(10):e123. CrossRef
- 51. Ranawat AS, Gaudiani MA, Slullitel PA, Satalich J, Rebolledo BJ. Foot progression angle walking test: a dynamic diagnostic assessment for femoroacetabular impingement and hip instability. Orthop J Sports Med. 2017;5(1):2325967116679641. CrossRef PubMed
- 52. Ranawat AS, Park C, Licatesi T, Rebolledo BJ, Satalich J. Foot progression angle walking test – an effective dynamic test for the diagnosis of femoroacetabular impingement and hip instability. Orthop J Sports Med. 2015;3(7_suppl 2):2325967115S00140. CrossRef
- 53. Curtis DM, Pullen WM, Hopkins JN, et al. Can hip passive range of motion predict hip microinstability? A comparative study. Orthop J Sports Med. 2023;11(6):23259671231169978. CrossRef PubMed
- 54. Safran MR, Hopkins J, Elisman K, Finlay A, Segovia NA. Can hip microinstability be predicted by hip range of motion. J ISAKOS. 2021;6(6):494.
- 55. Hatem MA, Helal A, Khoury AN, Martin HD. Anteroinferior hip instability in flexion during dynamic arthroscopic examination is associated with abnormal anterior acetabular horn. Orthop J Sports Med. 2020;8(12):2325967120965564. CrossRef PubMed
- 56. Wyatt M, Weidner J, Pfluger D, Beck M. The Femoro-Epiphyseal Acetabular Roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475(3):861-869. CrossRef PubMed
- 57. Zurmühle CA, Kuner V, McInnes J, Pfluger DH, Beck M. The crescent sign – a predictor of hip instability in magnetic resonance arthrography. J Hip Preserv Surg. 2021;8(2):164-171. CrossRef PubMed
- 58. Meyer AM, Schaver AL, Cohen BH, Glass NA, Willey MC, Westermann RW. FEAR index in predicting treatment among patients with femoroacetabular impingement and hip dysplasia and the relationship of femoral version. J Hip Preserv Surg. 2022;9(2):84-89. CrossRef PubMed
- 59. Schwabe M, Pascual-Garrido C, Clohisy J, Graesser E, Nepple J. Acetabular dysplasia: three-dimensional deformity predictors of the diagnosis of symptomatic instability treated with periacetabular osteotomy. Orthop J Sports Med. 2020;8(7_suppl 6):2325967120S00426. CrossRef
- 60. Schwabe MT, Clohisy JC, A Graesser E, Pascual-Garrido C, Nepple JJ. External validation of the FEAR index in borderline acetabular dysplasia. Orthop J Sports Med. 2022;10(8):23259671221113837. CrossRef PubMed
- 61. Larson CM. Editorial commentary: restoration of hip capsular tension is more important than repair construct configuration. Arthroscopy. 2022;38(12):3149-3151. CrossRef PubMed
- 62. Woodward RM, Vesey RM, Bacon CJ, White SG, Brick MJ, Blankenbaker DG. Microinstability of the hip: a systematic review of the imaging findings. Skeletal Radiol. 2020;49(12):1903-1919. CrossRef PubMed
- 63. Berthelot JM, Brulefert K, Arnolfo P, Le Goff B, Darrieutort-Laffite C. Update on contribution of hip labral tears to hip pain: a narrative review. Joint Bone Spine. 2023;90(1):105465. CrossRef PubMed
- 64. Magerkurth O, Jacobson JA, Morag Y, Caoili E, Fessell D, Sekiya JK. Capsular laxity of the hip: findings at magnetic resonance arthrography. Arthroscopy. 2013;29(10):1615-1622. CrossRef PubMed
- 65. Maas R, Wallentine S, Gerke D, Crager S, Stewart J. Posterior hip instability relocation testing: a resident’s case report. J Man Manip Ther. 2017;25(4):215-220. CrossRef PubMed
- 66. Reiman MP, Décary S, Mathew B, Reiman CK. Accuracy of clinical and imaging tests for the diagnosis of hip dysplasia and instability: a systematic review. J Orthop Sports Phys Ther. 2019;49(2):87-97. CrossRef PubMed
- 67. Gowd AK, Beck EC, Trammell AP, Edge C, Stubbs AJ. Evaluation of additional causes of hip pain in patients with femoroacetabular impingement syndrome. Front Surg. 2022;9:697488. CrossRef PubMed
- 68. Spiker AM, Fabricant PD, Wong AC, Suryavanshi JR, Sink EL. Radiographic and clinical characteristics associated with a positive PART (Prone Apprehension Relocation Test): a new provocative exam to elicit hip instability. J Hip Preserv Surg. 2020;7(2):288-297. CrossRef PubMed
- 69. Watchmaker LE, Hetzel SJ, Sink EL, Spiker AM. Interrater reliability of the prone apprehension relocation test. Orthop J Sports Med. 2021;9(9):23259671211032229. CrossRef PubMed
- 70. MacDonald AA, Blankenbaker DG, Brick MJ, Hanna CM, Woodward RM. The posterior crescent sign on MRI and MR arthrography: is it a marker of hip dysplasia and instability? Skeletal Radiol. 2023;52(6):1127-1135. CrossRef PubMed
- 71. Graesser E, Rhea L, Pascual-Garrido C, et al. Development and external validation of a novel clinical score to quantify the presence of instability characteristics in patients with borderline acetabular dysplasia. Orthop J Sports Med. 2020;8(7_suppl 6):2325967120S00431. CrossRef
- 72. Horton B, West H, Marl J, Wylie J. Imaging markers of hip instability are associated with worse outcomes at two to four-year follow-up in female patients undergoing hip arthroscopy for femoroacetabular impingement. American Orthopaedic Society for Sports Medicine (AOSSM), 2020 Annual Meeting (Virtual). Orthop J Sports Med. 2020;8:1-2.
- 73. Cohen D, Ifabiyi M, Mathewson G, et al. The radiographic femoroepiphyseal acetabular roof index is a reliable and reproducible diagnostic tool in patients undergoing hip-preservation surgery: a systematic review. Arthroscopy. 2023;39(4):1074-1087.e1. CrossRef PubMed
- 74. Dusak IWS, Ciatawi K. The application of the novel femoral-epiphyseal acetabular roof (FEAR) index. Orthop J Sports Med. 2023;11(2 suppl):2325967121S00914. CrossRef
- 75. Atzmon R, Safran MR. Arthroscopic treatment of mild/borderline hip dysplasia with concomitant femoroacetabular impingement – literature review. Curr Rev Musculoskelet Med. 2022;15(4):300-310. CrossRef PubMed
- 76. Foissey C, Abid H, Martinot P, Cazor A, Thaunat M. Predictive radiological parameters of failure following surgical management of femoroacetabular impingement associated with borderline acetabular dysplasia. Orthop Traumatol Surg Res. 2023;109(4):103349. CrossRef PubMed
- 77. Cvetanovich GL, Beck EC, Chalmers PN, et al. Assessment of hip translation in vivo in patients with femoracetabular impingement syndrome using 3-dimensional computed tomography. Arthrosc Sports Med Rehabil. 2020;2(2):e113-e120. CrossRef PubMed
- 78. Agten CA, Sutter R, Buck FM, Pfirrmann CW. Hip imaging in athletes: sports imaging series. Radiology. 2016;280(2):351-369. CrossRef PubMed
- 79. Featherall J, O’Neill DC, Mortensen AJ, Tomasevich KM, Metz AK, Aoki SK. Three-dimensional magnetic resonance arthrography of post-arthroscopy hip instability demonstrates increased effective intracapsular volume and anterosuperior capsular changes. Arthrosc Sports Med Rehabil. 2021;3(6):e1999-e2006. CrossRef PubMed
- 80. Maldonado DR. CORR Insights®: can dynamic ultrasonography of the hip reliably assess anterior femoral head translation? Clin Orthop Relat Res. 2019;477(5):1099-1100. CrossRef PubMed
- 81. Sahr ME, Endo Y, Sink EL, Miller TT. Dynamic ultrasound assessment of hip instability and anterior and posterior hip impingement. Skeletal Radiol. 2023;52(7):1385-1393. CrossRef PubMed
- 82. Packer JD, Foster MJ, Riley GM, et al. Capsular thinning on magnetic resonance arthrography is associated with intra-operative hip joint laxity in women. J Hip Preserv Surg. 2020;7(2):298-304. CrossRef PubMed
- 83. Curtis DM, Pullen WM, Murray IR, Money A, Safran M. The diagnosis of hip microinstability is correlated with ease of intra-operative hip distraction. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):33-39. CrossRef PubMed
- 84. Mortensen AJ, Tomasevich KM, Ohlsen SM, O’Neill DC, Featherall J, Aoki SK. Previous arthroscopic hip surgery increases axial distractibility compared to the native contralateral hip and may suggest instability. Arthroscopy. 2022;38(5):1466-1477. CrossRef PubMed
- 85. Safran MR, Murray IR, Andrade AJ, et al. Criteria for the operating room confirmation of the diagnosis of hip instability: the results of an international expert consensus conference. Arthroscopy. 2022;38(10):2837-2849.e2. CrossRef PubMed
- 86. Nwachukwu BU, Gaudiani MA, Marsh NA, Ranawat AS. Labral hypertrophy correlates with borderline hip dysplasia and microinstability in femoroacetabular impingement: a matched case-control analysis. Hip Int. 2019;29(2):198-203. CrossRef PubMed
- 87. Rosinsky PJ, Mayo BC, Kyin C, et al. The femoral head “divot” sign: a useful arthroscopic sign of hip microinstability. Orthop J Sports Med. 2020;8(5):2325967120917919. CrossRef PubMed
- 88. Abrams GD, Luria A, Sampson J, et al. Decreased synovial inflammation in atraumatic hip microinstability compared with femoroacetabular impingement. Arthroscopy. 2017;33(3):553-558. CrossRef PubMed
- 89. Pullen WM, Curtis DM, Safran MR. Central femoral head chondromalacia is associated with a diagnosis of hip instability. Arthrosc Sports Med Rehabil. 2021;4(2):e453-e457. CrossRef PubMed
- 90. Shibata KR, Matsuda S, Safran MR. Is there a distinct pattern to the acetabular labrum and articular cartilage damage in the non-dysplastic hip with instability? Knee Surg Sports Traumatol Arthrosc. 2017;25(1):84-93. CrossRef PubMed
- 91. Tibor LM, Liebert G, Sutter R, Impellizzeri FM, Leunig M. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res. 2013;471(12):3762-3773. CrossRef PubMed
- 92. Westermann RW, Willey MC. Femoral version in hip arthroscopy: does it matter? Sports Med Arthrosc Rev. 2021;29(1):28-34. CrossRef PubMed
- 93. Casartelli NC, Maffiuletti NA, Bizzini M, Kelly BT, Naal FD, Leunig M. The management of symptomatic femoroacetabular impingement: what is the rationale for non-surgical treatment? Br J Sports Med. 2016;50(9):511-512. CrossRef PubMed
- 94. Selley R, Lawton C, Dooley M, et al. Capsular complications and subsequent instability on the rise as indications for revision hip arthroscopy. Orthop J Sports Med. 2021;9(10_suppl 5). CrossRef
- 95. Mortensen AJ, Metz AK, Froerer DL, Aoki SK. Hip capsular deficiency – a cause of post-surgical instability in the revision setting following hip arthroscopy for femoroacetabular impingement. Curr Rev Musculoskelet Med. 2021;14(6):351-360. CrossRef PubMed
- 96. Bayer JL, Sekiya JK. Hip instability and capsular laxity. Oper Tech Orthop. 2010;20(4):237-241. CrossRef
- 97. Bowman KF Jr, Fox J, Sekiya JK. A clinically relevant review of hip biomechanics. Arthroscopy. 2010;26(8):1118-1129. CrossRef PubMed
- 98. Canham CD, Domb BG, Giordano BD. Atraumatic hip instability. JBJS Rev. 2016;4(5):17. CrossRef PubMed
- 99. Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470(12):3390-3397. CrossRef PubMed
- 100. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27(12):1720-1731. CrossRef PubMed
- 101. Hammoud S, Bedi A, Voos JE, Mauro CS, Kelly BT. The recognition and evaluation of patterns of compensatory injury in patients with mechanical hip pain. Sports Health. 2014;6(2):108-118. CrossRef PubMed
- 102. Charbonnier C, Kolo FC, Duthon VB, et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39(3):557-566. CrossRef PubMed
- 103. Blakey CM, Field MH, Singh PJ, Tayar R, Field RE. Secondary capsular laxity of the hip. Hip Int. 2010;20(4):497-504. CrossRef PubMed
- 104. Tibor LM, Ganz R, Leunig M. Anteroinferior acetabular rim damage due to femoroacetabular impingement. Clin Orthop Relat Res. 2013;471(12):3781-3787. CrossRef PubMed
- 105. Eijer H, Hogervorst T. Femoroacetabular impingement causes osteoarthritis of the hip by migration and micro-instability of the femoral head. Med Hypotheses. 2017;104:93-96. CrossRef PubMed
- 106. Hunt SA. Editorial commentary: hip cam overresection may result in inferior outcomes: the Goldilocks paradox of too little, too much, or just right? Arthroscopy. 2021;37(9):2817-2819. CrossRef PubMed
- 107. Jackson TJ. Editorial commentary: microinstability after cam osteochondroplasty results from over-resection – everything in moderation. Arthroscopy. 2021;37(1):171-172. CrossRef PubMed
- 108. Friel N, Ukwuani G, Nho SJ. Current techniques in treating femoroacetabular impingement: capsular repair and plication. Am J Orthop (Belle Mead NJ). 2017;46(1):49-54. PubMed
- 109. Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34(1):303-318. CrossRef PubMed
- 110. Woodward RM, Philippon MJ. Persistent or recurrent symptoms after arthroscopic surgery for femoroacetabular impingement: a review of imaging findings. J Med Imaging Radiat Oncol. 2019;63(1):15-24. CrossRef PubMed
- 111. Tahoun MF, Lizano-Díez X, Soler BC, Pons MT. Superior outcomes after arthroscopic treatment of femoroacetabular impingement and labral tears with closed versus open capsule. Knee Surg Sports Traumatol Arthrosc. 2023;31(10):4501-4509. CrossRef PubMed
- 112. Wu JY, Li W, Xu LY, Zheng G, Chen XD, Shen C. Ligamentum teres tears and increased combined anteversion are associated with hip microinstability in patients with borderline dysplasia. Arthroscopy. 2024;40(3):745-751. CrossRef PubMed
- 113. Nepple JJ, Fowler LM, Larson CM. Decision-making in the borderline hip. Sports Med Arthrosc Rev. 2021;29(1):15-21. CrossRef PubMed
- 114. Featherall J, Froerer D, Mortensen A, Aoki S, Metz A. Poster 195: inverse relationship of hip capsular thickness on magentic resonance imaging and increased axial distraction under anesthesia: further characterization of hip laxity. Orthop J Sports Med. 2022;10(7_suppl 5):2325967121S0075. CrossRef
- 115. Martin RL, McDonough C, Enseki K, Kohreiser D, Kivlan BR. Clinical relevance of the ligamentum teres: a literature review. Int J Sports Phys Ther. 2019;14(3):459-467. CrossRef PubMed
- 116. Chahla J, Soares EAM, Devitt BM, et al. Ligamentum teres tears and femoroacetabular impingement: prevalence and preoperative findings. Arthroscopy. 2016;32(7):1293-1297. CrossRef PubMed
- 117. Martin RL, Palmer I, Martin HD. Ligamentum teres: a functional description and potential clinical relevance. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1209-1214. CrossRef PubMed
- 118. Kaya M, Kano M, Sugi A, Sakakibara Y, Yamashita T. Factors contributing to the failure of conservative treatment for acetabular labrum tears. Eur Orthop Traumatol. 2014;5(3):261-265. CrossRef
- 119. Swarup I, Zaltz I, Robustelli S, Sink E. Outcomes of periacetabular osteotomy for borderline hip dysplasia in adolescent patients. J Hip Preserv Surg. 2020;7(2):249-255. CrossRef PubMed
- 120. Matthewson G, Williams A, Macciacchera M, Shahabinezhad A, Duong A, Ayeni OR. Effective management options for treatment of microinstability of the hip: a scoping review. Curr Rev Musculoskelet Med. 2023;16(1):9-18. CrossRef PubMed
- 121. Ejnisman L, Elisman K, Safran MR. Effectiveness of nonoperative management of hip microinstability. Am J Sports Med. 2022;50(4):1013-1019. CrossRef PubMed
- 122. Savic M, D’Angelo K. Exploring the role of microinstability of the hip: an atypical presentation of femoroacetabular impingement (FAI) and labral tear in a collegiate endurance athlete: a case report. J Can Chiropr Assoc. 2019;63(3):187-196. PubMed
- 123. Beck EC, Alter T, Mehta N, et al. Contemporary hip capsular management and closure using a suture passing device. Arthrosc Tech. 2019;8(9):e947-e952. CrossRef PubMed
- 124. Wylie J, Beckmann J, Maak T, Aoki S. Capsular repair for instability following hip arthroscopy for femoroacetabular impingement: preliminary outcomes and description of surgical technique. Arthroscopy. 2013;29(12):e206-e207. CrossRef
- 125. Charles T, Jayankura M, Laude F. Treatment of hip microinstability with arthroscopic capsular plication: a retrospective case series. Hip Pelvis. 2023;35(1):15-23. CrossRef PubMed
- 126. Wolff AB, Scanaliato JP. Editorial commentary: the importance of capsular closure following hip arthroscopy – leave no trace: an outdoorsman’s ramblings. Arthroscopy. 2022;38(11):3041-3042. CrossRef PubMed
- 127. Wu ZX, Ren WX, Ren YM, Tian MQ. Arthroscopic labral debridement versus labral repair for patients with femoroacetabular impingement: a meta-analysis. Medicine (Baltimore). 2020;99(19):e20141. CrossRef PubMed
- 128. Brusalis CM, Peck J, Wilkin GP, et al. Periacetabular osteotomy as a salvage procedure: early outcomes in patients treated for iatrogenic hip instability. J Bone Joint Surg Am. 2020;102(suppl 2):73-79. CrossRef PubMed
- 129. Nepple JJ, Ambastha C, Abu-Amer W, Clohisy JC. Mid-term outcomes of combined hip arthroscopy and limited open capsular plication in the non-dysplastic hip. Iowa Orthop J. 2021;41(1):133-139. PubMed
- 130. Nepple JJ. Editorial commentary: at the intersection of borderline dysplasia and femoroacetabular impingement – which way should we turn? Arthroscopy. 2020;36(4):1185-1188. CrossRef PubMed
- 131. Jimenez AE, Monahan PF, Miecznikowski KB, et al. Achieving successful outcomes in high-level athletes with borderline hip dysplasia undergoing hip arthroscopy with capsular plication and labral preservation: a propensity-matched controlled study. Am J Sports Med. 2021;49(9):2447-2456. CrossRef PubMed
- 132. Wong SE, Newhouse AC, Wichman DM, Bessa F, Williams J, Nho SJ. Patients with a high femoroepiphyseal roof with concomitant borderline hip dysplasia and femoroacetabular impingement syndrome do not demonstrate inferior outcomes following arthroscopic hip surgery. Arthroscopy. 2022;38(5):1509-1515. CrossRef PubMed
- 133. Kalisvaart MM, Safran MR. Hip instability treated with arthroscopic capsular plication. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):24-30. CrossRef PubMed
- 134. O’Neill DC, Mortensen AJ, Cannamela PC, Aoki SK. Clinical and radiographic presentation of capsular iatrogenic hip instability after previous hip arthroscopy. Am J Sports Med. 2020;48(12):2927-2932. CrossRef PubMed
- 135. Wylie JD, Beckmann JT, Maak TG, Aoki SK. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44(1):39-45. CrossRef PubMed
- 136. Leunig M, Beaulé PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467(3):616-622. CrossRef PubMed
- 137. Parvizi J, Bican O, Bender B, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24(6)(suppl):110-113. CrossRef PubMed
- 138. Curley AJ, Domb BG. Editorial commentary: evaluate for the Beighton Score and additional radiographic signs of instability prior to proceeding with hip arthroscopy in patients with combined borderline hip dysplasia and excessive femoral anteversion. Arthroscopy. 2023;39(4):978-980. CrossRef PubMed
- 139. Hohmann E. Editorial commentary: hip arthroscopy for femoroacetabular impingement in patients with borderline dysplasia does not result in inferior outcomes compared with outcomes in patients without dysplasia: do not fear. Arthroscopy. 2022;38(5):1516-1518. CrossRef PubMed
- 140. Canham CD, Yen YM, Giordano BD. Does femoroacetabular impingement cause hip instability? A systematic review. Arthroscopy. 2016;32(1):203-208. CrossRef PubMed
- 141. Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy. 2011;27(2):235-251. CrossRef PubMed
- 142. Philippon MJ, Ho CP, Briggs KK, Stull J, LaPrade RF. Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med. 2013;41(6):1357-1362. CrossRef PubMed
- 143. Heerey J, Agricola R, Smith A, et al. The size and prevalence of bony hip morphology do not differ between football players with and without hip and/or groin pain: findings from the force cohort. J Orthop Sports Phys Ther. 2021;51(3):115-125. CrossRef PubMed
- 144. Retchford TH, Crossley KM, Grimaldi A, Kemp JL, Cowan SM. Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact. 2013;13(1):1-12. PubMed
- 145. Cowan SM, Bennell KL, Hodges PW, Crossley KM, McConnell J. Simultaneous feedforward recruitment of the vasti in untrained postural tasks can be restored by physical therapy. J Orthop Res. 2003;21(3):553-558. CrossRef PubMed
- 146. Tsao H, Hodges PW. Immediate changes in feedforward postural adjustments following voluntary motor training. Exp Brain Res. 2007;181(4):537-546. CrossRef PubMed
- 147. Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27(17):1835-1843. CrossRef PubMed