 |
Arch Physioter 2024; 14: 20-28 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3023 REVIEW |
 |
Impact of direct access on the quality of primary care musculoskeletal physiotherapy: a scoping review from a patient, provider, and societal perspective
ABSTRACT
Introduction: Worldwide many countries provide direct access in physiotherapy. The aim of this scoping review was to synthesize the available evidence on the quality of primary care musculoskeletal physiotherapy from different perspectives.
Methods: Systematic searches were conducted in three databases up to September 2022. Studies were included when regarding assessment of at least one of the following perspectives: patient (quality of Life, patient satisfaction, pain, functioning, adverse events), provider (treatment compliance, responsibility, liability, status, prestige, job satisfaction), and society (number of referrals, amount of medical imaging, medication use, number of sessions needed for rehabilitation, and overall costs and cost-effectiveness). Selection and methodological quality assessment of systematic reviews were performed. Data extraction and analysis were performed separately for systematic reviews and individual primary studies.
Results: Five systematic reviews as well as 17 primary studies were included. From a patient perspective, no significant effect of direct access was found for pain and a tendency in favour of direct access was found for quality of life, functioning, and well-being. Concerning providers, higher treatment compliance was found in direct access to physiotherapy and decision-making was more accurate. From a societal perspective, significant differences in favour of direct access physiotherapy were found for waiting time, prescribed medication, and medical imaging. In addition, there was a tendency towards lower health care costs.
Conclusions: Emerging evidence suggests that direct access physiotherapy could provide at least equal quality of care for patients and better opportunities for providers and the society on selected outcomes.
Keywords: Direct access, Physiotherapy, Quality of care, Scoping review
Received: January 19, 2024
Accepted: June 5, 2024
Published online: July 1, 2024
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What is already known
- Direct access physiotherapy has proven to be a valid strategy in primary musculoskeletal care.
What this study adds
- The article brings together the results of previous systematic reviews and additionally includes those of recent randomized controlled trials. The review suggests that direct access physiotherapy could provide at least equal quality of care for patients and better opportunities for providers and society compared to physiotherapy on referral.
Introduction
Musculoskeletal (MSK) disorders are among the top ten leading causes of years lived with disability (YLD) (1,2). Mounting evidence suggests that the quality of care offered in primary care settings treating these MSK disorders is suboptimal and that often inaccurate diagnoses are made by primary care physicians (3,4). Physiotherapy is a frequently recommended treatment option for the management of MSK disorders (5). Responses to the latest World Confederation for Physical Therapy survey reveal direct access (DA) is available in 48 countries and there is no restriction on private practice in 77 countries (6). In countries where physiotherapists receive professional autonomy through DA, evidence suggests several benefits including a more valid diagnosis as compared to primary care physicians, better outcomes for patients, and more efficient use of resources, while maintaining high patient satisfaction (5,7).
Further benefits can be linked to DA physiotherapy, such as shorter waiting times, reduced health care costs including physician fees, medical imaging expenses, and medication costs (5,8), increased prestige for physiotherapists (9,10), and decreased workload for primary care physicians (10). However, cost reduction may be restricted to direct costs and general workload for the Physical Therapist (PT) may not necessarily be reduced (11). Also, potential disadvantages to this model of health care have been described, for instance, potential erosion of a strong patient-doctor relationship (12,13) or a robust physiotherapy-doctor connection (13), as well as concerns about overconsumption of physiotherapy services (14).
This scoping review aimed to identify, appraise, and synthesize existing literature to assess the impact of DA on primary care physiotherapy for patients presenting with various MSK disorders. The impact of DA will focus on outcomes from the perspectives of the patient, the provider, and society.
Methods
The reporting of this scoping review conforms to the PRISMA Extension for Scoping Reviews (PRISMA-ScR) guidelines (15).
MEDLINE (PubMed) and Web of Science were searched from 1990 until March 2024. The electronic search strategy used in these searches is listed in Table 1.
| (“referral and consultation”[MeSH Terms] OR “direct access” OR “self-referred” OR “self-referral” OR “primary care”) AND (physical therapy modalities[MeSH Terms] OR modality physical therapy[MeSH Terms] OR “physical therapy” OR “physiotherapy” OR “physical therapist” OR “physiotherapist” OR “rehabilitation”[MeSH Terms]) AND (“quality of life”[MeSH Terms] OR “assessment”, “outcomes”[MeSH Terms] OR “pain”[MeSH Terms] OR “back pain” OR “neck” OR “musculoskeletal subjective reporting” OR “discomfort” OR “injuries”[MeSH Terms] OR “trauma” OR “disability” OR “activities” OR “recovery” OR “safety” OR “sick leave”[MeSH Terms] OR “patient satisfaction”[MeSH Terms] OR “disability” OR “disability leave” OR “disability leaves” OR “illness days” OR “cost-effectiveness” OR “economic evaluation” OR “cost analysis” OR “analyses cost”[MeSH Terms] OR “cost” OR “cost projection analysis”) |
Titles and abstracts were independently reviewed by two reviewers up to March 2024, applying the following inclusion criteria: availability of quantitative data of at least one group that received physiotherapy through DA or direct allocation without consulting a physician and assessment of at least one of the perspectives for the patient (quality of life [QoL], well-being, satisfaction, pain, functioning, or adverse events), physiotherapists (treatment compliance, responsibility, liability, status, prestige, or job satisfaction), and society (number of referrals with and without a DA setting, amount of medical imaging, medication use, number of sessions needed for rehabilitation, and overall costs and cost-effectiveness). Articles written in English, Dutch, or French were considered. Papers not complying with the inclusion criteria were excluded. Randomized clinical trials were selected and studies retrieved by the above search string which were published after the latest systematic review were added to this scoping review.
The Risk of Bias in Systematic Reviews (ROBIS) tool was developed specifically to be used by guideline developers, authors of overviews of systematic reviews (“reviews of reviews”), and review authors who might want to assess or avoid risk of bias in their reviews (16). The ROBIS tool was utilized by two reviewers independently to assess the risk of bias in the included systematic reviews. Discrepancies between the two reviewers were resolved by discussion and if disagreement persisted, a third reviewer made the final decision.
Results
The flow of studies through the review is presented in Fig. 1.
Systematic reviews
Five systematic reviews were included in this scoping review. Table 2 summarizes the authors and dates of the primary studies included in each of these reviews. From this overview, it can be concluded that, overall, 56 individual studies were covered. Each of the reviews employed its own methodological quality evaluation protocol regarding the included studies (see Tab. 3). Regarding the assessment based on the ROBIS tool, one review showed an overall low risk of bias (17). On each of the different domains, at least one study scored low risk of bias and all domains were scored at high risk in at least one study. Data collection was scored as unclear for two studies. Overall bias in one study was considered unclear and in the three remaining there was a high risk.
Patient perspective
The low risk of bias review by Babatunde et al (17) found no significant differences in pain reduction between DA physiotherapy and care supervised by a general practitioner (GP). Similar findings were reported by Piscitelli et al (18) and Demont et al (19), although small differences in favour of DA physiotherapy were noticed (p = 0.76) (18). Ojha et al (20) reported a significant but small result for pain reduction in favour of DA physiotherapy (p = 0.011).
Babatunde et al (17) reported no significant results for QoL and function while Ojha et al (20) and Piscitelli et al (18) showed better outcomes in terms of QoL and function in favour of DA physiotherapy (p = 0.04 and p = 0.03, respectively). According to Ojha et al (20) and Demont et al (19), patients reported 5.0-21.5% greater satisfaction in the DA groups than in physician referral groups (p < 0.01). Additionally, Gallotti et al (21) reported equal to superior QoL and a tendency to higher patient satisfaction in DA groups.
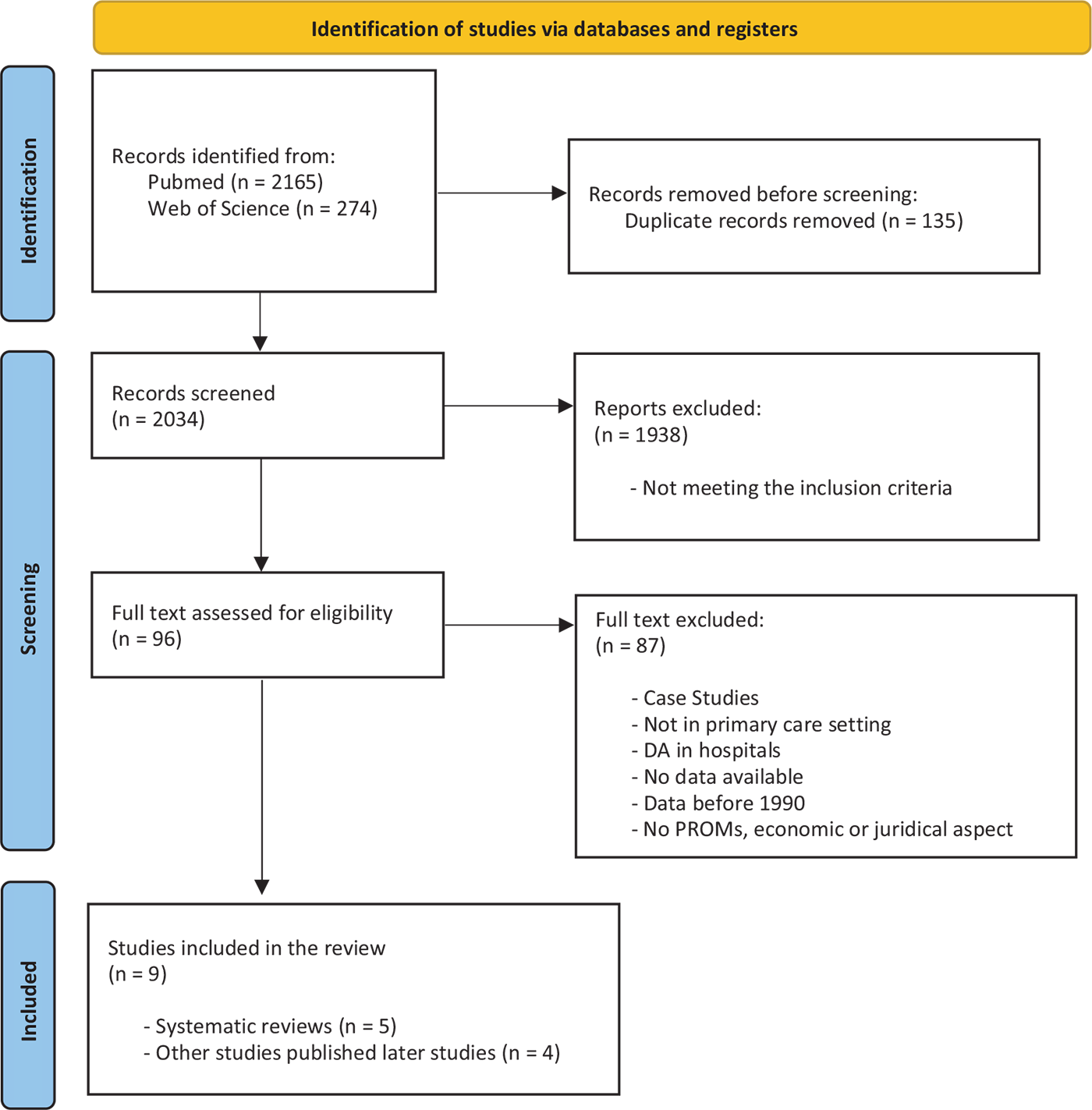
FIGURE 1 - PRISMA flow chart of the study selection.
Physiotherapist perspective
Piscitelli et al (18) and Demont et al (19) both showed significantly higher treatment compliance in DA physiotherapy compared to GP referral physiotherapy (p = 0.004). No other results were reported on aspects of the physiotherapists’ perspective.
Societal perspective
Piscitelli et al (18) and Demont et al (19) concur that DA physiotherapy can reduce the waiting time for primary consults by 4 to 63 days (p < 0.001). Similarly, Gallotti et al (21) reported shorter waiting times as well as improved management accuracy regarding the type of access to PT (i.e. by GP referral, access by consultant, or DA physiotherapy).
Four out of five systematic reviews showed consistent results regarding the amount of prescribed medication and medication use (17-20). DA physiotherapy led to 11.9-65.0% less prescribed medication (p < 0.01) and reduced pharmacological costs by $42-710 (p < 0.01) (17,20).
Ojha et al (20) reported significantly fewer physiotherapy visits in a DA setting, with a range of 1.1-13.4 visits (p < 0.01). Demont et al (19) found no consensus about the number of physiotherapy visits, with either two to three fewer physiotherapy visits needed in a DA setting (p = 0.001) or no significant difference found. Babatunde et al (17) and Piscitelli et al (18) reported that DA physiotherapy led to 2.0-21.5% fewer follow-up visits with the primary care physician (p < 0.05). Gallotti et al. (21) indicate a shorter time to discharge in DA. Demont et al (19) reported that 17% fewer patients required a primary care physician visit in a DA physiotherapy setting (p = 0.0113).
| Ojha et al 2014 (n = 8) | Piscitelli et al 2018 (n = 12) | Demont et al 2019 (n = 18) | Babatunde et al 2020 (n = 26) | Gallotti et al 2023 (n = 28) |
|---|---|---|---|---|
| Hackett et al 1993 | Gentle et al 1984 | Overman et al 1988 | Greenfield et al 1975 | Daker-White et al 1999 |
| Mitchell et al 1997 | Hackett et al 1993 | Holdsworth et al 2004 | Mitchell et al 1997 | Oldmeadow et al 2007 |
| Holdsworth et al 2004 | Mitchell et al 1997 | Moore et al 2005 | Overman et al 1988 | Sephton et al 2010 |
| Moore et al 2005 | Holdsworth et al 2004 | Holdsworth et al 2006 | Ferguson et al 1999 | Ludvigsson et al 2012 |
| Holdsworth et al 2007 | Holdsworth et al 2006 | Holdsworth et al 2007 | Moore et al 2005 | Phillips et al 2012 |
| Webster et al 2008 | Holdsworth et al 2007 | Brooks et al 2008 | Holdsworth 2007/2008 | Kooijman et al 2013 |
| Leemrijse et al 2008 | Leemrijse et al 2008 | Leemrijse et al 2008 | Bossonnaulth et al 2010 | Salisbury et al 2013 |
| Pendergast et al 2012 | Brooks et al 2008 | Webster et al 2008 | Pendergast et al 2012 | Mallett et al 2014 |
| Webster et al 2008 | Ludvigsson et al 2012 | Phillips et al 2012 | O’farrell et al 2014 | |
| Ludvigsson et al 2012 | Pendergast et al 2012 | Chetty et al 2012 | Samsson et al 2014 | |
| Pendergast et al 2012 | Mallett et al 2014 | Ludvigsson et al 2012 | Bornhöft et al 2015 | |
| Badke et al 2014 | Swinkels et al 2014 | McCallum et al 2012 | Samsson et al 2015 | |
| Bishop et al 2017 | Bomhöft et al 2015 | McGill et al 2013 | Bird et al 2016 | |
| Mintken et al 2015 | Badke et al 2014 | Kerridge-Weeks et al 2016 | ||
| Goodwin et al 2016 | Mallett et al 2014 | Samsson et al 2016 | ||
| Bishop et al 2017 | Swinkels et al 2014 | Bishop et al 2017 | ||
| Bomhöft et al 2019 | Bornhöft et al 2015 | Chang et al 2018 | ||
| Downie et al 2019 | Mintken et al 2015 | Bornhöft et al 2019 | ||
| Ojha et al 2015 | Caffrey et al 2019 | |||
| Boissonnaulth et al 2016 | Downie et al 2019 | |||
| Goodwin et al 2016 | Lankhorst et al 2020 | |||
| Harland et al 2016 | Ojha et al 2020 | |||
| Pearson et al 2016 | Oostendorp et al 2020 | |||
| Bishop et al 2017 | Peterson et al 2021 | |||
| Mant et al 2017 | Ho-Henrikson et al 2022 | |||
| Denninger et al 2018 | Lyons et al 2022 | |||
| Szymanek et al 2022 |
Shaded sections refer to primary studies that have been analysed also in previous systematic reviews.

FIGURE 2 - Risk of bias assessment of included systematic reviews (n = 5).
Four systematic reviews concluded that DA physiotherapy could lead to 6.3-70.0% fewer X-rays and other medical imaging (p < 0.001) (17,18, 20,21). Babatunde et al (17) and Piscitelli et al (18) also showed lower overall health costs (p < 0.01) up to 20%. Ojha et al (20) and Demont et al (19) showed decreased costs in a DA physiotherapy setting compared to a GP referral setting (p < 0.05). This was further supported by Gallotti et al (21).
Babatunde et al (17) and Gallotti et al (21) reported less work-related absence and sick leave in DA physiotherapy. Ojha et al (20) reported an average of 17.4 days less work absence in a DA physiotherapy. Piscitelli et al (18) did not find a consensus for the return-to-work rate. They found either no difference in return-to-work rate or 14.1% less lost time from work and daily duties (p < 0.05).
| First author (year of publication) | Patient perspective | Physiotherapist perspective | Societal perspective |
|---|---|---|---|
| Ojha et al (2014) (20) | Significantly less average pain was reported in DA. (VAS decreased from 5.7 to 2.7 vs. from 5.7 before treatment to 3.2 after treatment; p = 0.011.) Higher improvement in function in DA (79% vs. 60%; p = 0.04). Higher levels of satisfaction in DA (79%-93.2% vs. 74%-84.1%; p < 0.01). DA PT is not related to any adverse events (p>0.05). |
/ | Lower costs for radiological examinations in DA PT (5.1%-13.6%; p = NR)/(4.00 vs. 7.43; p < 0.01). Significantly fewer medication prescribed in DA PT (32.2%-48% vs. 44.1%-84%; p < 0.01). Significantly less PT visits in DA PT (5.9-20.2 vs. 7.0-33.6; p < 0.01). Decreased cost in DA (£9.55-$14.83 vs. £47.94-$63.65; p < 0.01). Mean number of days of work missed was significantly less in DA PT (10.4 vs. 27.9 days: p = NR). |
| Piscitelli et al (2018) (18) | No significant difference between GP referral and DA PT in terms of pain reduction (64.6% vs. 66.6%; p = 0.76). DA PT has better clinical outcomes in terms of function and health-related QoL (self-reported questionnaires: 2.4 ± 2.8 vs. 4.1 ± 4.6; p = 0.03). DA PT is not related to any adverse events (p>0.05). |
DA PT provides greater treatment compliance (76%-79% vs. 58%-69%; p = 0.004). | DA PT reduces waiting time and improves accessibility of PT (5-6 vs. 9-69 days; p < 0.001). DA PT leads to less medical imaging ($44 ± 190 vs. $175 ± 541; p < 0.01)/(47 vs. 242 patients; p < 0.001). DA PT leads to less prescribed medication ($36-163 vs. $78-873; p < 0.01)/(62-79 vs. 219-276 patients; p < 0.001). |
| Demont et al (2021) (19) | No significant difference between DA and physician-led usual medical care for pain but tendencies to positive effects (p≥0.05). Better clinical outcomes for function in DA PT (RMQ function score 4.1 in GP referral vs. 2.4 in DA PT; p = 0.03). No significant difference in QoL, but tendencies to positive effects (p≥0.05). Significantly higher satisfaction levels in DA compared to physician-led usual medical care (74.7% vs. 53.2%; p = 0.002). DA PT is not related to any adverse events (p>0.05). |
Significantly higher treatment compliance in DA (76%-79% vs. 58%-69%; p = 0.004). | Significantly shorter waiting time with DA PT (4-5 vs. 9-31 days; p < 0.001). Significantly less X-ray imaging described in DA PT (7.3% vs. 13.6%; p < 0.001). Significantly less medication prescribed in DA PT (32.2% vs. 44.1%; p < 0.01). Fewer or the same number of PT visits in DA PT (two to three fewer sessions; p = 0.001). Significant fewer patients required a primary care physician visit in DA (54% vs. 71%; p = 0.0113). Average cost saving per episode is significantly lower in DA PT (average saving = £36.42/patient/episode of care; p = 0.016)/(average costs £66.31 vs. £89.99; p < 0.05). |
| Babatunde et al (2020) (17) | No significant differences between patient characteristics in DA/self-referral vs. medical triage (p≥0.05) regarding age and gender. No significant differences in pain, functional outcomes, and QoL for patients who assessed MSK care via DA compared to GP-led care. No reports of adverse effects or missed red flags. |
Less work-related absence and sick leave in DA PT. 10%-20% less total cost for DA PT compared to GP-led care. >65% less prescribed analgesics and NSAID. >70% less radiology. 2%-10% lower follow-up consults. |
|
| Gallotti et al (2023) (21) | Better management accuracy, less waiting time, and equal to higher QoL. | Higher rate of presence; shorter time to discharge (+6%). | Higher cost-effectiveness (€−441.9 per episode of care) Imaging −28%; medication −41.2%; referral −20.7% Less sick leave (5% less prescriptions, −37 less sick leave days prescribed) |
DA = direct access; GP = general practitioner; MSK = musculoskeletal; NSAID = nonsteroidal anti-inflammatory care; PT = physiotherapy; QoL = quality of life; RMQ = Roland-Morris questionnaire; VAS = visual analogue scale.
Primary studies
Four primary studies, subsequent to the randomized controlled trial (RCT) conducted by Gallotti et al (21), contribute pertinent and insightful information to this scoping. Among these, one is a pilot RCT and three are retrospective cohort studies, which are elucidated further in the subsequent section.
Reddington et al (22) conducted a pilot RCT, employing qualitative analysis to examine patient expectations and experiences concerning accelerated access to physiotherapy. They engaged participants diagnosed with sciatica (n = 33) in individual interviews (n = 46) recruited from 14 National Health Service (NHS) primary care general practices and a physiotherapy service provider in the UK. Their findings indicate that expedited access to physiotherapy holds merit in terms of perceived recovery enhancement and/or mitigation of further physical and psychological decline. Negative patient expectations of physiotherapy predominantly stemmed from prior experiences of unfruitful physiotherapy. Based on their overarching study outcomes, the authors advocate for an individualized patient-centric approach alongside expedited access to physiotherapy for sciatica patients.
Crowell et al (23) conducted a retrospective cohort study to assess adherence to the low back pain Healthcare Effectiveness Data and Information Set (HEDIS) within the United States Military Health System Data Repository. They compared military personnel suffering from acute back pain regarding interventions administered in a DA physical therapy clinic vs. a general primary care clinic. Results indicate that in the physical therapy clinic, 96.7% of encounters did not entail imaging orders within the initial 28 days of symptom onset, compared to 82.0% in the primary care clinic (p < 0.001). The authors conclude that PTs operating in a DA setting are notably more inclined than primary care providers to adhere to low back pain imaging guidelines, particularly in young, athletic patients.
Wood et al (24) conducted another retrospective cohort study comprising a substantial qualitative analysis based on patient free-text reports concerning experiences with first contact physiotherapists (FCP) for MSK issues. Of the participants (n = 498), 73% reported being “extremely likely” to recommend the FCP service to friends and family, while 22% reported “likely” to recommend it. Conversely, only 1% would not recommend the service. Most respondents highlighted the communication skills of the FCP, emphasizing the importance of clear and understandable information provision. Additionally, respondents valued a diagnosis and treatment plan, as well as consultation with knowledgeable specialists. Self-management skills and shared decision-making were also perceived as valuable components. A small proportion of respondents reported unresolved conditions or dissatisfaction due to delays in treatment. Respondents appreciated being treated with respect and empathy, often comparing FCP consultations favourably to those with GPs.
The study by Halfpap et al (25) aimed to evaluate health care utilization and associated outcomes for Active Duty Service Members (ADSM) receiving services at an acute spine pain clinic (ASPC) during its initial 5 years of operation at a large military treatment facility in the United States. The most common chief complaint among 1,215 ADSM patients was acute lumbar spine pain (73%), followed by cervical spine pain (15%), with thoracic spine pain representing the fewest cases (12%). On average, patients attended 3.5 physical therapy visits (range 1-13), with the majority (61.1%) utilizing three or fewer visits. A review of medical records for 100 randomly selected patients within 12 months of their initial evaluation indicated reduced medication use, imaging, and referrals to surgical services. The authors concluded that the DA physiotherapy approach demonstrates potential benefits in terms of rapid access to treatment and education for patients with acute spine pain, facilitated by PTs in military treatment facilities.
In summary, it can be stated that the studies of Reddington et al (22) and Wood et al (24) indicate that from a patient’s perspective, several advantages are experienced especially regarding perceived recovery enhancement and high communication and information skills of PTs as well as the shared decision-making and self-management approach. However, also a small number of negative experiences are reported related to delayed referral for further treatment in case of unresolved conditions.
From a more societal perspective, the study from Crowell et al (23) indicates a better adherence to actual treatment guidelines in case of DA physiotherapy and resulting reduced medication use, imaging, and referrals to surgical services according to Halfpap et al (25).
Table 4 provides a summary of the individual studies presenting information such as the study and country, design and aim of the study, study setting, population and sample size, intervention, and outcome measures.
| Individual studies | ||||
|---|---|---|---|---|
| Study and country | Design, aim of the study | Study setting, population, sample size | Intervention | Outcome measures |
Crowell et al (2022) (23) United States |
Retrospective data analysis cohort study | To compare rates of compliance with the National Committee for Quality Assurance – Healthcare Effectiveness Data and Information Set (HEDIS) recommendations for diagnostic imaging in low back pain between physical therapists and primary care providers in young, athletic patients | Analysis of 1,845 Military Health System Data Repository (MDR) data | In the physical therapy clinic, 96.7% of encounters did not have imaging ordered within the first 28 days of onset of symptoms, compared with 82.0% in the primary care clinic (p < 0.001). |
Halfpap et al (2022) (25) United States |
Retrospective trial on low back pain in military | To compare DA PT in (acute) low back pain to random retrospective sample | 1,215 patients compared to 100 randomly selected patients’ medical records | Medication: 26% in PT vs 20% in non-PT and 47.4%-72% in the ED Radiographs: 7% in PT vs. 28% in non-PT vs. 26.1 in the ED Complex Imaging: 1% in PT vs. 12% in non-PT vs. 8.2% in the ED |
Reddington et al (2022) (22) UK |
Descriptive nested qualitative study via semi-structured patient interview | To explore sciatica patients’ experiences with DA | 80 patients with sciatica | This study suggests that accelerated access to physiotherapy has value in terms of aiding perceived recovery and/or halting further physical and psychological decline |
Wood et al (2022) (24) UK |
Online survey | Patient-reported experience and outcomes for DA | 680 reported questionnaires and 785 free-text responses | Approximately 70% of participants reported no need for consulting other health care professionals |
DA = direct access; ED = emergency department; PT = physiotherapy.
Discussion
The purpose of this scoping review was to analyse the impact of DA on the quality of MSK primary physiotherapy care from the perspectives of the patient, the provider, and society. No differences were found for pain reduction, QoL, functioning, and well-being although some systematic reviews indicated a tendency in favour of DA physiotherapy. Higher treatment compliance and a more accurate decision-making were found concerning the providers’ perspective and, finally, differences in favour of DA were found for waiting time, prescribed medication, and medical imaging. Less work-related absence and a clear reduction in health care costs were reported in some studies. Although some of the included reviews had a high risk of bias, their findings are in full agreement with the recent low-bias review of Babatunde et al (17).
Proponents of the DA system argue many advantages of this system. For patients, the most important advantage is that the physiotherapist becomes much more accessible, and patients lose less valuable time in the diagnostic process (26). Other advantages were expected to be found in terms of QoL, functioning, and patient satisfaction. From a clinical aspect, DA physiotherapy performs at least as well as physiotherapy by referral. However, all primary studies had relatively short follow-up of about 1 month, and the added benefits of DA may not be captured in the absence of a long-term follow-up.
For physiotherapists, an advantage could be found in the prestige of their profession and the greater responsibility involving an interesting challenge for physiotherapists in the functional evaluation of the patient (9,10). Moreover, several other health professions, such as chiropractors and osteopaths, are directly accessible, while their training courses are less focused on the diagnosis and screening of red and yellow flags (8). Red flags may indicate the presence of a serious underlying cause explaining the current symptoms. However, this must be put in perspective, as the evidential value for red flags has proved insufficient to state that they are excellent predictors of serious underlying disorders (12). Yellow flags identify underlying patient characteristics that could potentially lead to a slower recovery process or ending up in chronicity. It is very important to identify the presence of yellow flags to avoid non-response to the treatment of patients (27).
Furthermore, DA physiotherapy could be a step forward in the physiotherapists’ autonomy and development as a diagnostician. However, it should not become compulsory as some physiotherapists may not consider themselves competent or do not support it. In addition, it would be useful for older physiotherapists who did not follow the most modern training, especially in clinical reasoning and diagnosis, to be given further training in the field of diagnosis. However, no information emerged from this review regarding the responsibility, liability, status, prestige, and job satisfaction of the physiotherapists.
Evidence suggests greater treatment compliance of patients and fewer missed appointments in a DA physiotherapy setting, allowing the physiotherapist to spend their time optimally (21). Some diagnoses made by a GP do not provide added value in the clinical reasoning of the rehabilitation plan. Some diagnoses made by a GP are actually superfluous, as the pattern of symptoms may not have a clear pathophysiological foundation (28,29). The best example of this is the well-known non-specific low back pain phenomenon. In many cases, no underlying pathophysiological mechanism can be found. Treatment by the physiotherapist is then based on the pattern of symptoms and not on the prescribed medical diagnosis (29). Some studies (13) reported that the decision-making ability of physiotherapists is great, but they do not consistently recognize the need for immediate referral. Physiotherapists with MSK specialization were more likely to make correct decisions for patients with MSK conditions and critical medical conditions (13). But overall, the reported results may indicate that training might have to be adapted for this purpose.
Consensus on the benefits of the society perspective has not been found in all areas. DA physiotherapy can decrease the workload and pressure of GPs because a large number of patients with MSK disorders proceed directly to a physiotherapist. In this way, GPs have more time to focus on their other patients. It can also lead to less waiting time, less medical imaging, and fewer prescription and use of medication (17-21). Some studies (17, 19-21) reported less work-related absence and sick leave in DA physiotherapy but others did not find a consensus for the return-to-work rate (18). And, in general, there is evidence of an important cost reduction in health care for MSK disorders (18-21).
As a final argument in favour of DA physiotherapy, it can be noticed that there is no reporting of countries in which DA physiotherapy has been introduced where it was subsequently rejected. This shows that the advantages at least counterbalance, but presumably overweigh the possible disadvantages (30).
Limitations of this scoping review
The information gathering was restricted to English, Dutch, and French and two different databases (MEDLINE and Web of Science), possibly causing some relevant articles to be missed. A specific additional search in the PEDro database for systematic reviews did not reveal any additional publications.
Recommendations for future research
Different types of studies, preferably high-quality RCTs, should be conducted, focusing on various perspectives that remain unanswered or unclear. Economic evaluations could be performed from the societal perspective, and several options exist for designing studies from both the patients’ and therapists’ perspectives.
Conclusions
This scoping review suggests that DA physiotherapy can offer multiple advantages over GP referral physiotherapy. Although no significant effects were found for pain and QoL, strong evidence from one unbiased study, and supported by some lower quality evidence, indicates that DA does not result in a significant decrease in functional outcome. As such DA physiotherapy seems to be as beneficial to the patient as physiotherapy by referral. Moreover, evidence indicates that it does reduce the use of medical imaging and leads to less prescription and use of medication, resulting in costs. The small significant differences in favour of DA physiotherapy from the patients’ perspective, combined with no loss in terms of pain reduction, suggest at least an equal level of care quality. Moreover, it seems that DA physiotherapy does not have any adverse effects on patients. This, coupled with predominantly positive benefits from DA physiotherapy from a societal perspective, suggests that the advantages of DA physiotherapy are more situated in the societal domain.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ contributions: All authors actively participated in the preparation of this manuscript. EC: data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing original draft, writing review and editing. JVdB: data curation, formal analysis, investigation, supervision writing original draft. RP and AT: data curation, formal analysis, writing original draft. AS: formal analysis, validation. EVT: conceptualization, methodology, supervision, writing review and editing.
Data availability statement: Additional material may be requested directly from the responsible author. The information generated and analysed during the current study are publicly available by means of the mentioned search engines and publications in the reference list
References
- 1. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197-2223. CrossRef PubMed
- 2. Vos T, Barber RM, Bell B, et al; Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743-800. CrossRef PubMed
- 3. Davenport TE, Sebelski CA. The physical therapist as a diagnostician: how do we, should we, and could we use information about pathology in our practice? Phys Ther. 2011;91(11):1694-1695. CrossRef PubMed
- 4. Williams CM, Maher CG, Hancock MJ, et al. Low back pain and best practice care: a survey of general practice physicians. Arch Intern Med. 2010;170(3):271-277. CrossRef PubMed
- 5. Foster NE, Hartvigsen J, Croft PR. Taking responsibility for the early assessment and treatment of patients with musculoskeletal pain: a review and critical analysis. Arthritis Res Ther. 2012;14(1):205. CrossRef PubMed
- 6. World Physiotherapy. Country profiles reveal global state of the physical therapy profession 2019. Online. Accessed January 2024.
- 7. Bürge E, Monnin D, Berchtold A, Allet L. Cost-effectiveness of physical therapy only and of usual care for various health conditions: systematic review. Phys Ther. 2016;96(6):774-786. CrossRef PubMed
- 8. Mitchell JM, de Lissovoy G. A comparison of resource use and cost in direct access versus physician referral episodes of physical therapy. Phys Ther. 1997;77(1):10-18. CrossRef PubMed
- 9. American Physical Therapy Association (APTA). Vision Statement for the Physical Therapy Profession. 2022. Online. Accessed January 2024.
- 10. Leemrijse CJ, Swinkels ICS, Veenhof C. Direct access to physical therapy in the Netherlands: results from the first year in community-based physical therapy. Phys Ther. 2008;88(8):936-946. CrossRef PubMed
- 11. Bishop A, Ogollah RO, Jowett S, et al; STEMS study team. STEMS pilot trial: a pilot cluster randomised controlled trial to investigate the addition of patient direct access to physiotherapy to usual GP-led primary care for adults with musculoskeletal pain. BMJ Open. 2017;7(3):e012987. CrossRef PubMed
- 12. Galliker G, Scherer DE, Trippolini MA, Rasmussen-Barr E, LoMartire R, Wertli MM. Low back pain in the emergency department: prevalence of serious spinal pathologies and diagnostic accuracy of red flags. Am J Med. 2020;133(1):60-72.e14. CrossRef PubMed
- 13. Jette DU, Ardleigh K, Chandler K, McShea L. Decision-making ability of physical therapists: physical therapy intervention or medical referral. Phys Ther. 2006;86(12):1619-1629. CrossRef PubMed
- 14. Brooks G, Dripchak S, Vanbeveren P, Allaben S. Is a prescriptive or an open referral related to physical therapy outcomes in patients with lumbar spine-related problems? J Orthop Sports Phys Ther. 2008;38(3):109-115. CrossRef PubMed
- 15. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. CrossRef PubMed
- 16. Whiting P, Savović J, Higgins JPT, et al; ROBIS group. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225-234. CrossRef PubMed
- 17. Babatunde OO, Bishop A, Cottrell E, et al. A systematic review and evidence synthesis of non-medical triage, self-referral and direct access services for patients with musculoskeletal pain. PLoS One. 2020;15(7):e0235364. CrossRef PubMed
- 18. Piscitelli D, Furmanek MP, Meroni R, De Caro W, Pellicciari L. Direct access in physical therapy: a systematic review. Clin Ter. 2018;169(5):e249-e260. PubMed
- 19. Demont A, Bourmaud A, Kechichian A, Desmeules F. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: a systematic review of the literature. Disabil Rehabil. 2021;43(12):1637-1648. CrossRef PubMed
- 20. Ojha HA, Snyder RS, Davenport TE. Direct access compared with referred physical therapy episodes of care: a systematic review. Phys Ther. 2014;94(1):14-30. CrossRef PubMed
- 21. Gallotti M, Campagnola B, Cocchieri A, Mourad F, Heick JD, Maselli F. Effectiveness and consequences of direct access in physiotherapy: a systematic review. J Clin Med. 2023;12(18):5832. CrossRef PubMed
- 22. Reddington M, Baxter S, Walters SJ, Cole A. Patients’ expectations and experiences of accelerated access to physiotherapy for sciatica: qualitative findings from a mixed-methods study. Physiotherapy. 2022;115:102-110. CrossRef PubMed
- 23. Crowell MS, Mason JS, McGinniss JH. Musculoskeletal imaging for low back pain in direct access physical therapy compared to primary care: an observational study. Int J Sports Phys Ther. 2022;17(2):237-246. CrossRef PubMed
- 24. Wood L, Bishop A, Goodwin R, Stynes S. Patient satisfaction with the first contact physiotherapy service: results from the national evaluation survey. Musculoskeletal Care. 2022;20(2):363-370. CrossRef PubMed
- 25. Halfpap J, Riebel L, Tognoni A, Coller M, Sheu RG, Rosenthal MD. Improving access and decreasing healthcare utilization for patients with acute spine pain: five-year results of a direct access clinic. Mil Med. 2022 Mar 12:usac064. CrossRef PubMed
- 26. GOV-UK. Our health, our care, our say: a new direction for community services. 2006. Online. Accessed January 2024.
- 27. Stewart J, Kempenaar L, Lauchlan D. Rethinking yellow flags. Man Ther. 2011;16(2):196-198. CrossRef PubMed
- 28. Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343-350. PubMed
- 29. Pinnington MA, Miller J, Stanley I. An evaluation of prompt access to physiotherapy in the management of low back pain in primary care. Fam Pract. 2004;21(4):372-380. CrossRef PubMed
- 30. Deyle GD. Direct access physical therapy and diagnostic responsibility: the risk-to-benefit ratio. J Orthop Sports Phys Ther. 2006;36(9):632-634. CrossRef PubMed