 |
Arch Physioter 2024; 14: 47-55 ISSN 2057-0082 | DOI: 10.33393/aop.2024.3015 ORIGINAL RESEARCH ARTICLE |
 |
Defining the glenohumeral range of motion required for overhead shoulder mobility: an observational study
ABSTRACT
Background: Recovery of overhead mobility after shoulder surgery is time-consuming and important for patient satisfaction. Overhead stretching and mobilization of the scapulothoracic and glenohumeral (GH) joints are common treatment interventions. The isolated GH range of motion (ROM) of flexion, abduction, and external rotation required to move above 120° of global shoulder flexion in the clinical setting remains unclear. This study clarified the GH ROM needed for overhead mobility.
Methods: The timely development of shoulder ROM in patients after shoulder surgery was analyzed. Passive global shoulder flexion, GH flexion, abduction, and external rotation ROM were measured using goniometry and visually at 2-week intervals starting 6-week postsurgery until the end of treatment. Receiver operating characteristic curves were used to identify the GH ROM cutoff values allowing overhead mobility.
Results: A total of 21 patients (mean age 49 years; 76% men) after rotator cuff repair (71%), Latarjet shoulder stabilization (19%), and arthroscopic biceps tenotomy (10%) were included. The ROM cutoff value that accurately allowed overhead mobility was 83° for GH flexion and abduction with the area under the curve (AUC) ranging from 0.90 to 0.93 (p < 0.001). The cutoff value for GH external rotation was 53% of the amount of movement on the opposite side (AUC 0.87, p < 0.001).
Conclusions: Global shoulder flexion above 120° needs almost full GH flexion and abduction to be executable. External rotation ROM seems less important as long as it reaches over 53% of the opposite side.
Keywords: Glenohumeral, Postoperative, Range of motion, Rehabilitation, Shoulder, Stiffness
Received: December 22, 2023
Accepted: July 18, 2024
Published online: August 26, 2024
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What’s already known about this topic?
- Overhead shoulder mobility after shoulder surgery is an important treatment goal, but it requires time and a global shoulder flexion angle of over 120°. The exact relationship between global shoulder flexion and GH ROM remains unclear.
What does the study add?
- An observation of ROM development in patients after shoulder surgery provides the GH ROM cutoff values for global shoulder flexion above 120°. GH ROM measurements can be used to predict overhead shoulder mobility.
Background
Arm elevation is a crucial function of the shoulder girdle. Restricted shoulder elevation impairs many daily and athletic activities, such as reaching overhead. Overhead movement requires global shoulder flexion angles over 120° (1,2). After shoulder surgery, mobility can be restricted due to different underlying mechanisms (3). Restoring arm elevation is an important goal for all shoulder treatments and plays an important role in subsequent patient satisfaction (4). Common treatments include mobilizing and stretching the shoulder into passive end range elevation (5,6). However, these treatment approaches often cause severe pain (7,8). Therefore, understanding shoulder biomechanics and the relationship between its components is necessary to treat shoulders with motion loss (9).
Global shoulder flexion is defined as the motion of the humerus relative to the thorax in the sagittal plane of approximately 160° (1). It is a combined motion of the scapulothoracic and glenohumeral (GH) joints. The normal function of the shoulder complex is a coordinated motion sequence of all joint elements. Impairment in one joint directly affects the whole kinematic chain (10,11). Loss of GH range of motion (ROM) alters the entire kinematics of motion. The scapular upward rotation occurs earlier during arm elevation as a compensatory strategy for limited GH ROM (11,12). The scapula pulls the clavicle into an early final retraction position close to the neck muscles. Once the final position of the scapula and clavicle is achieved, only the thoracic spine can move to gain more elevation motion (13). The abnormal movement pattern of the scapula and clavicle often continues for a longer time, even after GH mobility has restored considerably (7,11).
Improving arm elevation by optimizing the scapulothoracic substitution is important in managing restricted shoulder ROM (12,13). However, excessive compensatory movements could cause secondary problems in other joints (14). Mobilizing and stretching the shoulder into further global flexion results in greater rotation of the scapula at the acromioclavicular joint. This may induce compression of the soft tissues between the coracoid process and the clavicle, which can again lead to pain (7). Further, subacromial structures can be irritated when the arm is pushed into elevation (8). In other words, GH loss of motion can result in mechanically related shoulder pain.
Thus, sufficient GH ROM is mandatory for overhead mobility as it decreases the requirement for the scapulothoracic substitution and allows the scapula and clavicle to move around the thorax (7). An impairment-based rehabilitation approach should therefore focus on improving GH ROM (15). In particular, increasing external rotation (ER) ROM has been recommended to improve global shoulder flexion (8,14,16,17).
From a biomechanical perspective, the amount of GH ER in full global shoulder flexion is controversially discussed in the literature (18-23). However, with regard to postoperative patient satisfaction, ER, if not massively impaired, has no major influence on overall patient satisfaction (24).
The amount of GH flexion, abduction, and ER mobility required to perform an overhead arm movement in patients with restricted shoulder ROM remains unclear. However, knowledge of the relationship of GH mobility and global shoulder flexion is important to guide the rehabilitation process.
Therefore, this study aimed to investigate the passive GH cutoff value for overhead mobility (global shoulder flexion above 120°). Based on preliminary data, we hypothesized that nearly full GH flexion and abduction is required for overhead mobility, whereas GH ER is negligible.
Methods
Study design and setting
A retrospective observational study was conducted in a group of patients after a variety of shoulder surgery. Data of patients who underwent postoperative physical therapy at the Balgrist University Hospital outpatient Physiotherapy Department, Zurich, Switzerland, were collected and analyzed. All patients provided written informed consent for the anonymized use of their medical data for scientific purposes before data collection. The retrospective data analysis was approved by the ethics committee of the Canton of Zurich (BASEC 2016 01120).
The following data from the patient reports were used for analysis: (a) ROM measurements of the unaffected and operated sides recorded 6 weeks after the surgery; (b) follow-up ROM measurements of the operated side at intervals of approximately 2 weeks. Demographic and baseline characteristics of the patients were recorded at the start of the treatment.
Participants
A total of 34 patients referred for treatment after arthroscopic rotator cuff repair, open shoulder stabilization with Latarjet procedure, arthroscopic biceps tenotomy and of a minimum age of 18 years were initially selected; 21 patients met the inclusion criteria and were included in the data analysis. The sample size for this study was determined a priori, based on similar studies in the literature, which typically included 20 to 30 subjects, ensuring sufficient statistical power (15,17,25).
Exclusion criteria were as follows: an unhealthy shoulder on the opposite side, prior shoulder fracture, scoliosis, and documented symptoms of complex regional pain syndrome. For the analysis, only the patients treated by physiotherapists who had experience in treating shoulder conditions for more than 10 years and who had seen more than five patients during the recruiting period were included.
All patients were treated once or twice a week with individual sessions and hydrotherapy in groups, each session lasting 30 minutes. The interventions were (a) instruction and progression of home exercises to increase shoulder ROM and rotator cuff and scapular muscle strength; (b) cognitive behavioral strategies, including goal setting, education, and positive reinforcement; (c) passive GH and scapulothoracic joint mobilization in supine or side position without pain provocation; (d) active joint movement in water of 34°C and swimming as soon as allowed; and (e) soft tissue massage. Treatment procedures after shoulder surgery were based on the patient’s condition and followed the standardized guidelines of the surgeon.
ROM measurement
The ROM measurement procedure used in the Physiotherapy Department is a combination of the method originally described by Winkel et al (26) and Cyriax (27), and, to some extent, our own clinical experience. The method was evaluated for its reproducibility. Reliability was excellent across all movement directions (intraclass correlation coefficient [ICC], 0.91-0.99). The standard error of measurement ranged from 2° to 5°, and the smallest detectable change ranged from 5° to 14° (unpublished data). All physiotherapists of the institution participated in a training session to standardize their shoulder ROM measurements for quality reasons. The shoulder ROM measurements and notations were part of the daily routine and were performed before the regular physiotherapy session.
For shoulder ROM measurements, all movements were performed passively until the end range position. Passive end range position was determined by the tactile perception of a clear resistance to further motion against the stabilizing hand (28). All passive movements were measured either with a standard 205 × 45-mm, double-armed 360° goniometer constructed of clear plastic or by visual estimation. All measurements were conducted with an accuracy of 5°, as this corresponds to the clinical standard.
Global shoulder flexion
For global shoulder flexion, the patients stood with their eyes fixed forward. The examiner moved the patient’s arm with one hand in the sagittal plane with the elbow in full extension and the thumb pointing up to the maximal end range position. The other hand rested on the scapula and thorax to secure upright posture. The patient was then asked to hold the elevated arm in position with his other hand while the examiner measured the angle using a goniometer. Anatomical landmarks and measurement device positioning followed the recommendations of Norkin and White (28). The stationary arm of the goniometer was placed parallel to the midline of the thorax, and the moving arm was aligned with the shaft of the humerus and lateral epicondyle (Fig. 1A).

FIGURE 1 - Joint measurement: (a) passive global shoulder flexion measured with goniometer; (b) passive glenohumeral (GH) flexion; (c) passive GH abduction; and (d) passive external rotation. All GH movements were measured visually.
GH motion
For GH motion measurement, the patients were sitting upright on a chair with their feet on the floor. GH flexion was performed in the sagittal plane. The arm was passively moved with one hand, while the other hand immobilized the lower angle of the scapula with the thumb. The angle was measured visually when the scapula began to rotate. The landmarks used for global shoulder flexion were also used here (Fig. 1B).
GH abduction was performed in the plane of the scapula approximately 30° anterior to the frontal plane. One hand was placed on the acromion for stabilization and the other hand moved the arm until the scapula began to move. The landmarks for visual estimation were the sagittal plane and the shaft of the humerus (Fig. 1C).
GH ER was taken by passively placing the patient’s arm at 0° of GH abduction with the elbow flexed at 90° with one hand. The medial border of the scapula was stabilized with the fingers of the other hand while the arm was moved in ER. The angle was measured visually from the sagittal plane and the forearm using the olecranon process and ulnar styloid for reference (Fig. 1D).
Statistical analysis
To describe the sample, data are expressed using descriptive statistics. Mean ROM of the healthy side at the start of evaluation was used as a reference for the percentage calculation. Mean ROM value of the operated arm at baseline and at the end of evaluation were computed. Data are presented separately for the dominant and nondominant sides.
Overhead movement was defined as a global shoulder flexion above 120° and was coded as a dichotomous variable (positive/negative results). To evaluate which GH ROM can be used as a predictor of overhead movement, a receiver operating characteristic (ROC) curve was computed. ROC curves were constructed by plotting sensitivity versus 1-specificity for the absolute data and the percentage data of the opposite side as independent variables. The area under the curve (AUC) was calculated to quantify the accuracy of the predictor. The AUCs can range from 0.50 (no accuracy in distinguishing overheads from nonoverheads) and 1.00 (perfect accuracy). An AUC of 0.75 has been proposed to be clinically useful (29). Significance level was set at p < 0.05. The optimal threshold value for each GH movement was determined by selecting the cutoff value closest to 80% specificity. Sensitivity at fixed point of specificity is suitable for determining the validity of a predictor and for comparing two diagnostic tests (30). In addition to the calculation, the measurements were graphically illustrated to exemplify the relationship between GH ROM and overhead mobility.
All statistical analyses were performed under the supervision of an experienced biostatistician using Statistical Package for the Social Sciences (SPSS) version 23.0 (IBM SPSS Statistics Inc., Chicago, IL, USA).
Results
A total of 34 patients were screened for inclusion. Of these, 21 patients with a total of 127 complete documentation measurements met the inclusion criteria and were analyzed. Reasons for exclusion were as follows: patients treated by therapists with less than five patients during the analyzing period (10), unhealthy shoulder on the opposite side (2), and documented symptoms of complex regional pain syndrome (1). Finally, patients of only two physiotherapists fulfilled the selection criteria. Demographic characteristics of the included patients are summarized in Table 1.
Descriptive data of the measured ROM value at the start and end of evaluation are presented in Table 2. Dominant and nondominant sides presented similar ROM values. Patients exhibited a larger standard deviation (SD) in the ROM on the healthy side for GH AR compared to GH flexion and GH abduction. All cases showed some loss of motion at the start of the evaluation and an improvement in ROM at the end of the evaluation.
The results of the ROC curve analysis are shown in Figure 2. From the 127 measurements, 70 were classified as overhead and 57 as nonoverhead. The absolute and percentage data of all GH movements showed good performance in distinguishing overhead mobility with AUCs ranging from 0.80 to 0.93, which were significant (p < 0.001).
The cutoff values of the shoulder ROM are presented in Table 3. The cutoff values closest to 80% specificity, along with their corresponding sensitivity and AUC with 95% confidence interval (CI), are presented separately based on degrees and as a percentage relative to the ROM of the opposite side. The 95% CI of the AUCs exhibit a relatively narrow range of 0.08 to 0.16, confirming the predictor’s test strength. GH ER exhibits lower sensitivity compared to GH flexion and GH abduction. This is supported by their respective AUC values.
| Characteristic | Summary | |
|---|---|---|
| Female/male | 5/16 | |
| Mean age, years (SD) | 49.1 (15.7) | |
| Mean body height, cm (SD) | 174.4 (8.3) | |
| Mean body mass, kg (SD) | 81.5 (14.2) | |
| Dominant hand: left/right | 0/21 | |
| Side of surgery: left/right | 10/11 | |
| Surgery (number) | ||
| Rotator cuff repair | 15 | |
| Latarjet shoulder stabilization | 4 | |
| Arthroscopic biceps tenotomy | 2 | |
| Mean evaluation duration, days | ||
| Rotator cuff repair | 92.0 | |
| Latarjet shoulder stabilization | 69.0 | |
| Arthroscopic biceps tenotomy | 93.5 | |
| Total measurement points | 127 | |
| Rotator cuff repair | 94 | |
| Latarjet shoulder stabilization | 21 | |
| Arthroscopic biceps tenotomy | 12 | |
SD = standard deviation.
In addition to the calculation, the measurements were graphically illustrated to exemplify the relationship between GH ROM and the ability to move overhead (Fig. 3). The pattern for GH flexion and GH abduction differs from that of GH ER. The graph illustrates that some patients were able to achieve overhead movement with less than 20° and 20% GH ER, respectively.
Discussion
The goal of this observational study was to evaluate the required GH ROM to achieve overhead mobility in patients after shoulder surgery. Our results showed that overhead mobility can be expected with a GH ROM of 83° for flexion and abduction each and with 53% ER of the contralateral side. In other words, consistent with our hypothesis, overhead mobility needs nearly full ROM for GH flexion and abduction, whereas ER ROM seems less important.
An understanding of normal shoulder ROM is crucial to interpret the results of this investigation. Normative data vary considerably in the literature as many factors can influence ROM. These factors include age, gender, sports activity, and the position of the subject during the examination. Arm dominance is another factor that can influence shoulder ROM (31-33). To minimize the abovementioned variability, the healthy side of the participants was used as a reference. In the present study the mean shoulder ROM for GH flexion was 93° (SD ± 4°), for GH abduction 93° (SD ± 5°), and for GH ER 43° (SD ± 17°) on the dominant side (Tab. 2). Due to the wide range of GH ER, the relationship between the affected and healthy sides was used for interpretation.
| Shoulder | Global flexion | GH flexion | GH abduction | GH exorotation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At start of evaluation | ||||||||||||
| Healthy side dominant | ||||||||||||
| Mean/% | 154°/100% | 93°/100% | 93°/100% | 43°/100% | ||||||||
| (SD/range) | (5/150-165) | (4/85-100) | (5/90-105) | (17/5-60) | ||||||||
| Healthy side nondominant | ||||||||||||
| Mean/% | 155°/100% | 96°/100% | 93°/100% | 47°/100% | ||||||||
| (SD/range) | (7/140-165) | (5/90-100) | (5/85-100) | (13/15-75) | ||||||||
| Operated side dominant | ||||||||||||
| Mean/%* | 111°/72% | 73°/78% | 69°/74% | 15°/35% | ||||||||
| (SD/range) | (23/70-145) | (13/50-90) | (12/50-90) | (15/0-35) | ||||||||
| Operated side nondominant | ||||||||||||
| Mean/%* | 109°/70% | 65°/68% | 62°/67% | −1°/0% | ||||||||
| (SD/range) | (24/80-140) | (18/35-90) | (18/35-85) | (7/−20-5) | ||||||||
| At end of evaluation | ||||||||||||
| Operated side dominant | ||||||||||||
| Mean/%* | 137°/89% | 90°/97% | 87°/94% | 38°/88% | ||||||||
| (SD/range) | (17/110-135) | (9/70-100) | (7/70-95) | (19/0-60) | ||||||||
| Operated side nondominant | ||||||||||||
| Mean/%* | 143°/92% | 90°/94% | 87°/94% | 28°/60% | ||||||||
| (SD/range) | (18/100-160) | (8/70-100) | (11/55-95) | (18/0-50) | ||||||||
Operated on the dominant side, n = 11, nondominant side, n = 10; total, n = 21.
GH = glenohumeral; SD = standard deviation.
*Percent of range of motion of the healthy side.
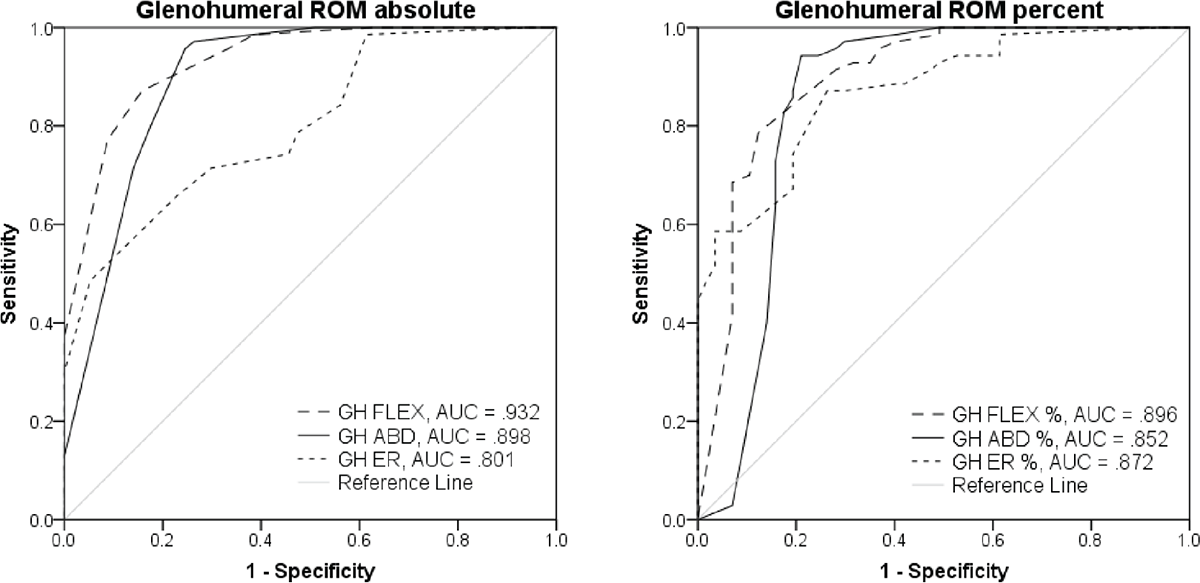
FIGURE 2 - Receiver operating characteristic curves for glenohumeral ROM. It was constructed with the data points of ROM absolute and ROM percentage of the opposite side by plotting sensitivity versus 1-specificity. The greater the area under the curves, the greater was the ability of the predictor to distinguish between overhead mobility (>120° global flexion) and nonoverhead mobility. ABD = abduction; AUC = area under the curve; ER = external rotation; FLEX = flexion; GH = glenohumeral; ROM = range of motion.
To the best of our knowledge, this is the first study to investigate the GH cutoff value for overhead shoulder mobility in patients recovering from a shoulder surgery. A comparative analysis of our data with other studies is difficult due to several methodological differences. Previous studies of shoulder kinematics in patients with loss of motion have predominantly described active rather than passive motion (11,12,14,15,34). Both conditions are important to understand the state of the joint, but passive ROM measurements are more useful to obtain the maximal achievable motion. In addition, passive motion assessments allow clinicians to estimate the amount of isolated GH motion (31). Another factor that affects the results when GH mobility is studied is the type of device used to measure shoulder ROM (35). In clinical practices, shoulder ROM is usually measured with goniometry or visually (36). The accuracy of visual estimation and goniometry varies highly in the current literature (36). However, Warth and Millett (33) have reported that experienced clinicians can measure shoulder ROM with an acceptable precision.
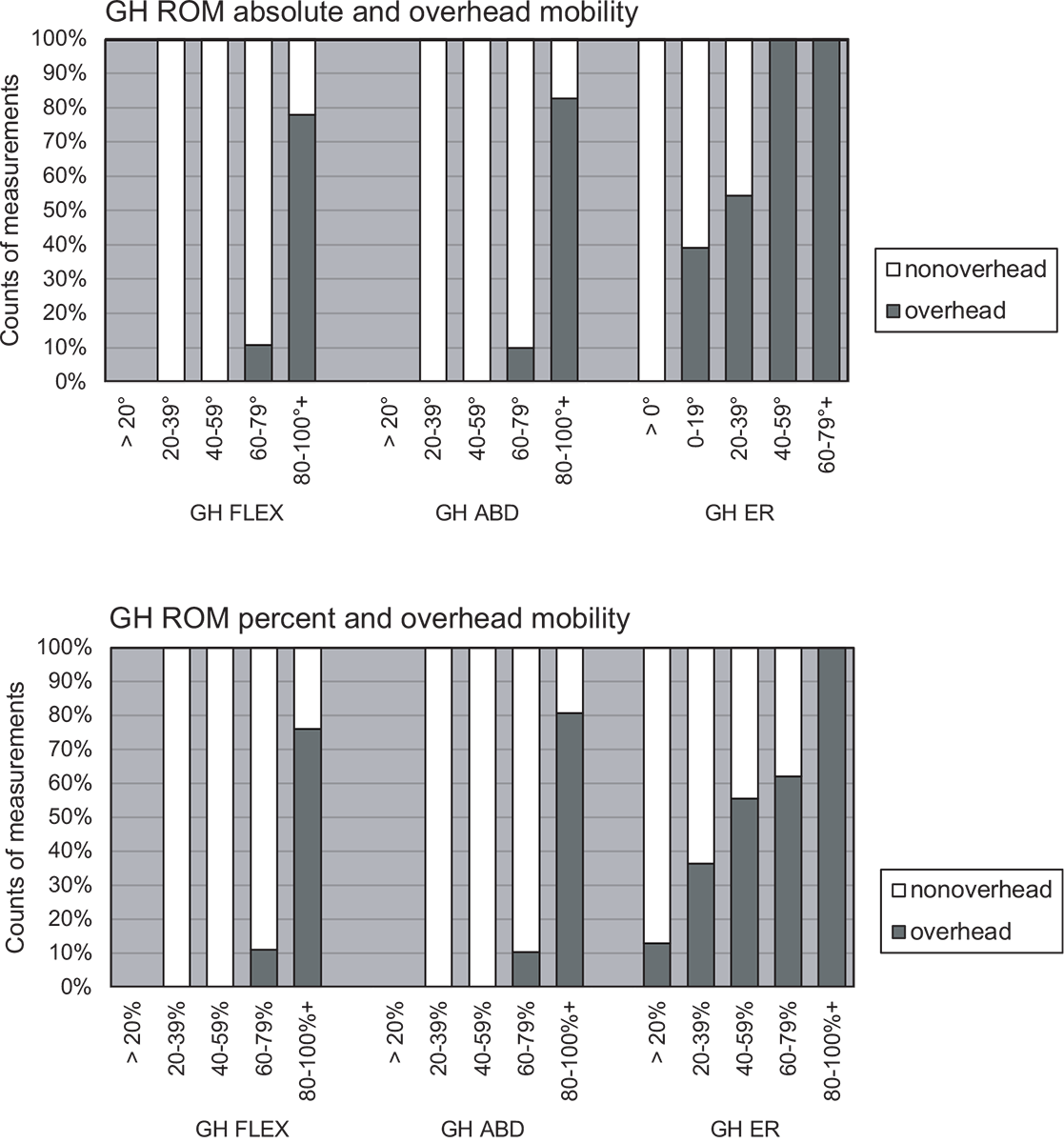
FIGURE 3 - Relationship between the glenohumeral range of motion improvement and the overhead mobility (>120° global flexion). The column chart displays all measurements (n = 127), divided into white (nonoverhead; n = 57) and gray (overhead; n = 70), along with the corresponding glenohumeral range of motion. Glenohumeral movements are demonstrated in absolute values and in percentage of the opposite side values. GH FLEX = glenohumeral flexion; GH ABD = glenohumeral abduction; GH ER = glenohumeral external rotation; GH ROM = glenohumeral range of motion.
| Predictor | 80% specificity cutoff value | Sensitivity (%) | AUC | 95% CI | |
|---|---|---|---|---|---|
| GH ROM absolute | |||||
| FLEX | 83° | 87 | 0.93 | 0.89-0.97 | |
| ABD | 83° | 80 | 0.90 | 0.83-0.95 | |
| ER | 28° | 66 | 0.80 | 0.72-0.87 | |
| GH ROM percent | |||||
| FLEX | 87% | 90 | 0.90 | 0.83-0.95 | |
| ABD | 85% | 87 | 0.85 | 0.77-0.93 | |
| ER | 53% | 74 | 0.87 | 0.81-0.93 | |
The ROM cutoff values closest to 80% specificity are presented both as absolute values in degrees and as a percentage relative to the opposite side. The corresponding sensitivity at the identified cutoff point is displayed, providing insight into the test’s ability to correctly identify true positives at this level of specificity. Along with the AUC and 95% CI, this provides a comprehensive view of the diagnostic performance at the specified specificity level.
ABD = abduction; AUC = area under the curve; CI = confidence interval; ER = external rotation; FLEX = flexion; GH ROM = glenohumeral range of motion.
Thus, a direct comparison of our findings with those of previous studies was not possible due to the aforementioned reasons. Nevertheless, consistent with our data, Stenvers (7) reported similar GH ROM values for global shoulder flexion. The author used X-ray cinematography to study the development of global shoulder flexion in subjects with frozen shoulder. Passive shoulder motion in supine position was used for the investigation. The results showed that almost 90° of GH flexion and abduction was necessary before the shoulder could move over a so-called 90° mechanism. This 90° mechanism was used as an umbrella term for the abnormal motion kinematics of the frozen shoulder and is comparable with the nonoverhead mobility of the present investigation. In a study by Baettig et al (37) patient satisfaction after rotator cuff repair was analyzed. They found active abduction ROM was the only shoulder movement that significantly correlated with higher patient satisfaction in a multivariate analysis. It is known that GH stiffness generates greater impairments in global abduction movements as it does for global flexion movements due to the reduced compensating ability of the scapulothoracic joint in the abduction plane (7). This supports the findings of the present study and indicates that GH mobility plays a key role in shoulder function.
Interestingly, the results demonstrated that some patients could move overhead with considerably restricted GH ER, whereas only a few patients could move overhead with less than 80° of GH flexion and abduction (Fig. 3). A possible explanation was found in a basic study that investigated the effect of selective capsular shortening on passive GH ROM (38). The shortening of the superior part of the capsule resulted in limited GH ER of the adducted arm, whereas GH abduction was not restricted (38). According to Crétual et al (39), GH ER mobility in adduction is least correlated with global shoulder mobility and should therefore be done with the shoulder in abduction. Nevertheless, ER with the arm at the side is commonly used to monitor the development of mobility in patients with restricted shoulder ROM. It has the advantage of being assessed independently of abduction ability, which is often restricted after shoulder surgery (39).
Thus, a question arises about the amount of ER necessary for full global shoulder flexion. However, this topic is controversially discussed in the literature (18,20,21,23). In this context, McClure et al (35) mentioned the importance of scapular upward rotation in full arm elevation for a healthy shoulder. They speculated that scapular upward rotation reduces GH ER requirement. This may be an explanation why some patients were able to move overhead with considerably restricted ER values.
Several limitations should be considered when interpreting the results of our study. First, the data were based on clinical assessments with visual estimation and goniometry, which are not the gold standards for research due to the lack of desired accuracy. Second, when interpreting ROM in clinical practice, the measurement of all ROM directions is important. It provides the information which parts of the capsule are responsible for the specific restrictions (3,38). The present investigation did not evaluate GH internal rotation ROM. The internal rotation in adduction with the hand behind back maneuver is a motion of different joints that requires GH, scapulothoracic, elbow, wrist, and finger movements (40). It is therefore recommended to measure isolated GH internal rotation with the arm abducted. However, internal rotation cannot be measured as recommended in patients with restricted GH abduction. Finally, the present study group consisted of 21 patients who had undergone different shoulder surgery. This nonhomogeneous group may have different impairments. Nevertheless, the mobility of the GH joint is significantly influenced by its biomechanical properties, such as ROM and the surrounding musculoskeletal structures, rather than solely by surgical procedures. The relatively small sample size of 21 patients is consistent with similar studies in the field (15,17,25). Additionally, the AUCs demonstrated a narrow range within the 95% confidence interval (CI), indicating a high level of validity of the results despite the limited sample size.
The main clinical implication of the findings of this study is that the assessment of GH ROM is important for predicting global shoulder flexion mobility. The results imply that nearly normal GH flexion and abduction ROM is required before the shoulder can move above 120° global shoulder flexion. Therefore, a rehabilitation approach that focuses on GH mobility improvement rather than on global shoulder flexion is recommended. The results of this investigation showed a tendency toward greater importance of GH flexion and abduction values than for GH ER, which needs to be confirmed by future research.
Conclusion
This study documents the cutoff values for GH flexion, abduction, and ER ROM that can accurately predict overhead mobility. Results showed that 83° of GH flexion and abduction was required before patients could move their arms above 120° of global shoulder flexion. This means nearly full GH ROM in flexion and abduction is required before overhead mobility is achievable. Consequently, overhead stretches in the presence of GH stiffness should be performed with caution. The cutoff value for GH ER in degrees was inaccurate for interpretation due to the wide range of GH ER of the healthy opposite shoulders. Therefore, it is suggested to use the percent value. About 53% of the ROM of the opposite side for GH ER was required for overhead mobility.
Acknowledgments
The authors thank Marcel Enzler for the technical help and general support and Prof. Dr. Burkhardt Seifert for helping with the statistical analysis. Clinical Trial registration: BASEC 2016 01120, retrospectively registered.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ contributions: LD and JS were responsible for the design of the study. LD conducted the final analysis and wrote the manuscript. LD and SB provided significant contributions to data analysis. JS and HS mentored LD to interpret the data and provided critical feedback for manuscript. All authors read and approved the final manuscript.
Data availability: The data presented in this study are available on request from the corresponding author.
Ethics approval and consent to participate: This study was approved by the ethics committee of the Canton of Zurich (BASEC 2016 01120). All participants provided written informed consent for the anonymized use of their medical data for scientific purposes.
Consent for publication: The authors affirm that participants provided informed consent to publish the obtained data in this study.
References
- 1. Magermans DJ, Chadwick EK, Veeger HE, van der Helm FC. Requirements for upper extremity motions during activities of daily living. Clin Biomech (Bristol, Avon). 2005;20(6):591-599. CrossRef PubMed
- 2. Namdari S, Yagnik G, Ebaugh DD, et al. Defining functional shoulder range of motion for activities of daily living. J Shoulder Elbow Surg. 2012 Sep;21(9):1177-83. CrossRef. Epub 2011 Nov 1. PubMed.
- 3. Warner JJ, Greis PE. The treatment of stiffness of the shoulder after repair of the rotator cuff. J Bone Joint Surg. 1997; 79(8):1260-1269. CrossRef
- 4. O’Holleran JD, Kocher MS, Horan MP, Briggs KK, Hawkins RJ. Determinants of patient satisfaction with outcome after rotator cuff surgery. J Bone Joint Surg Am. 2005;87(1):121-126. CrossRef PubMed
- 5. Vermeulen HM, Obermann WR, Burger BJ, Kok GJ, Rozing PM, van Den Ende CH. End-range mobilization techniques in adhesive capsulitis of the shoulder joint: a multiple-subject case report. Phys Ther. 2000;80(12):1204-1213. CrossRef PubMed
- 6. Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am. 2000;82(10):1398-1407. CrossRef PubMed
- 7. Stenvers JD. Primary frozen shoulder: a retrospective study on treatment with physiotherapy [Doctoral dissertation]: University of Groningen 1994.
- 8. Donatelli R, Ruivo RM, Thurner M, Ibrahim MI. New concepts in restoring shoulder elevation in a stiff and painful shoulder patient. Phys Ther Sport. 2014;15(1):3-14. CrossRef PubMed
- 9. Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91(2):378-389. CrossRef PubMed
- 10. Fayad F, Hoffmann G, Hanneton S, et al. 3-D scapular kinematics during arm elevation: effect of motion velocity. Clin Biomech (Bristol, Avon). 2006;21(9):932-941. CrossRef PubMed
- 11. Vermeulen HM, Stokdijk M, Eilers PH, Meskers CG, Rozing PM, Vliet Vlieland TP. Measurement of three dimensional shoulder movement patterns with an electromagnetic tracking device in patients with a frozen shoulder. Ann Rheum Dis. 2002;61(2):115-120. CrossRef PubMed
- 12. Fayad F, Roby-Brami A, Yazbeck C, et al. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech. 2008;41(2):326-332. CrossRef PubMed
- 13. Stenvers JD, van Woerden HH. The primary frozen shoulder [CD-ROM]. Nederland: Onderwijscentrum NSA; 2011.
- 14. Veeger HE, Magermans DJ, Nagels J, Chadwick EK, van der Helm FC. A kinematical analysis of the shoulder after arthroplasty during a hair combing task. Clin Biomech (Bristol, Avon). 2006;21(suppl 1):S39-S44. CrossRef PubMed
- 15. Rundquist PJ, Ludewig PM. Correlation of 3-dimensional shoulder kinematics to function in subjects with idiopathic loss of shoulder range of motion. Phys Ther. 2005;85(7):636-647. CrossRef PubMed
- 16. Magermans DJ, Smits NC, Chadwick EK, Veeger D, van der Helm FC, Rozing PM. Discriminating factors for functional outcome after shoulder arthroplasty. A critical review of the literature. Acta Orthop Belg. 2003;69(2):127-136. PubMed
- 17. Yang JL, Chang CW, Chen SY, Lin JJ. Shoulder kinematic features using arm elevation and rotation tests for classifying patients with frozen shoulder syndrome who respond to physical therapy. Man Ther. 2008;13(6):544-551. CrossRef PubMed
- 18. Itoi E, Hsu HC, An KN. Biomechanical investigation of the glenohumeral joint. J Shoulder Elbow Surg. 1996;5(5):407-424. CrossRef
- 19. Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90-104. CrossRef PubMed
- 20. Browne AO, Hoffmeyer P, Tanaka S, An KN, Morrey BF. Glenohumeral elevation studied in three dimensions. J Bone Joint Surg Br. 1990;72(5):843-845. CrossRef PubMed
- 21. Inui H, Nobuhara K. Glenohumeral relationship in maximum elevation. Surg Radiol Anat. 2014;36(8):755-761. CrossRef PubMed
- 22. Johnston T. The movements of the shoulder‐joint: a plea for the use of the ‘plane of the scapula’ as the plane of reference for movements occurring at the humero‐scapular joint. Br J Surg. 2005;25(98):252-260. CrossRef
- 23. Matsuki K, Matsuki KO, Yamaguchi S, et al. Dynamic in vivo glenohumeral kinematics during scapular plane abduction in healthy shoulders. J Orthop Sports Phys Ther. 2012;42(2):96-104. CrossRef PubMed
- 24. Baettig SJ, Wieser K, Gerber C. Determinants of patient satisfaction following reconstructive shoulder surgery. BMC Musculoskelet Disord. 2017;18(1):458. CrossRef PubMed
- 25. Ruiz Ibán MA, Alonso Güemes S, Ruiz Díaz R, Diaz Heredia J, de Rus Aznar I, Lorente Moreno R. Assessment of isolated glenohumeral range of motion in patients with adhesive capsulitis can help predict failure of conservative treatment: a pilot study. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2099-2104. CrossRef PubMed
- 26. Winkel D, Aufdemkampe G, Meijer O. Nonoperative Orthopedics and Manual Therapy, Part 2/1: Diagnosis of the Extremities. Gustav Fischer Verlag; 1994.
- 27. Cyriax J. Textbook of orthopaedic medicine. Diagnosis of soft tissue lesion. 8th ed. Bailliere Tindall; 1982:1.
- 28. Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. 4th ed. FA Davis Company; 2009.
- 29. Fan J, Upadhye S, Worster A. Understanding receiver operating characteristic (ROC) curves. CJEM. 2006;8(1):19-20. CrossRef PubMed
- 30. Kumar R, Indrayan A. Receiver operating characteristic (ROC) curve for medical researchers. Indian Pediatr. 2011;48(4):277-287. CrossRef PubMed
- 31. Clarke GR, Willis LA, Fish WW, Nichols PJ. Preliminary studies in measuring range of motion in normal and painful stiff shoulders. Rheumatol Rehabil. 1975;14(1):39-46. CrossRef PubMed
- 32. Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61(5):756-759. CrossRef PubMed
- 33. Warth RJ, Millett PJ. Physical examination of the shoulder. 1 ed. New York: Springer; 2015: VII, 276 p.
- 34. Triffitt PD. The relationship between motion of the shoulder and the stated ability to perform activities of daily living. J Bone Joint Surg Am. 1998;80(1):41-46. CrossRef PubMed
- 35. McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001 May-Jun;10(3):269-77. CrossRef. PubMed.
- 36. Hanney WJ, Kolber MJ, Marshall JS. The reliability of clinical measurements designed to quantify shoulder mobility. Phys Ther Rev. 2011;16(6):413-422. CrossRef
- 37. Baettig SJ, Wieser K, Gerber C. Determinants of patient satisfaction following reconstructive shoulder surgery. BMC Musculoskelet Disord. 2017 Nov 15;18(1):458. CrossRef. PubMed
- 38. Gerber C, Werner CM, Macy JC, Jacob HA, Nyffeler RW. Effect of selective capsulorrhaphy on the passive range of motion of the glenohumeral joint. J Bone Joint Surg Am. 2003;85(1):48-55. CrossRef PubMed
- 39. Crétual A, Bonan I, Ropars M. Development of a novel index of shoulder’s mobility based on the configuration space volume and its link to mono-axial amplitudes. Man Ther. 2015;20(3):433-439. CrossRef PubMed
- 40. Mallon WJ, Herring CL, Sallay PI, Moorman CT III, Crim JR. Use of vertebral levels to measure presumed internal rotation at the shoulder: a radiographic analysis. J Shoulder Elbow Surg. 1996;5(4):299-306. CrossRef PubMed