 |
Arch Physioter 2024; 14: 70-79 ISSN 2057-0082 | DOI: 10.33393/aop.2024.2733 ORIGINAL RESEARCH ARTICLE |
 |
Neurological conditions and community-based physical activity: physical therapists’ belief and actions
ABSTRACT
Introduction: Physical therapists (PTs) are key actors in physical activity (PA) promotion. However, it remains unclear whether PTs in community settings promote community-based PA such as adapted physical activity (APA) and adaptive sports (AS) to their patients with neurological conditions (NCs). The main purposes were to evaluate the beliefs PTs have of APA and AS, and to explore actions they undertake to promote it to their patients with NCs.
Methods: An online survey was created specifically for the study. PT associations and institutions were contacted and licensed PTs working in community-based settings, treating at least one patient with a NC, were invited to participate. Questionnaires were analyzed only if all mandatory questions had been answered.
Results: A total of 165 questionnaires were analyzed. PTs reported prioritizing active treatment. They viewed APA and AS as beneficial for their patients with NCs; however, its promotion remained largely infrequent due to a number of barriers. The PTs’ own level of PA seemed to significantly influence their beliefs of the benefits of APA and AS (p = 0.001), while being specialized in neurologic physical therapy enabled the PTs to increase frequency of promotion (p = 0.003).
Conclusion: Though community-based PTs are aware of the importance of PA for individuals with NCs, they face difficulties in promoting it to their patients. However, these difficulties are reduced among PTs who are specialized in neurologic physical therapy. Efforts should be made toward educating PTs to neurological pathologies and their specificities when it comes to PA.
Keywords: Health promotion, Neurological rehabilitation, Physical activity, Physical therapists
Received: November 23, 2023
Accepted: September 5, 2024
Published online: September 30, 2024
This article includes supplementary material
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What’s already known about this topic:
• Adapted physical activity, including adaptive sports, is very beneficial for individuals with disabilities due to neurological conditions. Health care professionals, especially physical therapists, are well placed to vehicle such messages and should promote such activities.
What does the study add:
• Physical therapists do not frequently promote adapted physical activity and adaptive sports to their patients with neurological conditions. Lack of knowledge limits their actions. Such barriers are reduced when specializing in neurologic physical therapy.
Introduction
Though it was long believed that physical activity (PA) was detrimental for people presenting with neurological conditions (NCs) such as stroke, multiple sclerosis (MS), Parkinson’s disease (PD), spinal cord injury (SCI), or others (1), sound evidence now clearly demonstrates the beneficial effects of PA on different NCs (2,3), enabling a paradigm shift (4). The literature suggests PA reduces the risk of developing secondary complications (5) and improves autonomy in everyday life (6-10). Finally, in some progressive NCs such as PD or MS, PA may decelerate neurodeterioration (11,12). PA should therefore be a vital part of neurorehabilitation, as recommended by a wide range of condition-specific clinical guidelines (13-16).
Despite this, a majority of individuals with disability due to NCs do not engage in sufficient PA. Indeed, studies suggest that, in the United States, up to 80% of this population are physically inactive (17,18). This finding has been echoed in other parts of the world, as authors repeatedly report low level of PA and highly sedentary lifestyles among individuals with NCs (19-22). A drop in PA level is especially great after rehabilitation, when people with NCs return to their communities (23). This lack of compliance to long-term PA may be overcome by making the activity more enjoyable and social. In that sense adapted physical activity (APA) and adaptive sports (AS) allow for PA to be performed in group settings, while under supervision of a trained coach or therapist.
However, individuals with NCs often report lack of knowledge on how, and where, to engage in such PA in the community (24,25). Health care professionals (HCPs) therefore play a vital role in educating their patients toward leading a more active lifestyle (26). In that regard, physical therapists (PTs), defined as exercise experts by the “World Confederation for Physical Therapy,” are especially important (27). Moreover, during rehabilitation, individuals with NCs will spend more time with their PT than with any other HCP, making PTs a key reference (28).
While most PTs acknowledge their responsibility in PA promotion among individuals with NCs, implementation in real-life settings remains challenging (27). A qualitative study found that although English PTs believed PA to be important, efforts to promote it to their patients with SCI were lacking (29). However, this study focused specifically on PTs working within SCI-specific rehabilitation centers. Yet, people with NCs do not always have the opportunity to attend highly specialized centers on a long-term basis. Furthermore, PTs who work in community-based settings may encounter ever more difficulty in promoting PA to such patients. It is therefore important to investigate how these PTs use PA, and promote APA and AS among their patients with NCs, within nonspecialized, community settings.
Therefore, the aims of the present study are (i) to explore the perceptions of benefits of APA and AS for individuals with NCs among PTs working within community settings; (ii) to assess if PTs utilize PA in their therapy, and (iii) to explore actions undertaken by the PTs to promote APA and AS as well as barriers to such actions. The secondary objective is to identify PT-related factors influencing PA beliefs and actions. Our hypothesis is that PTs perceive APA and AS as beneficial, but only few utilize PA as a therapeutic tool. Additionally, we except that the majority do not actively promote these activities to their patients with NCs.
Methods
This cross-sectional study was a web-based survey, directed toward French-speaking PTs in Belgium. The study was constructed and written according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines, as well as the “Checklist for Reporting Results of Internet E-surveys” guidelines (30). The completed checklist can be found in the Supplementary material I: CHERRIES. Ethical clearance was granted by the Ethics Committee of the Catholic University of Louvain. Participants remained anonymous, and gave their informed consent. Data were treated according to the General Data Protection Regulation.
Convenience sampling was used and participants were invited to respond to the online survey from November 2020 to April 2021. Participation was voluntary.
Eligible participants had to be (i) licensed PTs, (ii) practicing in Brussels or Wallonia (Belgium), (iii) practicing at least partly in a community setting, and (iv) French speakers. Moreover, (v) participants had to be treating at least one patient with a NC when answering the survey. PTs were excluded if their practice setting was solely based in hospitals, clinics, or rehabilitation centers, or if they were retired.
Sample size calculations were performed according to the total number of PTs practicing in Brussels and Wallonia. According to the latest Belgian report, this equaled 12,053 in 2016 (31). As response rates for online surveys approximate 30% (32), and using a margin error of 5% with a confidence level of 90%, the recommended sample size was 225 (33).
An online, adaptive, open questionnaire was created specifically for the study using “Limesurvey.” This platform performs IP checks to disable duplicate responses and ensures secure data protection through the Catholic University of Louvain.
Brainstorms among three researchers (one PT and two physicians), with knowledge of the literature available on the topic, were conducted and led to the creation of an initial version of the questionnaire. General guidelines for creating web-based surveys were followed (34): the majority of the questions were mandatory, it was not possible to return to previous questions once answered, questions were mainly closed-ended in order to decrease participation time (35), an adaptive structure was used (i.e., answers to one question determined following questions), and demographic-related questions were placed at the end of the survey (34). A progression bar was added so participants could estimate time to survey completion. Majority of the answers were on a 4-point Likert scale going from 0 (never/not at all) to 3 (always/very).
This first version was critically reviewed by three PTs with experience in neurorehabilitation, and modifications were made. The second version was then tested by another five PTs, who were naïve to the previous version. Their comments allowed final modifications to be made. The questionnaire’s final version included 26 questions, with an estimated completion time of 12 minutes. An English version can be found in the Supplementary material II: questionnaire used for the survey (translated from French to English).
Different communication channels were used simultaneously. First, a short message pertaining to our survey’s objectives and length, and containing the URL link toward the questionnaire, was published on different Belgian PTs Facebook groups. Second, local and national PT associations were contacted, by mail or phone, in order to diffuse survey link to their members. Third, the published repertoires “kinesithérapie.be” and “abterna.be” were used to contact PTs directly. Only PTs whose contacted details were published were contacted, preferably by phone (if their phone number was published) or by mail. Reminders were sent twice, with a 1-month interval.
Data were exported from Limesurvey into Excel in CSV format. Incomplete questionnaires (where a minimum one mandatory question was left unanswered) were removed from the analysis. Answers were summarized descriptively, by reporting the absolute and relative frequency.
A score was attributed to the PTs’ beliefs of benefits of APA and AS, and another for actions to promote APA and AS. This was done by summing the answers obtained on the Likert scales (i.e., “0: never/not important/not efficient” equaled 0, while “3: very frequently/very important/very efficient” equaled 3). For the total belief score, as this comprised the participants’ answers to four questions, maximal score was 12. Higher scores represented more positive beliefs. For the total action score, this related to five questions, with a maximal score of 15. Higher scores represented greater frequency of APA and AS promotion.
Statistical analyses were performed on both total belief and action scores using Statistical Package for the Social Sciences (SPSS; IBM, version 27). First, correlation between beliefs and actions scores was computed through Spearman’s test. The correlation coefficient was interpreted as negligible (0-0.10), low (0.11-0.39), moderate (0.40-0.69), strong (0.70-0.89), or very strong (0.90-1) (36). Second, to evaluate the influence of demographics on beliefs and actions, different tests were performed: Spearman’s correlations, to explore influence of the number of years PT treated patients with NCs; Kruskal-Wallis tests, first, to evaluate differences according to self-reported level of PA, and second, to explore differences according to percentage of patients with NCs within total patient population; and finally, Mann-Whitney tests, to evaluate differences according to presence of specific training in neurologic physical therapy. When differences were found, they were further analyzed by a chi-square test, to identify which questions led to the significant difference in scores between the groups. For all analyses, a p-value ≤ 0.05 was considered significant.
Results
A total of 255 individuals viewed the questionnaire’s introduction page, of which 224 advanced to the next section containing the questions related to eligibility; 33 individuals did not respect the inclusion criteria and were excluded. Of the remaining 191 PTs, 26 did not answer all mandatory questions. Therefore, 165 participants were included for analysis. The number of years practicing physical therapy with patients with NCs ranged from 0.08 (equivalent to 1 month) to 50, with a median of 7 years. While n = 19 participants self-reported low PA levels, the majority reported being moderately (n = 80) and highly (n = 61) physically active. No participant self-reported as not being physically active at all. Only 29% of the sample were specialized in neurologic physical therapy. Demographic parameters of the sample and their patient populations are displayed in Table 1.
| Variable | Categories | n (%) or median (1st; 3rd quartile) |
|---|---|---|
| Number of years practicing physical therapy with patients with NCs | 7 (3; 20) | |
| Specialized in neurologic physical therapy | -Yes
- No - No answer |
48 (29%)
109 (67%) 8 (4%) |
| Percentage of patients with NCs within overall patient population | - Less than 25%
- More than 25% but less than 50% - More than 50% but less than 75% - More than 75% but less than 100% - 100% |
104 (63%)
23 (14%) 11 (7%) 20 (12%) 7 (4%) |
| Type of NCs presented by patients* | - Stroke
- Parkinson’s disease - Multiple sclerosis - Peripheral nerve lesion - Neuromuscular disease - Traumatic brain injury - Spinal cord injury: paraplegia - Spinal cord injury: tetraplegia - Spina bifida - Others |
137 (83%)
111 (67%) 74 (45%) 61 (37%) 55 (34%) 44 (26%) 28 (16%) 20 (12%) 15 (9%) 16 (10%) |
| Disability level of patients presenting with NCs | - Majority (over 50%) present with severe disability
- Majority (over 50%) present with moderate disability - Majority (over 50%) present with mild disability - Disability level evenly spread among severe, moderate, and mild |
17 (9%)
53 (31%) 65 (38%) 30 (22%) |
| Self-reported PA level | -None
-Low -Moderate -High -No answer |
0
19 (11%) 80 (48%) 61 (37%) 5 (3%) |
NCs = neurological conditions; PA = physical activity.
*Note that multiple answers were possible. Therefore, some participants responded positively to a range of categories.
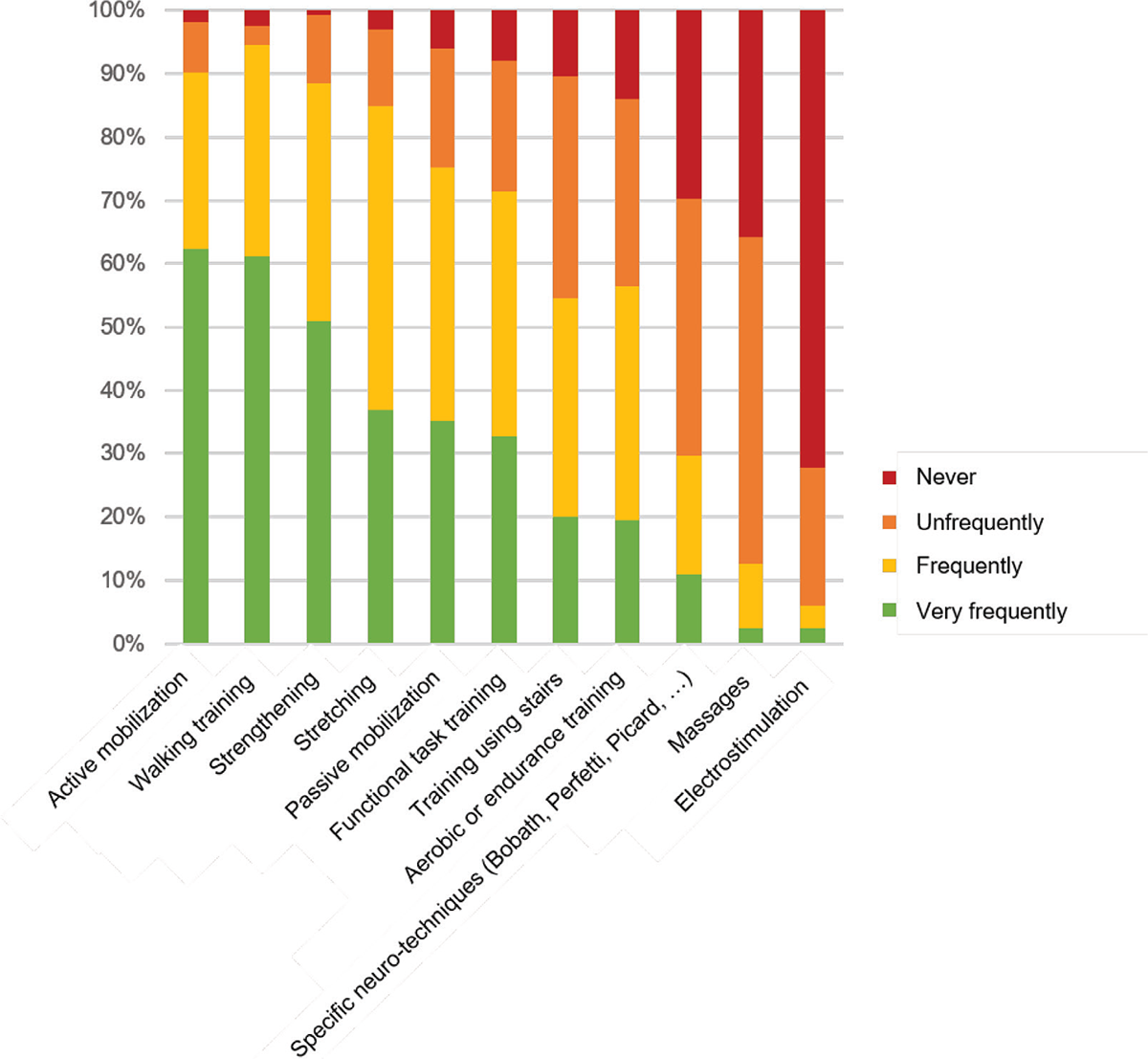
FIGURE 1 - Treatments used by the PTs during therapy. Bar graph demonstrating treatments used by all participants during sessions with patients with neurologic conditions.
Concerning general treatments performed with patients with NCs, the most common were: active mobilization, walking training, resistance training, and stretching. Endurance training was never or infrequently used by 14% and 30% of the sample, respectively. Massages and electrostimulation were the least common treatment options (Fig. 1).
The vast majority of PTs believed APA and AS to be important or very important for the physical and mental health of their patients with NCs. They also believed APA and AS to be effective at improving and maintaining motor function and autonomy (Tab. 2). Altogether, beliefs regarding the benefits of APA and AS were high among PTs, with a median score of 10 (Fig. 2).
| Items | Not effective/not important/never
(0) |
Slightly effective/slightly important/rarely
(1) |
Effective/important/frequently
(2) |
Very effective/very important/very frequently (3) |
|---|---|---|---|---|
| Belief 1: Effects of APA or AS on physical health | n = 3
2% |
n = 8
5% |
n = 60
36% |
n = 94
57% |
| Belief 2: Effects of APA or AS on mental health | n = 2
1% |
n = 7
4% |
n = 56
34% |
n = 100
61% |
| Belief 3: Effects of APA or AS on motor function | n = 4
2% |
n = 5
3% |
n = 74
45% |
n = 82
50% |
| Belief 4: Effects of APA or AS on autonomy | n = 4
2% |
n = 5
3% |
n = 87
53% |
n = 69
42% |
| Action 1: Discuss the subject of APA or AS with patient | n = 31
19% |
n = 53
32% |
n = 63
38% |
n = 18
11% |
| Action 2: Inquire into patient’s habits concerning APA or AS | n = 35
21% |
n = 54
33% |
n = 61
37% |
n = 15
9% |
| Action 3: Encourage patient to partake in APA or AS outside of physical therapy session | n = 30
18% |
n = 38
23% |
n = 66
40% |
n = 31
19% |
| Action 4: Guide patient with steps toward participating in APA or AS | n = 76
46% |
n = 63
38% |
n = 20
12% |
n = 6
4% |
| Action 5: Assess amount of PA undertaken by patient | n = 134
81% |
n = 13
8% |
n = 15
9% |
n = 3
2% |
APA = adapted physical activity; AS = adaptive sports; PA = physical therapist; PT = physical activity.
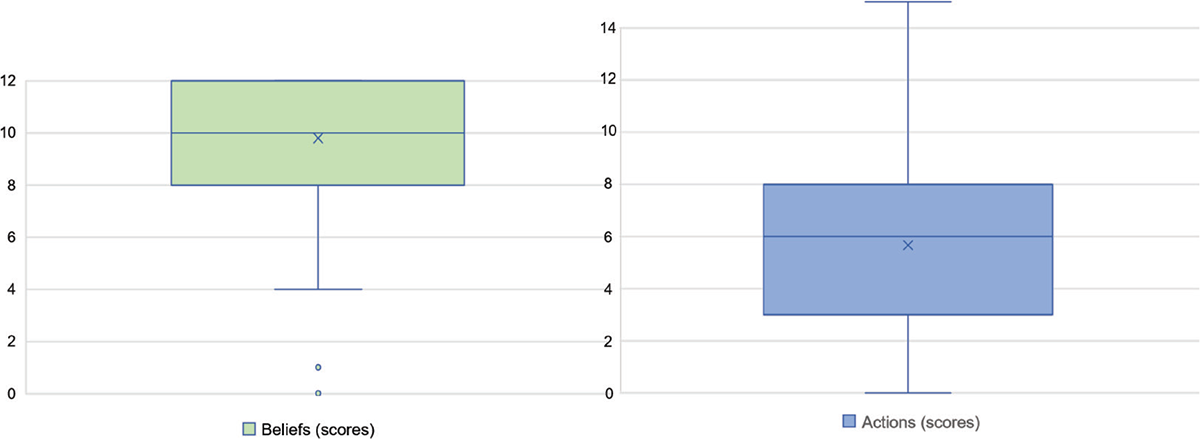
FIGURE 2 - Distribution of belief and action scores of the total sample. Boxplot demonstrating belief and action scores obtained by all participants. Belief scale ranged from 0 to 12, while action scale ranged from 0 to 15.
Concerning actions undertaken to promote APA and AS, half of the sample did not discuss the subject of APA and AS with their patients with NCs, and more than half did not inquire about their patients’ habits concerning APA and AS participation. Other actions to promote APA and AS, such as encouraging their patients with NCs to partake in such activities, or helping patients with NCs through the steps toward participating in APA or AS in community settings (including finding accessible sports clubs or centers), remained rare. Finally, 81% of the sample never assessed the amount of PA performed by their patients with NCs (Tab. 2). Accordingly, action scores of the sample were low, with a median of 5 (Fig. 2).
The most common barriers to undertaking actions toward APA or AS promotion are summarized in Table 3. While the most frequent barrier for PTs specialized in neurology was the lack of accessibility regarding information on APA and AS sessions, nonspecialized PTs reported being most limited by the lack of demand for such activities coming from their patients.
Statistical analyses demonstrated significant correlations of moderate intensity (r = 0.48, p = 0.001) between the PTs’ belief and action scores. Number of years practicing physical therapy with patients with NCs did not correlate with beliefs (r = 0.06, p=0.460) or actions (r = 0.098, p = 0.217). Likewise, the percentage of patients with NCs within total patient population did not influence both scores (beliefs p = 0.227, actions p = 0.138).
| Barriers | Yes, this is a barrier
(n, %) of total sample |
Yes, this is a barrier
(n, %) of sample with specific training in neurology |
Yes, this is a barrier
(n, %) of sample without training in neurology |
|---|---|---|---|
| Availability of time | 90
55% |
26
54% |
62
56% |
| Patient demand for such activities | 130
79% |
34
70% |
90
82% |
| Knowledge on APA and AS | 113
69% |
27
56% |
83
76% |
| Accessibility to information regarding APA and AS availability | 129
78% |
36
75% |
88
80% |
APA = adapted physical activity; AS = adaptive sports.
The presence of specific training within the neurology domain played a significant role on action scores (p = 0.003), whereby PTs with specific training in neurology undertook action to promote APA and AS more frequently than their colleagues (Fig. 3). Specifically, chi-square tests revealed that the actions undertaken significantly more frequently among PTs with training were inquiring into the patients’ habits concerning APA and AS (p = 0.040), guiding patients through the steps toward APA and AS sessions (p = 0.033), as well as assessing patients’ PA levels (p = 0.001). Training in neurology did not impact belief scores (p = 0.451). Conversely, while self-reported PA levels significantly influenced beliefs (p = 0.001) (Fig. 4), it had no impact on actions (p = 0.148). The highly and moderately active groups had significantly more positive beliefs related to the effects of APA and AS on their patients’ physical health (p = 0.010) and motor function (p = 0. 022), in comparison to the group that reported low PA levels.
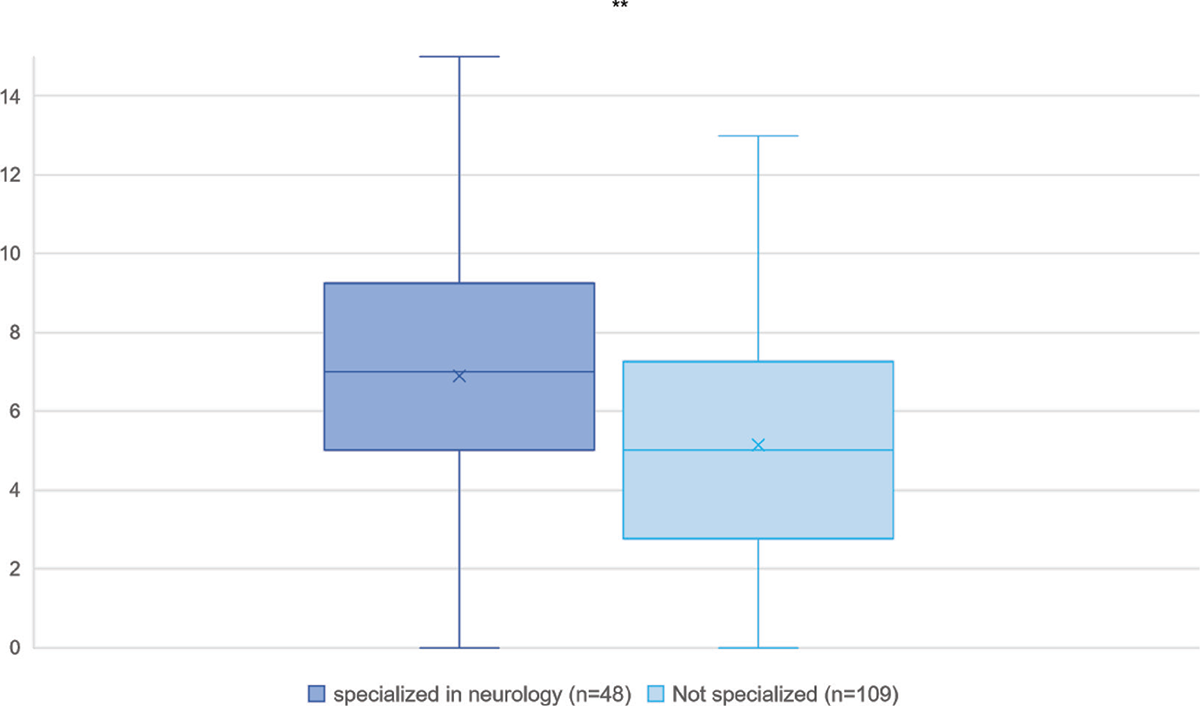
FIGURE 3 - Action scores obtained by physical therapists with and without specific specialization in neurology. Boxplot demonstrating the action scores obtained by the participants with and without specialization in neurologic physical therapy. **Significant difference where p-value is inferior to 0.01.
Discussion
The primary aims of this survey were to explore community-based PTs’ beliefs regarding APA and AS, and actions undertaken to promote these activities to individuals with NCs. The findings show that while the PTs believe APA and AS to be very beneficial for their patients with NCs, and commonly use active treatments in their therapy, they rarely undertake actions to promote APA and AS practice. Lack of demand from their patients, as well as lack of information on where APA and AS can be practiced, seem to be the two greatest barriers.
A large majority of the participating PTs had very positive beliefs regarding APA and AS, and favored active treatments to passive ones such as massage. This is in line with clinical guidelines stating the importance of PA in all stages of neurorehabilitation (37). A range of studies, performed among PTs in other various parts of the world, demonstrated similar positive attitudes toward PA, for all types of patients (29,38-41). Our findings further demonstrate that some demographic factors such as the number of years of practice with patients with NCs, specialization in neurologic physical therapy, as well as percentage of patients with NCs compared to total patient population do not influence beliefs. On the other hand, PTs who self-report as moderately or highly physically active view the effects of APA and AS more positively than PTs with low levels of PA. This seems to be related to APA and AS’ effects on physical health and motor capacity specifically. Similarly, Turkish PTs with greater levels of PA were more convinced of the benefits of PA for their patients, than their less active colleagues (42).
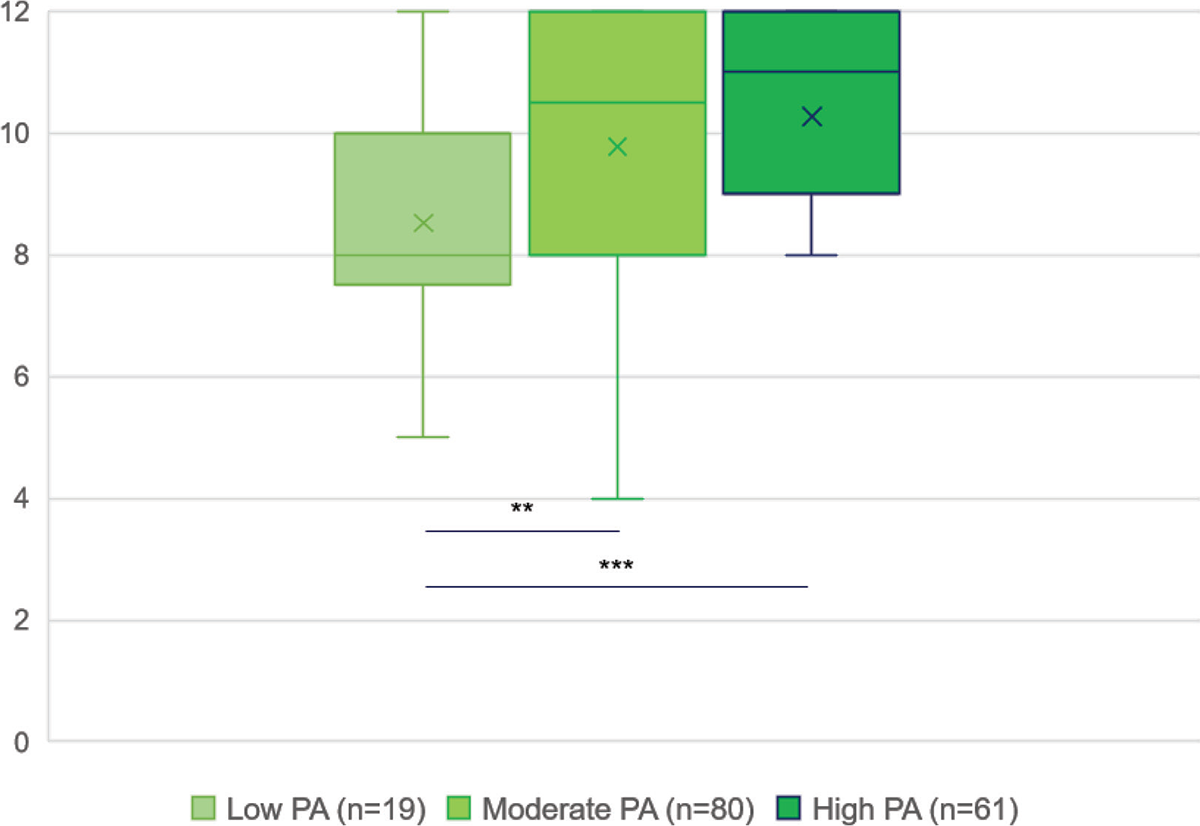
FIGURE 4 - Belief scores obtained by physical therapists reporting low, moderate, or high level of physical activity. Boxplot demonstrating belief scores obtained by the participants engaging in low, moderate, or high self-reported level of physical activity. **Significant difference where p-value is inferior to 0.01. ***Significant difference where p-value is 0.001.
However, actions undertaken to promote APA and AS remained infrequent. Only half of the PTs reported discussing APA or AS with their patients or inquiring into their PA habits, and little more than half encouraged their patients to engage in these activities. Moreover, the percentage of PTs who reported promoting APA or AS “very frequently” further dropped to less than 20%. This low percentage is in line with conclusions drawn by two qualitative studies within the field of neurological physical therapy. Indeed, authors of these studies, performed in England and Ireland (29), and New Zealand and Sweden (43), also observed that PA promotion remained predominantly absent from clinical practice. Conversely, Kennedy et al have found that 45% of their sample of 76 American PTs always promoted PA to patients with NCs (44). This difference, noted between Europe and New Zealand, and the United States, could be due to contextual factors such as PT education and reimbursement conditions. International collaborations could be set up in that regard, in order to learn from one another’s experience and benefit all parties involved.
The action that was found to be most lacking was guiding patients with NCs through the steps toward enrolling in an APA or AS in the community. Indeed, above 80% of our study’s total sample reported never, or only rarely, doing this. Yet, studies show that tailored PA counseling, taking into account the social and environmental conditions unique to each patient, is key in order to increase PA participation (45). To be effective, PA promotion needs to be frequent, repetitive, and include information on how and where to engage in such activities in the community. Educating patients with NCs on where to find this information themselves, as well as who to contact in order to enroll in APA or AS session in the community, is important as it empowers them and creates long-term changes (45).
Interestingly, our data uncovered that the frequency of APA and AS promotion-action was significantly greater following additional training in the field of neurologic physical therapy. Indeed, PTs with additional training in neurology reported undertaking more actions to promote APA or AS to patients with NCs, than their colleagues without training. This related to actions such as inquiring into their patients’ APA and AS habits, guiding patients through the steps needed to enroll in an APA or AS program in the community, and finally, monitoring or assessing their patients’ PA levels. All these actions allow PA promotion to be tailored according to the individual and his/her needs, and is vital for long-term participation (46). Therefore, efforts should be placed toward training more PTs in neurology, as it allows them to develop essential competencies that seem to be lacking from general PT training. This lack of training was observed by Eisele et al, who reported that German PTs, working in outpatient settings with all types of patients, believed they required greater competencies in order to promote exercise to patients who do not engage in PA (47).
Moreover, our findings suggest that PTs who are trained in neurology encounter less barriers to APA and AS promotion. Barriers such as accessibility to information on APA and AS availability in the community, as well as knowledge on APA and AS in general, were also less common among this group. Increased knowledge on APA and AS likely contributed to the increased actions undertaken by specialized PTs to promote such activities to their patients. Other authors have also reported on the important role of knowledge on increasing frequency of PA promotion among PTs (44,48). It is therefore of utmost importance that individuals with NCs who are discharged from rehabilitation settings be redirected to PTs in the community who are specialized in neurology. Indeed, these PTs have greater understanding of the special needs of this population, and therefore may provide them with more information on ways to be physically active.
The total sample’s greatest barrier to PA promotion seemed to be lack of demand from patients with NCs for such activities. German PTs also reported lack of patient interest for PA as the primary obstacle to exercise promotion for all types of patients (47). However, data suggest that the majority of patients with NCs, such as those with stroke, are interested in PA but lack education on the matter and therefore do not bring up the subject with HCPs (45,49). Moreover, certain tools, including behavior change techniques and education, have shown to be effective for those with low PA motivation (50).
In regard to accessibility to information on APA and AS availability in the community, ranked as the second and first barriers for PTs without and with specialization in neurology, similar results have been observed by Zhu et al. In their sample of 84 Australian PTs working in hospital settings, difficulty locating adequate PA opportunities in the community was cited as one of the most common barriers (51). Indeed, APA and AS still remain poorly developed when compared to sporting activities and opportunities for individuals without a disability (52). A solution could be to develop tools such as websites or applications that display this information in a user-friendly way, and that updates them regularly. Collaborating with patient organizations, which can provide greater insight into the specific needs of their members, should be encouraged when developing this. Such tools then need to be made visible among PTs in order to become engrained in everyday use with patients with NCs. Associations representing PTs at both a national and international level (such as “World Physiotherapy”) could be involved in making these tools visible.
Finally, time, or lack of it, seemed to be a barrier for half of the sample. While some authors reported time to be a significant, or even the most significant, barrier (38,53,54), others found only small proportions of the sample to be limited by time (42,55). However, as exercise is now recognized as a vital sign of health (56), it should gain priority in the treatment. This could be facilitated through education and implementation of specific guidelines on PA promotion in the physical therapy practice (29).
Certain study limitations should be considered. First, the sample size of 225 was not reached, though 255 PTs opened the survey. This may be due to our eligibility criteria. Indeed, the sample size calculation was based on the total number of PTs in Brussels and Wallonia, while our study only recruited PTs working in community settings with at least one patient with a NC. Thus, the sample number obtained may be representative of our specific population, though it is impossible to be certain as reports only state total number of PTs. Second, similarly to other self-completed questionnaires, social desirability may have skewed results concerning the frequency of actions undertaken to promote APA and AS. Moreover, participation was voluntary, so recruited PTs may have been highly interested in APA or AS. Yet, as one step of recruitment included contacting PTs one by one, and as the percentages of PTs answering “no” or “rarely” to some questions is high, the influence of these factors likely remained small.
Conclusions
Though PTs practicing in the community view APA and AS as very beneficial for their patients with NCs, and primarily use active therapies within the treatment they provide to these patients, promotion of APA and AS remains infrequent. Certain barriers, including lack of demand for such activities as well as difficulty in obtaining information on the availability of community-based APA and AS, still limit them. However, PTs who are specialized within neurologic physical therapy promote APA and AS more frequently, and report fewer barriers limiting their actions to do so. Effort toward educating more PTs to neurological physical therapy should therefore be made. Moreover, individuals with NCs should be directed to these types of PTs once they return to community settings. International collaborations should be encouraged, in order to inform best practices on PA promotion within individuals with NCs. Finally, tools, which centralize the information on availability of APA and AS sessions, should be created to facilitate visibility of these activities.
Acknowledgments
The work reported in the manuscript has been presented, through a 5-minute oral presentation, at the “XXIe Journées d’Etudes Francophones en Activité Physique Adaptée” in Nantes (France) in March 2023.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Authors’ contributions: LD played a role in conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, writing original draft, and writing review and editing. GS played a role in conceptualization, formal analysis, investigation, project administration, supervision, validation, writing original draft, and writing review and editing. JFK played a role in conceptualization, investigation, project administration, validation, and writing review and editing. MG and CG played a role in data curation, formal analysis, methodology, and writing original draft.
Data availability statement: The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the nature of the data.
Clinical Trial Protocol number: Not applicable to this survey.
References
- 1. Carr J, Shepherd R. The changing face of neurological rehabilitation. Braz J Phys Ther. 2006;10(2). CrossRef
- 2. Martin Ginis KA, van der Ploeg HP, Foster C, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet. 2021;398(10298):443-455. CrossRef PubMed
- 3. Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451-1462. CrossRef PubMed
- 4. Nadeau SE. A paradigm shift in neurorehabilitation. Lancet Neurol. 2002;1(2):126-130. CrossRef PubMed
- 5. Selph SS, Skelly AC, Wasson N, et al. Physical activity and the health of wheelchair users: a systematic review in multiple sclerosis, cerebral palsy, and spinal cord injury. Arch Phys Med Rehabil. 2021;102(12):2464-2481.e33. CrossRef PubMed
- 6. Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2020;3(3):CD003316. PubMed
- 7. Hayes S, Galvin R, Kennedy C, et al. Interventions for preventing falls in people with multiple sclerosis. Cochrane Database Syst Rev. 2019;11(11):CD012475; Epub ahead of print. CrossRef PubMed
- 8. Mehrholz J, Kugler J, Storch A, Pohl M, Hirsch K, Elsner B. Treadmill training for patients with Parkinson’s disease. Cochrane Database Syst Rev. 2015;2015(9):CD007830; Epub ahead of print. CrossRef PubMed
- 9. Ortega-Hombrados L, Molina-Torres G, Galán-Mercant A, Sánchez-Guerrero E, González-Sánchez M, Ruiz-Muñoz M. Systematic review of therapeutic physical exercise in patients with amyotrophic lateral sclerosis over time. Int J Environ Res Public Health. 2021;18(3):1074. CrossRef PubMed
- 10. Lai B, Lee E, Kim Y, et al. Leisure-time physical activity interventions for children and adults with cerebral palsy: a scoping review. Dev Med Child Neurol. 2021;63(2):162-171. CrossRef PubMed
- 11. Spielman LJ, Little JP, Klegeris A. Physical activity and exercise attenuate neuroinflammation in neurological diseases. Brain Res Bull. 2016;125:19-29. CrossRef PubMed
- 12. Motl RW, Pilutti LA. Is physical exercise a multiple sclerosis disease modifying treatment? Expert Rev Neurother. 2016;16(8):951-960. CrossRef PubMed
- 13. Winstein CJ, Stein J, Arena R, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98-e169. CrossRef PubMed
- 14. Haselkorn JK, Hughes C, Rae-Grant A, et al. Summary of comprehensive systematic review: rehabilitation in multiple sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2015;85(21):1896-1903. CrossRef PubMed
- 15. Keus S, Munneke M, Graziano M, et al. European Physiotherapy Guideline for Parkinson’s Disease. 2014;191. Online. Accessed November 2023.
- 16. Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56(4):308-321. CrossRef PubMed
- 17. Carroll DDC-LE, Courtney-Long EA, Stevens AC, et al; Centers for Disease Control and Prevention (CDC). Vital signs: disability and physical activity—United States, 2009-2012. MMWR Morb Mortal Wkly Rep. 2014;63(18):407-413. PubMed
- 18. Butler EN, Evenson KR. Prevalence of physical activity and sedentary behavior among stroke survivors in the United States. Top Stroke Rehabil. 2014;21(3):246-255. CrossRef PubMed
- 19. Casey B, Coote S, Galvin R, Donnelly A. Objective physical activity levels in people with multiple sclerosis: meta-analysis. Scand J Med Sci Sports. 2018;28(9):1960-1969. CrossRef PubMed
- 20. de Hollander EL, Proper KI. Physical activity levels of adults with various physical disabilities. Prev Med Rep. 2018;10:370-376. CrossRef PubMed
- 21. Joseph C, Conradsson D, Hagströmer M, Lawal I, Rhoda A. Objectively assessed physical activity and associated factors of sedentary behavior among survivors of stroke living in Cape Town, South Africa. Disabil Rehabil. 2018;40(21):2509-2515. CrossRef PubMed
- 22. Fini NA, Holland AE, Keating J, Simek J, Bernhardt J. How physically active are people following stroke? Systematic review and quantitative synthesis. Phys Ther. 2017;97(7):707-717. CrossRef PubMed
- 23. van den Berg-Emons RJ, Bussmann JB, Haisma JA, et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil. 2008;89(11):2094-2101. CrossRef PubMed
- 24. Moffat F, Paul L. Barriers and solutions to participation in exercise for moderately disabled people with multiple sclerosis not currently exercising: a consensus development study using nominal group technique. Disabil Rehabil. 2019;41(23):2775-2783. CrossRef PubMed
- 25. Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med. 2004;26(5):419-425. CrossRef PubMed
- 26. Shirazipour CH, Evans MB, Leo J, Lithopoulos A, Martin Ginis KA, Latimer-Cheung AE. Program conditions that foster quality physical activity participation experiences for people with a physical disability: a systematic review. Disabil Rehabil. 2020;42(2):147-155. CrossRef PubMed
- 27. Kunstler BE, Cook JL, Freene N, et al. Physiotherapist-led physical activity interventions are efficacious at increasing physical activity levels: a systematic review and meta-analysis. Clin J Sport Med. 2018;28(3):304-315. CrossRef PubMed
- 28. Keith RA, Cowell KS. Time use of stroke patients in three rehabilitation hospitals. Soc Sci Med. 1987;24(6):529-533. CrossRef PubMed
- 29. Williams TL, Smith B, Papathomas A. Physical activity promotion for people with spinal cord injury: physiotherapists’ beliefs and actions. Disabil Rehabil. 2018;40(1):52-61. CrossRef PubMed
- 30. Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. CrossRef PubMed
- 31. Cellule Planification de l’Offre des Professions des Soins de Santé. Statistiques Annuelles des professionnels des soins de santé en Belgique. Bruxelles: Service public fédéral (SPF) Santé publique, Sécurité de la Chaîne alimentaire et Environnement. Online. Accessed November 2023.
- 32. Nulty DD. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval High Educ. 2008;33(3):301-314. CrossRef
- 33. Daniel W. Biostatistics : a foundation for analysis in the health sciences. 7th ed. John Wiley & Sons; 1999.
- 34. Maisonneuve H, Fournier J-P. Construire une enquête et un questionnaire. E-respect[].2012;1(2):15-21.
- 35. Sammut R, Griscti O, Norman IJ. Strategies to improve response rates to web surveys: a literature review. Int J Nurs Stud. 2021;123:104058. CrossRef PubMed
- 36. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763-1768. CrossRef PubMed
- 37. Harris SR, Winstein CJ. The past, present, and future of neurorehabilitation: from NUSTEP through IV STEP and beyond. Pediatr Phys Ther. 2017;29(suppl 3):S2-S9. CrossRef PubMed
- 38. Aweto HA, Oligbo CN, Fapojuwo OA, Olawale OA. Knowledge, attitude and practice of physiotherapists towards promotion of physically active lifestyles in patient management. BMC Health Serv Res. 2013;13(1):21. CrossRef PubMed
- 39. Shirley D, van der Ploeg HP, Bauman AE. Physical activity promotion in the physical therapy setting: perspectives from practitioners and students. Phys Ther. 2010;90(9):1311-1322. CrossRef PubMed
- 40. Mohan N, Collins E, Cusack T, O’Donoghue G. Physical activity and exercise prescription: senior physiotherapists’ knowledge, attitudes and beliefs. Physiother Pract Res. 2012;33(2):71-80. CrossRef
- 41. Boakye H, Quartey J, Baidoo NAB, Ahenkorah J. Knowledge, attitude and practice of physiotherapists towards health promotion in Ghana. S Afr J Physiother. 2018;74(1):443. CrossRef PubMed
- 42. Tuna H, Bozan O, Elibol N, Unver B. Are the physical activity habits of Turkish physiotherapists associated with their physical activity promotion and counseling? Physiother Theory Pract. 2022;38(1):189-200. CrossRef PubMed
- 43. Mulligan H, Fjellman-Wiklund A, Hale L, Thomas D, Häger-Ross C. Promoting physical activity for people with neurological disability: perspectives and experiences of physiotherapists. Physiother Theory Pract. 2011;27(6):399-410. CrossRef PubMed
- 44. Kennedy W, Curtin C, Bowling A. Access to physical activity promotion for people with neurological conditions: are physical therapists leading the way? Disabil Health J. 2024;17(1):101517. CrossRef PubMed
- 45. Morris JH, Oliver T, Kroll T, Joice S, Williams B. From physical and functional to continuity with pre-stroke self and participation in valued activities: a qualitative exploration of stroke survivors’, carers’ and physiotherapists’ perceptions of physical activity after stroke. Disabil Rehabil. 2015;37(1):64-77. CrossRef PubMed
- 46. Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: a systematic review of reviews. PLoS One. 2017;12(7):e0180902. CrossRef PubMed
- 47. Eisele A, Schagg D, Göhner W. Exercise promotion in physiotherapy: a qualitative study providing insights into German physiotherapists’ practices and experiences. Musculoskelet Sci Pract. 2020;45:102104. CrossRef PubMed
- 48. Freene N, Cools S, Bissett B. Are we missing opportunities? Physiotherapy and physical activity promotion: a cross-sectional survey. BMC Sports Sci Med Rehabil. 2017;9(1):19. CrossRef PubMed
- 49. Prout EC, Mansfield A, McIlroy WE, Brooks D. Patients’ perspectives on aerobic exercise early after stroke. Disabil Rehabil. 2017;39(7):684-690. CrossRef PubMed
- 50. Watson PK, Eitivipart AC, Davis GM, Arora M, Middleton JW, De Oliveira CQ. Effects of behaviour change interventions on physical activity in people with spinal cord injury: a systematic review and meta-analysis. Psychol Sport Exerc. 2023;67:102408. CrossRef PubMed
- 51. Zhu S, Sherrington C, Jennings M, et al. Current practice of physical activity counselling within physiotherapy usual care and influences on its use: a cross-sectional survey. Int J Environ Res Public Health. 2021;18(9):4762. CrossRef PubMed
- 52. Declerck L, Stoquart G, Lejeune T, Vanderthommen M, Kaux J-F. Barriers to development and expansion of adaptive physical activity and sports for individuals with a physical disability in sports clubs and centres. Sci Sports. 2021;36(3):202-209. CrossRef
- 53. Albert FA, Crowe MJ, Malau-Aduli AEO, Malau-Aduli BS. Physical activity promotion: a systematic review of the perceptions of healthcare professionals. Int J Environ Res Public Health. 2020;17(12):4358. CrossRef PubMed
- 54. Giouridis N, Williams TL, Tomasone JR. Physical activity promotion to persons with spinal cord injury by health and exercise professionals: a scoping review. J Spinal Cord Med. 2023;46(1):126-145. CrossRef PubMed
- 55. Rethorn ZD, Covington JK, Cook CE, Bezner JR. Physical activity promotion attitudes and practices among outpatient physical therapists: results of a national survey. J Geriatr Phys Ther. 2021;44(1):25-34. CrossRef PubMed
- 56. Bowen PG, Mankowski RT, Harper SA, Buford TW. Exercise is medicine as a vital sign: challenges and opportunities. Transl J Am Coll Sports Med. 2019;4(1):1-7. CrossRef PubMed