 |
Arch Physioter 2024; 14: 11-19 ISSN 2057-0082 | DOI: 10.33393/aop.2024.2702 ORIGINAL RESEARCH ARTICLE |
 |
The psychometric properties of the modified fear of falling avoidance behavior questionnaire in Parkinson’s disease and older adults
ABSTRACT
Introduction: The Fear of Falling Avoidance Behavior Questionnaire (FFABQ) has good psychometric properties. However, we have recently modified the FFABQ (mFFABQ) to improve the clarity of the questions and Likert responses. This study aimed to examine the reliability and validity of this modified version in older adults and people with Parkinson’s disease (PD).
Methods: A total of 88 participants, 39 with PD (age = 72.2 ± 9.5; 29 males, 10 females) and 49 older adults (age = 72.8 ± 5.0; 13 males, 36 females), answered the mFFABQ twice, separated by 1 week, for test-retest reliability. Construct validity was evaluated through correlational analyses with fall history, Activities-Specific Balance Confidence Scale (ABC), Berg Balance Scale (BBS), Timed Up and Go, 30-Second Sit to Stand, Sensory Organization Test, Zung Anxiety Scale, Beck Depression Inventory, Consequences of Falling Questionnaire (CoFQ), and average daily activity levels using an activity monitor.
Results: The mFFABQ had good overall test-retest reliability (intraclass correlational coefficient [ICC] = 0.822; older adult ICC = 0.781, PD ICC = 0.806). The mFFABQ correlated with fall history (r = −0.430) and exhibited high correlation with the ABC (rho = −0.804) and moderate correlations with CoFQ (rho = 0.582) and BBS (rho = −0.595). The mFFABQ also correlated with time stepping (rho = −0.298) and number of steps (rho = −0.358).
Conclusion: These results provide supportive evidence for the reliability and validity of the mFFABQ in older adults and people with PD, which supports its suitability as a clinical and research tool for the assessment of fear of falling avoidance behavior.
Keywords: Balance, Balance confidence, Falls, Gait, Postural instability, Reliability
Received: October 27, 2023
Accepted: April 4, 2024
Published online: May 2, 2024
Archives of Physiotherapy - ISSN 2057-0082 - www.archivesofphysiotherapy.com
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0).
Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
What is known about the topic?
- Fear of falling avoidance behavior is common in older adults and people with Parkinson’s disease and, because of its negative downstream consequences, it is important that therapists have a way to reliably assess its impact.
What does the study add:
- This study adds evidence for the reliability and validity of the mFFABQ. Because it is clinically feasible and has sound psychometric properties, it is suitable for both the clinic and research lab.
Introduction
Falls are common in older adults and people with Parkinson’s disease (PD), with prevalence estimates of 26.5% (1) and 35%-90% (2), respectively. After a fall or near fall, fear of falling (FOF) can develop, which can lead to FOF avoidance behavior (FFAB). Interestingly, FFAB can also occur in those who have not had a recent fall (3). FFAB can be protective (adaptive) in that it may limit the occurrence of falls in the short term (4). That is, people with FOF may avoid risky tasks that threaten their balance, thereby protecting them from a future fall. However, excessive FFAB (maladaptive) may lead to a disproportionate amount of avoidance behavior, which reduces physical activity and increases sedentary behaviors (4). As a result of decreased activity, other downstream consequences may emerge, including physical deconditioning, weakened balance systems, poor bone health, social isolation, loneliness, and depression (4-6). Physical decline ultimately magnifies the consequences of avoidance behavior, leading to worsening balance function, thereby creating a vicious cycle (4,6).
The Fear of Falling Avoidance Behavior Questionnaire (FFABQ) was created as a tool for researchers and clinicians to quickly and reliably assess avoidance behavior (7). It has been shown to have sound psychometric properties (7) and to be associated with future falls in older adults (8). High FFABQ scores (high avoidance behavior) have also been shown to be related to emotional regulation and depression (9) and vision impairment in community-dwelling older adults (10). Furthermore, the FFABQ has contributed to research involving self-efficacy in older adults regarding fall prevention (11). Although the FFABQ has sound psychometrics, our experience suggests that the Likert responses (completely disagree, disagree, unsure, agree, completely agree) are unclear for some and may not match the sentence stem “Due to my FOF, I avoid [insert activity].” For this reason, there was a necessity to reexamine the language of the FFABQ and make improvements.
A modified version (mFFABQ) was subsequently created to improve the clarity of the Likert responses with the question stem. Specifically, the mFFABQ uses a different Likert response for each of the 14 items, which shifts the focus from agreement to quantification. In the mFFABQ, the item stem is the same, but the updated Likert responses provide a more quantitative focus for each activity: never (0% of the time), rarely (25% of the time), sometimes (50% of the time), often (75% of the time), and always (100% of the time). We believe that the updated mFFABQ responses align more clearly with the stem. The first aim of this study was to examine the test-retest reliability and minimal detectable change (MDC) of the mFFABQ to determine if it had properties similar to the original. The second aim of this study was to provide evidence of the construct validity of the mFFABQ in people with PD and older adults. Specifically, we hypothesized the following:
- The mFFABQ would be strongly correlated with the original FFABQ (criterion-related validity).
- Participants with PD, who theoretically have more balance and gait impairment, will have higher mFFABQ scores than older adult participants (known-groups validity).
- Fallers will have higher mFFABQ scores than non-fallers (known-groups validity).
- Measures of closely related constructs (e.g., balance confidence, balance performance, mobility and motor function, anxiety, depression, catastrophization) would moderately correlate with the mFFABQ as they should share some variance; strong correlations would not be expected since they are not measuring the same constructs.
- mFFABQ scores would be predictive of sedentary behavior and fall history and will have suitable cut points for clinical decision-making (predictive validity).
Methods
Study design
This study utilized a cross-sectional design for test-retest reliability wherein participants completed the mFFABQ twice, separated by approximately 1 week. One week was deemed a suitable wash-out period for remembering specific mFFABQ items, but not too long that there was a maturation effect (e.g., worsening or improving condition) or history effect (e.g., fall). All physical performance measures and additional questionnaires were administered during the in-person assessments at the Gait and Balance Research Laboratory at the University of Nevada, Las Vegas by members of the research team, except for the second administration of the mFFABQ. Participants with PD (n = 39) also completed the original FFABQ to allow for comparison of the two questionnaires. Participants wore activity monitors between the two assessments to collect data about their level of physical activity (e.g., time stepping, step count, time sitting/lying). The second mFFABQ was completed at home and returned at the same time as the activity monitor. Construct validity was examined by comparing the mFFABQ to the self-perceived balance confidence, balance, mobility, postural control, affective function, and physical activity levels. Known-groups and convergent validity were analyzed using these same measures.
Sample size estimation
The sample size was estimated using confidence intervals (CIs) for the intraclass correlation module in PASS 20.0.6 (NCSS, LLC.; Kaysville, Utah, USA). Based on data from the original FFABQ reliability study, a sample of 59 participants was needed for Aim 1 (reliability) (7). This estimation was based on a two-way mixed-effects analysis of variance (ANOVA) model (intraclass correlational coefficient [ICC] (3,1)) with each participant measured twice, a two-sided 95% CI with a width of 0.178, and an ICC of 0.815. For Aim 2 (validity), a sample size of 46 would achieve 80% power to detect a Pearson correlation coefficient of 0.40 for convergent validity analyses using a two-sided hypothesis test with a significance level of 0.05.
Participants
Inclusion criteria for both groups were the following: 60 to 90 years old; willingness to participate in one, 60-minute testing session; and willingness to wear an activity monitor for 1 week. Additional inclusion criteria for PD participants were that they had been diagnosed with PD by a neurologist. Participants were excluded if they were unable to read or speak English, exhibited evidence of dementia (Montreal Cognitive Assessment [MoCA] <18 or Mini-Mental State Exam <25) (13), or were unable to stand unassisted for 10 minutes. Participants were recruited from local PD support groups, senior centers, community events, and community centers through print advertisements and snowball recruitment. The study protocol was approved by the University of Nevada, Las Vegas Institutional Review Board. Data were collected from 2014 to 2023.
Measures
To examine construct validity, the mFFABQ was compared to the following:
- Self-perceived balance confidence: The Activities-Specific Balance Confidence Scale (ABC) (14)
- Balance, mobility, and postural control: Berg Balance Scale (BBS) (15), 30-Second Sit to Stand (30STS) (16), Timed Up and Go (TUG) (17), 2-minute step test (2MST) (18), and computerized dynamic posturography – Sensory Organization Test (SOT) (19)
- Affective function: Zung Anxiety Scale (ZAS) (20), Beck Depression Inventory (BDI) (21), and Consequences of Falling Questionnaire (CoFQ) (22)
- Physical activity levels: Average daily activity levels (i.e., time sitting/lying, time standing, time stepping, and number of steps) using a physical activity monitor
These measures and questionnaires were chosen for known-groups and convergent validity, permitting inferences regarding the validity of the mFFABQ.
mFFABQ. The mFFABQ is a 14-item self-report questionnaire with a 5-point Likert scale to measure FFAB (7). Item scores were summed to form a total score ranging from 0 to 56, with higher scores indicating more FFAB.
Self-perceived balance confidence
The ABC is a 16-item self-report measure that evaluates balance confidence during various activities of daily living (14). Evidence for the reliability and validity of the scale has been provided for older adults with and without PD (23,24).
Balance, mobility, and postural control
BBS. The BBS (25) was used as a performance-based balance scale with 14 functional balance tasks (25). It has good evidence for reliability (26) and validity (27) in predicting the risk of falls, multiple falls, and injurious falls in older adults with and without PD (28,29).
30STS. The 30STS was used to measure lower body strength in older adults (16). Evidence suggests excellent reliability in people with PD (30).
TUG. The TUG test was used as a measure of functional mobility in older adults (17). Evidence suggests good reliability and validity in older adults with and without PD (31).
2MST. The 2MST was used to assess aerobic capacity. Evidence suggests good reliability in older adults (18) and is strongly correlated with the Six-Minute Walk Test (32).
SOT. Bertec Balance Computerized Dynamic Posturography (Bertec®, Model 80P-0019, 2500 Citygate Drive, Columbus, OH) was used to calculate a composite balance score based on sway over six conditions (33). Evidence suggests good reliability in older adults (19) and has been shown to be a sensitive tool for identifying fall risk in people with PD (34,35).
Affective function
ZAS. The ZAS, a 20-item, self-report questionnaire, was used to measure anxiety (20). Scores range from 20 to 80 with a higher score indicating a higher level of anxiety (20).
BDI. The BDI, a 21-item self-administered questionnaire, was used to measure symptoms of depression (36). The overall score ranges from 0 to 63, with a higher score suggesting a higher level of depression. The BDI demonstrates high internal consistency in psychiatric and nonpsychiatric populations (37).
CoFQ. The CoFQ, a 12-item, self-report questionnaire, was used to measure catastrophization related to falling (22). The total score ranges from 12 to 48, with a higher score suggesting more catastrophization about falling. It has two subscales, damage to identity and loss of functional independence. Evidence suggests excellent internal reliability and moderate test-retest reliability in older adults (22).
Physical activity levels
Activity monitor. Physical activity levels were measured using ActivPAL activity monitors (PAL Technologies Ltd., Glasgow, United Kingdom) over a 7-day period. Any devices returned with less than 5 days of data were excluded from the analyses. Data extracted included the number of hours per day that the participant was sitting, lying down, biking, or standing. In addition, total steps and time stepping per day were collected.
Data analysis
Data were analyzed using SPSS version 28.0 (IBM SPSS Statistics for Windows, IBM Corp, Armonk, NY, USA) with α = 0.05. For Aim 1 (reliability), a two-way mixed-effects ANOVA model ICC (3,1) was used for the two mFFABQ measurements. The MDCs were calculated based on the Standard Error of Measurement (SEM) using the test-retest reliability statistic (ICC value) where rxx = test-retest reliability:  (38). Once SEM was determined, the MDC at the 95% confidence level was calculated by multiplying the SEM by 1.96 (representing 95% of the area under the curve of a normal distribution) and 1.41 (the square root of 2, to control for possible error associated with calculating the coefficient from two time points). Aim 2 (validity) of the study was to provide evidence for the criterion-related validity of the mFFABQ relative to the original FFABQ; these were compared using Spearman’s rho. Additionally, construct validity for the mFFABQ was conducted using known-groups and convergent validity analyses. Known-group analysis was used to determine if there were differences between those with PD and healthy older adults on the mFFABQ. In addition, differences were explored based on fall history, which included fallers or non-fallers in the previous year (fall status), fallers and non-fallers in the previous month (fall recency), and injurious fallers and non-injurious fallers in the previous year (fall injury) on mFFABQ scores via t-tests. Convergent validity was evaluated by comparing the mFFABQ to measures of similar constructs using Spearman’s rho. Since there was likely a nonlinear relationship with falls over time (inverted U curve) (4), the ratio of the number of falls (falls in the last year, last month, and injurious falls) per average daily steps taken was compared to the mFFABQ using Spearman’s rho. To determine the optimal cut point for the mFFABQ on sedentary behavior (step-defined sedentary lifestyle index of <5,000 steps per day) (39) and fall history (one or more falls in the last year), the area under the receiver operating characteristic (ROC) curve was calculated and the Youden Index (maximum vertical distance or difference between the ROC curve and the diagonal or chance line) was used to optimize the mFFABQ’s ability, given both sensitivity and specificity.
(38). Once SEM was determined, the MDC at the 95% confidence level was calculated by multiplying the SEM by 1.96 (representing 95% of the area under the curve of a normal distribution) and 1.41 (the square root of 2, to control for possible error associated with calculating the coefficient from two time points). Aim 2 (validity) of the study was to provide evidence for the criterion-related validity of the mFFABQ relative to the original FFABQ; these were compared using Spearman’s rho. Additionally, construct validity for the mFFABQ was conducted using known-groups and convergent validity analyses. Known-group analysis was used to determine if there were differences between those with PD and healthy older adults on the mFFABQ. In addition, differences were explored based on fall history, which included fallers or non-fallers in the previous year (fall status), fallers and non-fallers in the previous month (fall recency), and injurious fallers and non-injurious fallers in the previous year (fall injury) on mFFABQ scores via t-tests. Convergent validity was evaluated by comparing the mFFABQ to measures of similar constructs using Spearman’s rho. Since there was likely a nonlinear relationship with falls over time (inverted U curve) (4), the ratio of the number of falls (falls in the last year, last month, and injurious falls) per average daily steps taken was compared to the mFFABQ using Spearman’s rho. To determine the optimal cut point for the mFFABQ on sedentary behavior (step-defined sedentary lifestyle index of <5,000 steps per day) (39) and fall history (one or more falls in the last year), the area under the receiver operating characteristic (ROC) curve was calculated and the Youden Index (maximum vertical distance or difference between the ROC curve and the diagonal or chance line) was used to optimize the mFFABQ’s ability, given both sensitivity and specificity.
Results
Participants
Ninety-one participants were recruited for the study, 3 participants were excluded due to missing data points, and 3 were excluded due to dementia. A total of 39 participants (age = 72.2 ± 9.5; 29 males, 10 females) diagnosed with PD (Hoehn and Yahr [HY] (12) median and mode = 3.0; frequencies – HY Stage 1 [n = 10], HY Stage 1.5 [n = 1], HY Stage 2 [n = 6], HY Stage 2.5 [n = 1], HY Stage 3 [n = 20], HY Stage 4 [n = 1]) and 49 healthy older adults (age = 72.9 ± 5.0; 13 males, 36 females) participated (Tab. 1).
| Overall
(n = 88) |
People with PD (n = 39, 44.3%) | Older adults
(n = 49, 55.7%) |
||
|---|---|---|---|---|
| Demographics | Age | 72.6 ± 7.3 | 72.2 ± 9.5 | 72.9 ± 5.0 |
| Sex | 42 males (47.7%)
46 females (52.3%) |
29 males (74.4%)
10 females (25.6%) |
13 males (26.5%)
36 females (73.5%) |
|
| PD-specific characteristics | MDS-UPDRS overall | Not applicable | 66.2 ± 31.7 | Not applicable |
| MDS-UPDRS Part 1: mental | 13.4 ± 7.3 | |||
| MDS-UPDRS Part 2: activities of daily living | 17.3 ± 10.8 | |||
| MDS-UPDRS Part 3: motor | 30.2 ± 16.8 | |||
| Freezing of gait from MDS-UPDRS, item 2.13 | No freezing = 24
Slight = 6 Mild = 3 Moderate = 2 Severe = 1 |
|||
| PDQ39 | 25.1 ± 15.8 | |||
| Balance confidence | ABC | 75.2 ± 24.5 | 64.2 ± 25.9 | 84.2 ± 19.2 |
| Balance, mobility, and postural control | Falls in the last year (#) | 6.8 ± 37.7
Median = 0 (0-350) |
14.5 ± 56.1
Median = 0 (0-350) |
0.7 ± 1.0
Median = 0 (0-3) |
| Falls in the last month (#) | 0.7 ± 3.3
Median = 0 (0-30) |
1.4 ± 5.0
Median = 0 (0-30) |
1.1 ± 0.3
Median = 0 (0-1) |
|
| Injurious falls in the last year (#) | 0.4 ± 1.1
Median = 0 (0-8) |
0.6 ± 1.4
Median = 0 (0-8) |
1.2 ± 0.7
Median = 0 (0-3) |
|
| BBS (scale points) | 49.8 ± 9.5 | 44.4 ± 12.1 | 54.1 ± 2.4 | |
| 30STS (#) | 10.2 ±5.5 | 8.5 ± 7.1 | 11.6 ± 3.4 | |
| TUG (seconds) | 10.9 ± 5.0 | 13.4 ± 6.3 | 8.9 ± 2.3 | |
| 2MST (#) | 65.8 ± 34.0 | 50.0 ± 37.2 | 78.4 ± 25.2 | |
| SOT composite (equilibrium score) | 62.4 ± 18.0 | 65.3 ± 26.6 | 62.2 ± 17.7 | |
| Affective function | ZAS (scale points) | 41.4 ± 10.5 | 43.7 ± 11.1 | 39.7 ± 9.7 |
| BDI (scale points) | 8.8 ± 8.0 | 12.2 ± 9.3 | 6.1 ± 5.5 | |
| CoFQ (scale points) | 24.7 ± 6.6 | 27.4 ± 5.1 | 22.6 ± 7.0 | |
| Physical activity levels | Time sitting/lying per day (hours) | 18.8 ± 2.4 | 19.5 ± 2.2 | 18.2 ± 2.3 |
| Time standing per day (hours) | 3.7 ± 1.9 | 3.6 ± 1.8 | 3.9 ± 2.0 | |
| Time stepping per day (hours) | 1.3 ± 0.7 | 0.9 ± 0.6 | 1.6 ± 0.7 | |
| Number of daily steps (steps) | 6,131.6 ± 3,696.5
Median = 5,924 (11-18,457) |
4,471.4 ± 2,964.5
Median = 3,966 (11-10,536) |
7,533.6 ± 3,699.1
Median = 6,999 (1,973-18,457) |
|
2MST = Two-Minute Step Test; 30STS = 30-Second Sit to Stand; ABC = Activities-Specific Balance Confidence Scale; BBS = Berg Balance Scale; BDI = Beck Depression Inventory; CoFQ = Consequences of Falling Questionnaire; MDS-UPDRS = Movement Disorders Society Unified Parkinson’s Disease Rating Scale; PD = Parkinson’s disease; PDQ39 = Parkinson’s Disease Questionnaire – 39; SOT = Sensory Organization Test; TUG = Timed Up and Go; ZAS = Zung Anxiety Scale.
Reliability
The mFFABQ demonstrated good overall reliability, ICC(3,1) = 0.822 (95% CI: 0.739-0.881) for all participants, including those with mild cognitive impairment. The mFFABQ demonstrated good overall test-retest reliability for older adults and people with PD, ICC (3,1) = 0.781 (95% CI: 0.636-0.871) and 0.806 (95% CI: 0.658-0.894), respectively. The 95% MDC was 14.8 scale points for the overall sample and 12.2 and 17.7 scale points for older adults and people with PD, respectively.
Criterion-related validity
The correlation between the mFFABQ (average of the two scores) and the original FFABQ was rho = 0.874, p < 0.001.
Known-groups validity
Participants with PD had higher mFFABQ scores than older adults, p < 0.001 (Tab. 2). Participants who reported at least one fall in the previous year (“fallers”) during the in-person assessment had higher mFFABQ scores than non-fallers, p < 0.001 (Tab. 2). Participants who had experienced a fall in the previous month (“recent faller”) had higher mFFABQ scores than nonrecent fallers, p = 0.208 (Tab. 2). There was no difference between those who had experienced a fall injury in the previous year and those who had not, p = 0.471 (Tab. 2).
| Comparison | Group | mFFABQ | SEM | Cohen’s D with 95% CI (Hedges correction) | Statistic | p-Value |
|---|---|---|---|---|---|---|
| Diagnosis | People with PD (n = 38, 44.7%) | 16.4 | 2.3 | 0.777 (0.335 to 1.215) | t = 3.596 | <0.001 |
| Healthy older adults (n = 47, 55.3%) | 7.6 | 1.3 | ||||
| Fall status | Fallers (n = 44, 51.8%) | 16.4 | 2.1 | 0.917 (0.471 to 1.359) | t = 4.264 | <0.001 |
| Non-fallers (n = 41, 48.2%) | 6.3 | 1.1 | ||||
| Fall recency | Recent fallers (n = 15, 17.6%) | 15.1 | 2.4 | 0.357 (−0.199 to 0.912) | t = 1.268 | 0.208 |
| Nonrecent faller (n = 70, 82.4%) | 10.8 | 1.5 | ||||
| Fall injury | Fall injury (n = 20, 23.5%) | 13.3 | 2.1 | −0.184 (−0.681 to 0.314) | t = −0.725 | 0.471 |
| Nonfall injury (n = 65, 76.5%) | 11.0 | 1.6 |
CI, confidence interval; mFFABQ = modified Fear of Falling Avoidance Behavior Questionnaire; PD = Parkinson’s disease; SEM = standard error of the mean.
Convergent validity
For all participants, the mFFABQ was significantly correlated with fall history (fall status rho = −0.430, p < 0.001) and fall recency (rho = −0.235, p = 0.031) but not with fall injuries (rho = 0.173, p = 0.113). The correlations between the mFFABQ and the ratio of steps per day and falls (fall-to-step) were as follows: falls/year/step (rho = 0.630, p < 0.001), falls/month/steps (rho = 0.209, p = 0.189), and injurious falls/year/steps (rho = 0.172, p = 0.282). The mFFABQ also correlated with the ABC (rho = −0.804, p < 0.001), BBS (rho = −0.595, p < 0.001), TUG (rho = 0.560, p < 0.001), and 30STS (rho = −0.386, p < 0.001). The mFFABQ correlated with the ZAS (rho = 0.428, p < 0.001), BDI (rho = 0.606, p < 0.001), and CoFQ (rho = 0.582, p < 0.001) including damage to identity (rho = 0.608, p < 0.001) and loss of functional independence (rho = 0.497, p < 0.001) subscales of the CoFQ. For physical activity, the mFFABQ did not correlate with sitting/lying (rho = 0.129, p = 0.248) or standing time (rho = −0.072, p = 0.520); however, it did correlate with time stepping (rho = −0.298, p = 0.007) and number of steps (rho = −0.358, p < 0.001) in a direction consistent with the hypotheses and the construct.
Predictive validity
The area under the ROC curve was 0.720 (95% CI: 0.613-0.828) with an optimal cut point of 11.5 on the mFFABQ (scores range from 0 to 56) for predicting sedentary behavior (<5,000 steps per day) (39) (Fig. 1). The sensitivity and specificity of the 11.5 cut point were 0.667 and 0.702, respectively. The area under the ROC curve for fall history (one or more falls in the last year) was 0.723 (95% CI: 0.618-0.827) and the optimal cut point was 13.5, with a sensitivity of 0.551 and specificity of 0.810 (Fig. 2).
Discussion
An important objective of the original FFABQ was to create a reliable, clinically feasible, and accessible tool to assess FFAB (7). The changes made in the mFFABQ were implemented to improve clarity and, thus, reliability and validity. Our results provide evidence that the mFFABQ has acceptable reliability for the overall sample (ICC = 0.822), older adults (ICC = 0.781), and people with PD (ICC = 0.806). Although these reliability coefficients are solidly in the “good reliability” range (40), they represent modest improvements over the original FFABQ (overall ICC = 0.812) and for people with neurological conditions (ICC = 0.751) (7). The reliability coefficients for the mFFABQ were consistent with the Brazilian Portuguese FFABQ in older adults (ICC = 0.810) (41) but were lower than the Turkish FFABQ in older adults (ICC = 0.999) (42). Based on these data, we recommend that both the FFABQ and mFFABQ are suitable for clinical or research use. Still, we favor the mFFABQ because the Likert options are more quantitative and, based on our experience, make more theoretical sense to the research team and some of the participants than the original. While we did not keep track, there were more clarifying questions from participants about the FFABQ than the mFFABQ. Additionally, the modest improvements in the reliability coefficients support our recommendation to use the mFFABQ. Also, there have been no studies reporting evidence for the validity and reliability of the original FFABQ in a PD population; thus, the evidence reported in this study for the mFFABQ supports our recommendation for its use. In addition, with an MDC of 15 scale points (14.8), which is consistent with the original, a therapist or researcher can be confident that a change in score beyond this value would be indicative of an increase or decrease beyond error at 95% of confidence in FFAB.
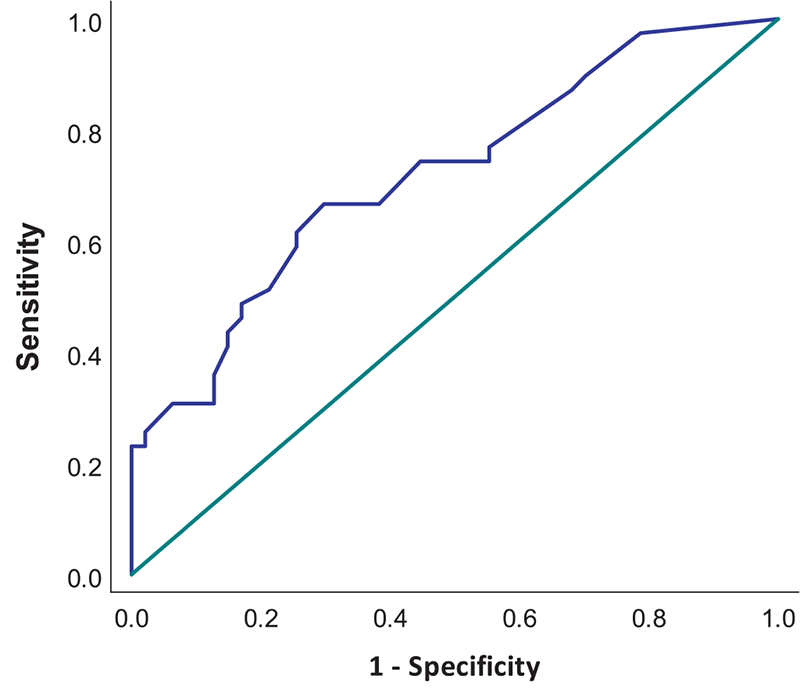
FIGURE 1 - Receiver operating characteristic (ROC) curve for the modified Fear of Falling Avoidance Behavior Questionnaire (mFFABQ) on sedentary activity (<5,000 steps per day).
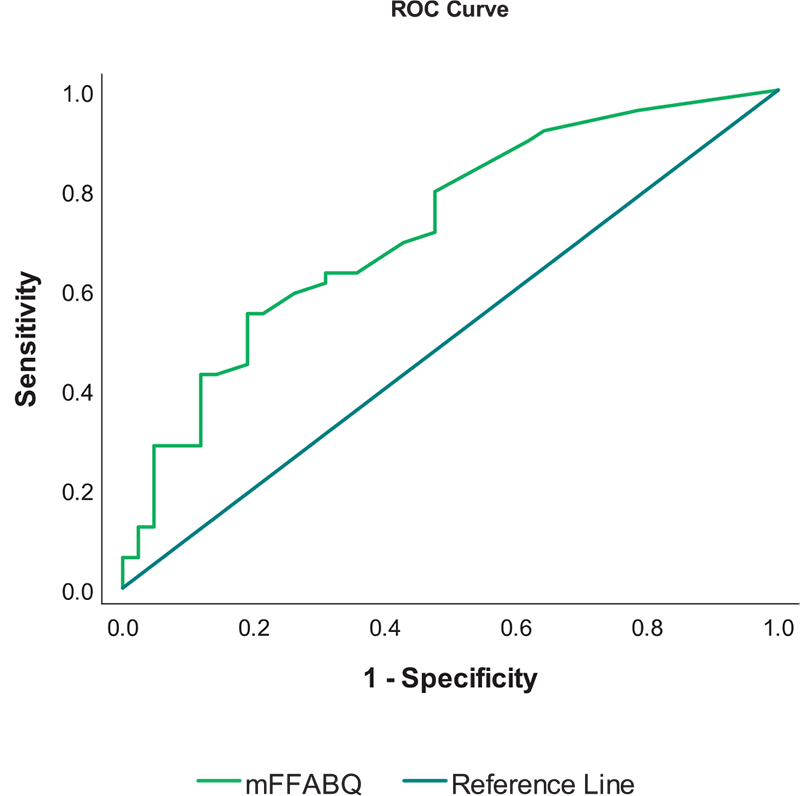
FIGURE 2 - Receiver operating characteristic (ROC) curve for the modified Fear of Falling Avoidance Behavior Questionnaire (mFFABQ) on fall history (one or more falls in the last year).
The criterion-related validity of the mFFABQ was supported by its strong correlation with the original FFABQ as initially hypothesized. In the original study of the FFABQ, the results supported the notion that the FFABQ measured FFAB rather than balance confidence, self-efficacy, or fear (7). The results of the present study are consistent with the original study and further support the validity of these instruments. Likewise, as hypothesized, the results of the known-groups analyses support the validity of the mFFABQ. That is, those with gait and balance dysfunction inherent to their disease (known group [PD]) would have higher mFFABQ scores (i.e., more FFAB) than healthy older adults, who would logically have less gait and balance dysfunction and, subsequently, lower mFFABQ scores. This was indeed the case, and these differences were also observed among other known groups, including fallers and recent fallers. These results add evidence about the validity of the mFFABQ in these populations in discriminating between two known groups that would logically differ in the construct of the instrument.
Similar to the original FFABQ (7), the mFFABQ correlated with performance-based balance measures (i.e., BBS, TUG, and 30STS), which supports the convergent validity of the mFFABQ. The correlations between these performance-based tools make theoretical sense because they are in the same gait and balance domain. It was hypothesized that the correlations would be moderate. If the correlations would have been strong, then that would suggest that they were measuring the same construct or significantly overlapping constructs. The strongest correlation was found with the ABC. This is logical because balance self-confidence is a closer construct to FOF and, subsequently, FFAB. The directionality and strength of these correlations are consistent with the results from the Brazilian Portuguese FFABQ translation, reliability, and validity study (41) but were lower than the Turkish FFABQ translation, reliability, and validity, which reported stronger correlations (42). Despite being in the same domain, fall history was not consistently or strongly correlated with the mFFABQ, reinforcing the idea that falls are nonlinear over time or as a disease progresses (inverted U curve) (4). It is theorized that individuals with high FOF and FFAB, triggered by decreased balance capability/confidence, limit or recalibrate their exposure to risky balance conditions and, thus, are less likely to fall (4). Moreover, the correlations between the mFFABQ and measures in the gait and balance domain suggest that individuals with increased FFAB are likely to demonstrate impaired balance with functional activities (4). This supports the notion that increased FFAB may decrease fall frequency but does not decrease postural instability (43).
In additional support of the construct of validity of the mFFABQ, there were also moderate, positive correlations with the following scales in the affective domain: ZAS (anxiety), BDI (depression), and CoFQ (catastrophization). These results are consistent with our original hypotheses and are also consistent with other studies (5,44). While many consider anxiety and fear to be related (both deal with the idea of danger or threat) but different constructs (fear is seen as a reaction to a specific, observable threat, while anxiety is worry about a future threat that has not happened or may never happen), they are clearly interrelated and it is not surprising that there are moderate correlations between these constructs and FFAB. However, the cause-and-effect direction is not known from our study and, subsequently, it is possible that this relationship could be bidirectional, with FOF triggering a generalized anxiety disorder or, alternatively, someone with an anxiety disorder could be more susceptible to developing fear in other aspects of their life. The relationship could also be more complex with mediator and moderator effects. Likewise, the relationship with depression makes theoretical sense and could also be bidirectional. One theory regarding this is that FFAB may have downstream consequences such as social isolation and loneliness, which could, in turn, trigger or exacerbate depression (4). Furthermore, as hypothesized, there was a moderate correlation with the CoFQ (catastrophization), particularly the damage to identity subsection. This is consistent with research suggesting that the FFAB is more strongly correlated with damage to identity (i.e., the immediate consequences of pain, shame, and embarrassment) than loss of functional independence (i.e., enduring consequences of injury and disability) in people with PD (44). From a clinical context, it is important to holistically consider the associations of the mFFABQ with constructs in the affective domains and to collaborate with other members of the healthcare team with expertise in this area. Because therapists frequently encounter FOF and FFAB during gait and balance treatment, it is important that therapists become well-versed in these areas to mitigate the consequences and optimize care.
As hypothesized, convergent validity of the mFFABQ was also supported by moderate correlations with time stepping and the number of steps taken on average per day. Because avoidance behavior likely affects activity levels, these correlations support the notion that those with high avoidance behavior exhibit more sedentary behavior (less time stepping and fewer steps per day). As functional balance declines, a person is likely to cope through increased sedentary behaviors and avoiding activities that challenge balance (45). These results are consistent with other studies in the literature for people with PD and support the notion of a vicious cycle of FFAB (4-6). In addition, predictive validity was supported by the ROC analyses, which suggest that the mFFABQ is predictive of sedentary behavior (i.e., less than 5,000 steps per day) at a cut-off score of 11.5 (AUC = 0.720) and also falls within the last year (AUC = 0.723 with a 13.5 mFFABQ cut point). These results are consistent with FFAB predicting future falls in older adults (8). From a clinical perspective, because FFAB may have several negative downstream consequences, including a vicious cycle (4,6), the mFFABQ may be a helpful clinical tool in a comprehensive examination for clinical decision-making related to sedentary behavior, activity limitation and participation restriction, fall and balance behavior, and outcomes of different treatment approaches to mitigate the downstream consequences of FFAB. These treatment approaches may include high-intensity multimodal exercise with balance training (46) and cognitive behavioral therapy (4,47,48).
One of the limitations of this study was that many participants had low FFAB, especially in the older adult group. Recruiting people with high FFAB is challenging because their FFAB makes them less likely to leave their homes and travel to an urban campus, which would likely entail significant walking, physical performance tests, and other factors that would feed into their FOF. Thus, the results of this study may not be fully generalizable to typical clinical populations that are most likely to be seen and evaluated for gait and balance problems. Future research in this area should consider conducting assessments in participant homes to remove some barriers to participation for individuals with high FFAB. Another limitation was that the sample size estimation was for the overall sample and, subsequently, the subgroups may not have been sufficiently powered. Therefore, the subgroup analyses should be interpreted with some caution. However, psychometrically, the subgroup analyses were actually quite strong so this may only be a minor concern. Another limitation was that the sex proportion of the participants was different in the participants with PD (males > females) and older adults (females > males). Neither of these proportions are inconsistent with expectations of clinical research in these populations (i.e., there are more males with PD, more females volunteer for research studies); however, this does limit the generalizability. Another limitation is that two scales that also measure the construct of FFAB, the Falls Efficacy Scale – International (49) and Survey of Activities and Fear of Falling in the Elderly (50), were not included in this study. They would have added support to the construct validity of the mFFABQ. Lastly, only participants with PD completed both the original and modified versions of the FFABQ; therefore, the correlational data reported in this article should be interpreted with caution and should not be generalized to older adults.
Conclusions
The results of this study provide sound psychometric support for the use of the mFFABQ as a clinical or research measure for FFAB in older adults and people with PD. Similar to the original FFABQ, the mFFABQ exhibited good reliability and demonstrated good evidence of its validity in the measurement of the construct of FFAB. These results also demonstrated a modest improvement in psychometric properties relative to the original and, therefore, it is recommended that clinicians and researchers use the updated, mFFABQ version. However, the original FFABQ remains a suitable measure. Researchers and clinicians should adhere to a single scale and not intermix them.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions: Conceptualization (MRL), data curation (MRL, AMH, AA, BL), formal analysis (MRL, AMH, AA, BL, AAB), investigation/methodology (MRL, AMH, AA, BL, AAB), project administration (MRL, JVR, JKL), writing – original draft (MRL, AMH, AA, BL), writing – review and editing (MRL, AMH, AA, BL, AAB, JVR, JKL).
Data availability statement: Data for this study are not currently available as this was not stipulated in the IRB-approved protocol.
Ethics approval statement: Ethical approval was received from the University of Nevada, Las Vegas Biomedical Institutional Review Board. All authors have adhered to the ethical standards stipulated in the IRB-approved trial.
Patient consent statement: All participants consented to participate by signing an IRB-approved consent form.
References
- 1. Salari N, Darvishi N, Ahmadipanah M, Shohaimi S, Mohammadi M. Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2022;17(1):334. CrossRef PubMed
- 2. Allen NE, Schwarzel AK, Canning CG. Recurrent falls in Parkinson’s disease: a systematic review. Parkinsons Dis. 2013;2013:906274. CrossRef PubMed
- 3. Lee S, Oh E, Hong GS. Comparison of factors associated with fear of falling between older adults with and without a fall history. Int J Environ Res Public Health. 2018;15(5):982. CrossRef PubMed
- 4. Landers MR, Nilsson MH. A theoretical framework for addressing fear of falling avoidance behavior in Parkinson’s disease. Physiother Theory Pract. 2023;39(5):895-911. CrossRef PubMed
- 5. Landers MR, Lopker M, Newman M, Gourlie R, Sorensen S, Vong R. A cross-sectional analysis of the characteristics of individuals with Parkinson disease who avoid activities and participation due to fear of falling. J Neurol Phys Ther. 2017;41(1):31-42. CrossRef PubMed
- 6. Landers MR, Jacobson KM, Matsunami NE, McCarl HE, Regis MT, Longhurst JK. A vicious cycle of fear of falling avoidance behavior in Parkinson’s disease: a path analysis. Clin Park Relat Disord. 2021;4:100089. CrossRef PubMed
- 7. Landers MR, Durand C, Powell DS, Dibble LE, Young DL. Development of a scale to assess avoidance behavior due to a fear of falling: the Fear of Falling Avoidance Behavior Questionnaire. Phys Ther. 2011;91(8):1253-1265. CrossRef PubMed
- 8. Landers MR, Oscar S, Sasaoka J, Vaughn K. Balance confidence and fear of falling avoidance behavior are most predictive of falling in older adults: prospective analysis. Phys Ther. 2016;96(4):433-442. CrossRef PubMed
- 9. Scarlett L, Baikie E, Chan SWY. Fear of falling and emotional regulation in older adults. Aging Ment Health. 2019;23(12):1684-1690. CrossRef PubMed
- 10. Lee SP, Hsu YW, Andrew L, Davis T, Johnson C. Fear of falling avoidance behavior affects the inter-relationship between vision impairment and diminished mobility in community-dwelling older adults. Physiother Theory Pract. 2022;38(5):686-694. CrossRef PubMed
- 11. Soh SL, Tan CW, Thomas JI, et al. Falls efficacy: extending the understanding of self-efficacy in older adults towards managing falls. J Frailty Sarcopenia Falls. 2021;6(3):131-138. CrossRef PubMed
- 12. Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427-442. CrossRef PubMed
- 13. Hoops S, Nazem S, Siderowf AD, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology. 2009;73(21):1738-1745. CrossRef PubMed
- 14. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28-M34. CrossRef PubMed
- 15. Berg K, Wood-Dauphinee S, Willliams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304-311. CrossRef
- 16. Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. 1999;7(2):127-129. CrossRef
- 17. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148. CrossRef PubMed
- 18. Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53(2):255-267. CrossRef PubMed
- 19. Ford-Smith CD, Wyman JF, Elswick RK Jr, Fernandez T, Newton RA. Test-retest reliability of the sensory organization test in noninstitutionalized older adults. Arch Phys Med Rehabil. 1995;76(1):77-81. CrossRef PubMed
- 20. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371-379. CrossRef PubMed
- 21. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561-571. CrossRef PubMed
- 22. Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42(1):17-23. CrossRef PubMed
- 23. Talley KM, Wyman JF, Gross CR. Psychometric properties of the activities-specific balance confidence scale and the survey of activities and fear of falling in older women. J Am Geriatr Soc. 2008;56(2):328-333. CrossRef PubMed
- 24. Jonasson SB, Nilsson MH, Lexell J. Psychometric properties of four fear of falling rating scales in people with Parkinson’s disease. BMC Geriatr. 2014;14(1):66. CrossRef PubMed
- 25. Donoghue D, Stokes EK; Physiotherapy Research and Older People (PROP) group. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343-346. CrossRef PubMed
- 26. Meseguer-Henarejos AB, Rubio-Aparicio M, López-Pina JA, Carles-Hernández R, Gómez-Conesa A. Characteristics that affect score reliability in the Berg Balance Scale: a meta-analytic reliability generalization study. Eur J Phys Rehabil Med. 2019;55(5):570-584. CrossRef PubMed
- 27. Park SH, Lee YS. The diagnostic accuracy of the Berg Balance Scale in predicting falls. West J Nurs Res. 2017;39(11):1502-1525. CrossRef PubMed
- 28. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449-459. CrossRef PubMed
- 29. Qutubuddin AA, Pegg PO, Cifu DX, Brown R, McNamee S, Carne W. Validating the Berg Balance Scale for patients with Parkinson’s disease: a key to rehabilitation evaluation. Arch Phys Med Rehabil. 2005;86(4):789-792. CrossRef PubMed
- 30. Petersen C, Steffen T, Paly E, Dvorak L, Nelson R. Reliability and minimal detectable change for Sit-to-Stand Tests and the Functional Gait Assessment for individuals with Parkinson disease. J Geriatr Phys Ther. 2017;40(4):223-226. CrossRef PubMed
- 31. Christopher A, Kraft E, Olenick H, Kiesling R, Doty A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: a systematic review. Disabil Rehabil. 2021;43(13):1799-1813. CrossRef PubMed
- 32. Berlanga LA, Matos-Duarte M, Abdalla P, Alves E, Mota J, Bohn L. Validity of the two-minute step test for healthy older adults. Geriatr Nurs. 2023;51:415-421. CrossRef PubMed
- 33. Grove CR, Whitney SL, Hetzel SJ, Heiderscheit BC, Pyle GM. Validation of a next-generation sensory organization test in adults with and without vestibular dysfunction. J Vestib Res. 2021;31(1):33-45. CrossRef PubMed
- 34. Freeman L, Gera G, Horak FB, Blackinton MT, Besch M, King L. Instrumented test of sensory integration for balance: a validation study. J Geriatr Phys Ther. 2018;41(2):77-84. CrossRef PubMed
- 35. Rossi-Izquierdo M, Basta D, Rubio-Rodríguez JP, et al. Is posturography able to identify fallers in patients with Parkinson’s disease? Gait Posture. 2014;40(1):53-57. CrossRef PubMed
- 36. Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77-100. CrossRef
- 37. Wang YP, Gorenstein C. Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Br J Psychiatry. 2013;35(4):416-431. CrossRef PubMed
- 38. Beaton DE, Bombardier C, Katz JN, Wright JG. A taxonomy for responsiveness. J Clin Epidemiol. 2001;54(12):1204-1217. CrossRef PubMed
- 39. Tudor-Locke C, Craig CL, Thyfault JP, Spence JC. A step-defined sedentary lifestyle index: <5000 steps/day. Appl Physiol Nutr Metab. 2013;38(2):100-114. CrossRef PubMed
- 40. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. CrossRef PubMed
- 41. Nunes ACL, Jesus-Moraleida FR, Lima POP, Landers MR. Translation, cross-cultural adaptation, and measurement properties of the Brazilian-Portuguese version of the fear of falling avoidance behavior questionnaire in older adults. J Aging Phys Act. 2022;30(6):1014-1023. CrossRef PubMed
- 42. Acaröz Candan S, Demircioğlu A, Şahin ÜK. Cross-cultural adaptation and psychometric properties of the Fear of Falling Avoidance Behavior Questionnaire in Turkish community-dwelling older adults. Disabil Rehabil. 2021;43(23):3387-3394. CrossRef PubMed
- 43. Longhurst JK, Rider JV, Eckard K, et al. Factors predicting fear of falling avoidance behavior in parkinsonisms. NeuroRehabilitation. 2022;50(1):65-73. CrossRef PubMed
- 44. Rider JV, Longhurst JK, Lekhak N, Navalta JW, Young DL, Landers MR. Psychological factors associated with fear of falling avoidance behavior in Parkinson’s disease: the role of depression, anxiety, and catastrophizing. J Geriatr Psychiatry Neurol. 2023 May;36(3):215-224. CrossRef PubMed
- 45. Nilsson MH, Drake AM, Hagell P. Assessment of fall-related self-efficacy and activity avoidance in people with Parkinson’s disease. BMC Geriatr. 2010;10(1):78. CrossRef PubMed
- 46. Landers MR, Navalta JW, Murtishaw AS, Kinney JW, Pirio Richardson S. A high-intensity exercise boot camp for persons with Parkinson disease: a phase II, pragmatic, randomized clinical trial of feasibility, safety, signal of efficacy, and disease mechanisms. J Neurol Phys Ther. 2019;43(1):12-25. CrossRef PubMed
- 47. Tennstedt S, Howland J, Lachman M, Peterson E, Kasten L, Jette A. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci. 1998;53(6):384-392. CrossRef PubMed
- 48. Dorresteijn TA, Zijlstra GA, Ambergen AW, Delbaere K, Vlaeyen JW, Kempen GI. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial. BMC Geriatr. 2016;16(1):2. CrossRef PubMed
- 49. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614-619. CrossRef PubMed
- 50. Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci. 1998;53(1):43-50. CrossRef PubMed