 |
AboutOpen | 2024; 11: 18-20 ISSN 2465-2628 | DOI: 10.33393/ao.2024.2736 CASE REPORT |
 |
Fournier’s gangrene wounds successfully healed with High pbserum enzymes: a case report
ABSTRACT
Fournier’s gangrene is an aggressive form of infective necrotizing fasciitis in the perianal and genital area. In this article we discuss the case of a 75-year-old male patient diagnosed with Fournier’s gangrene with the entire perianal region affected. Surgical washings were performed and debridement with multiple flaps were required for reconstruction. Complications in the suture wounds, cavities, and a seroma were observed after 5 weeks, and they were treated with dressings. Treatment with High pbserum recombinant enzymes was initiated after 3 weeks, to accelerate the closure of the wounds. The granulation tissue was irrigated by drip irrigation once every 3 weeks, ensuring good tissue impregnation. We observed that the epithelialization of the affected areas was achieved after the first week, and in 1 month, most of the wounds healed properly without signs of infection. High pbserum is an enzyme cocktail, composed of higher collagenase concentration, lipase, and liase. This study shows how High pbserum improves and accelerates wound healing in a patient with Fournier’s gangrene. Further investigations are needed to conclude treatment recommendations.
Keywords: Collagenase, Enzymes, Fournier’s gangrene, Recombinant, Wound healing
Received: Norvember 27, 2023
Accepted: January 9, 2023
Published online: February 26, 2024
AboutOpen - ISSN 2465-2628 - www.aboutscience.eu/aboutopen
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Fournier’s gangrene is a fulminant infectious form of synergistic necrotizing fasciitis described by Jean-Alfred Fournier in 1883 (1) that involves the perirectal, perineal, and genital areas. Fournier’s gangrene affects all ages and both genders with a higher male prevalence (2).
Necrotizing fasciitis is an infection of the deep soft tissues triggered by a polymicrobial infection in the subcutaneous zone. The rapid spread of microorganism produces an obliterative endarteritis leading to a vascular thrombosis and gangrene (3).
Clinical features of Fournier’s gangrene include sudden pain, scrotal swelling and erythema, prostration, pallor, and pyrexia. Anorectal, genitourinary, and skin infections, together with local injuries, are the most common causes of this necrotizing fasciitis (3,4). Fournier’s gangrene patients also have some predisposing factors, such as diabetes mellitus as the most common, advancing age, prolonged hospitalization, malignancy, and alcoholism. Those factors decrease the host immunity and allow the entry of microorganisms into the zone (3).
The overall incidence of Fournier’s gangrene is 1.6 cases per 100,000 males. This pathology is rare in children and the incidence increases with age. Incidence peaked after age 50 years at 3.3 cases per 100,000 males (5).
Mortality rate ranges from 20% to 30% (6), this being a challenging surgery. Early recognition, extensive debridement of the zone, and aggressive antibiotic therapy continue to be the main approach for an adequate outcome, followed by other preventive measures such as good management and scarring of the skin.
The aim of this article is to present our protocol for wound healing with High pbserum, a novel enzymatic treatment, in a patient with Fournier’s gangrene.
Case description
A 75-year-old male patient presented with pain in the perianal region and, on defecation, general discomfort and fever. He was admitted to hospital on February 14, 2023 (day 0), due to the progression of symptomatology, being diagnosed with Fournier’s gangrene. The patient also had diabetes mellitus, hypertension, and obesity.
Patient swallowed a toothpick, which perforated the rectum and triggered sepsis and tissue necrosis in the perianal region. A multidisciplinary team including general and plastic surgery, infectious disease, and intensive care was involved in this case. First, we performed a surgical washing on the first day of admission to remove necrotic tissue from the perineal area. A second washing was done after 48 hours. On day 5, another surgical washing was performed, and the toothpick was found. Fourteen surgical washings were carried out in total and multiple flaps were required for perianal reconstruction.
A wound of 17 cm depth and a diameter of 8 × 5 cm in the left buttock with abundant exudate and fibrin remained despite all the washings. Patient also presented with a small lesion of size 1 × 1 cm from the drainage and multiple sutures from the flaps. The goal at this time was to close the left gluteal cavity and to prevent reinfections. On day 23 we proceeded with daily cleansings with Anasept® and placed biological dressings to protect the cavity and the regions from surgical wounds.
On day 36 the patient reported pain of 8 on a scale of 10 and we observed complications around the suture wounds. The flaps contracted, revealing a perianal seroma (2.5 cm depth with a diameter of 5 × 1 cm) and a cavity in the posterior scrotum (15 cm depth with a diameter of 3.5 × 1 cm). Advanced wound management was performed using dressings to absorb the fluid produced by the seroma and clean the scrotal and the left gluteal cavities. This was key to reduce the risk of infection and preparing the wound for future treatments. Furthermore, we treated the wounds caused by the contraction of the flaps and separation of the suture wounds on a daily basis using Cutimed sorbact®, Acticoat®, and Aquacell® dressings (shown in Fig. 1). We observed a decrease in the depth of the wounds and a good generation of granulation tissue.
On day 49 the wounds healed properly, complications were controlled, and there was good granulation tissue. At this point, and since the patient was diabetic, it was necessary to avoid the risk of reinfection; thus, it was necessary to accelerate the closure of the wounds. For this purpose, on day 54, it was decided to start treatment with High pbserum recombinant enzymes, which contain a high percentage of collagenase. Surgery was declined due to the patient’s characteristics. It was decided to irrigate the zone and not inject it due to the underlying Fournier’s gangrene and diabetes. The granulation tissue was irrigated with 6 cc of the dilution applied once every 3 weeks, using a syringe, ensuring good tissue impregnation (shown in Fig. 2). Concomitantly, collagen dressings were used to enhance the collagenase effect.

FIGURE 1 - The appearance of the whole zone with flaps and the surgical wounds on day 33.

FIGURE 2 - High pbserum application using a syringe included in the kit.
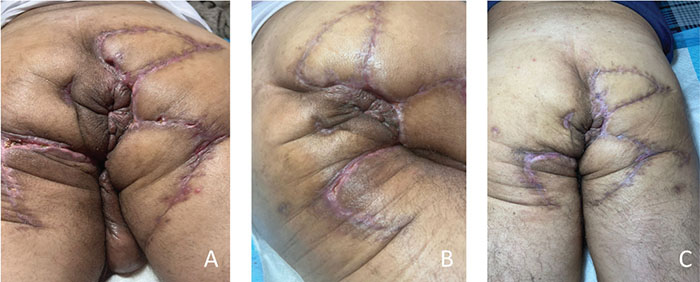
FIGURE 3 - High pbserum recombinant enzymes treatment: A) After 2 weeks of treatment; B) After 5.5 weeks of treatment; and C) After 11 weeks of treatment.
After the first week of application, epithelialization of the three affected areas was observed: the wound in the left buttock epithelialized completely, the wound in the scrotal area reduced its depth to 2.5 cm, and the wounds produced by the separation of the surgical edges became smaller and shallower. After the second week of application, the lesions in the left buttock closed completely and the scrotal lesion decreased in depth to 0.5 cm. After 1 month of treatment, most of the wounds healed adequately and without signs of infection (shown in Fig. 3).
Discussion
Fournier’s gangrene is a life-threatening infectious disease that requires early intervention due to its rapid and extensive progression into the fascia and skin, up to 3 cm per hour (7). The infection can affect the scrotum and penis, extending to the anterior abdominal wall, and even reaching the clavicle (8). To achieve a high rate of survival, it is necessary to apply a very aggressive debridement, which affects a vast dermal zone. Optimal wound healing is also required to prevent the new entrance and growth of pathogens.
When a skin wound occurs, a series of four phases are instantly initiated to repair the skin lesion (9): hemostasis, inflammation, proliferation, and remodeling. The extracellular matrix (ECM) remodeling is controlled by the metalloproteinases (MMPs).
Collagenases are a type of MMPs. Besides being responsible for degrading collagen, they have been found to facilitate dermal cell migration and reepithelialization, prevent apoptosis and inflammation (9). They regulate the balance between tissue synthesis and tissue degradation in any biological process requiring tissue reorganization, inflammation, and remodeling. It has been observed that the lack of the expression of collagenase in knockout mice leads to a delay in wound healing and to an increase in inflammation process in the zone (10). Collagenase stimulated keratinocyte cellular response in vitro and was superior to other treatments in granulation tissue formation, inflammation, reepithelialization, and time to wound closure in a micropig in vivo model (11).
High pbserum is an enzyme cocktail, composed of collagenase PB220 at the highest concentration, lipase PB500, and liase PB72K. It has already demonstrated its effect in providing a better recovery of the skin in scars (12). High pbserum is approved in Europe, Latin America, Middle East, and North Africa. Registration in the UK is still in process. In Europe, the presentation is 2.0 High pbserum, which contains 2 mL of hyaluronic acid as the enzyme vehicle. In America 1.5 High pbserum is commercialized, with 1.5 mL of hyaluronic acid. The enzyme proportions are the same. In our clinical practice High pbserum enzymes have been used in cases of acute burns, in chronic irrigations, and in other accelerated wound healing and scarring processes. In our personal experience, unpublished data, we have also used the enzymes in five patients with arterial wounds; however, the outcomes were not as expected. On the contrary, the results were excellent in other wound healing cases without vascular involvement. In this study we show how High pbserum improves and accelerates the wound healing process in a patient with Fournier’s gangrene, which has suffered from an extensive debridement. The results were seen after 1 week of the first application, achieving an 85% reduction in the depth of one of the cavities. After 1 month of treatment, most of the wounds were completely healed without adverse events. Our explanation for this patient is that collagenase in a high concentration has played a role in the second phase of wound healing, promoting fibroblast migration through the fibrin network, and reepithelialization by keratinocytes and epithelial stem cells. This action would lead to an improvement of the wound healing process in a shorter period of time.
In addition, the patient’s perception was that High pbserum enzymes made a difference in his treatment. According to the patient, he experienced a rapid improvement, with reported pain of 0 on a scale of 10 at the end of treatment, and never had pain or discomfort during its application.
Conclusions
In conclusion, High pbserum recombinant enzymes show better and rapid wound healing, particularly in the recovery of deep cavities generated by necrotizing fasciitis and in sutures raised after an extensive debridement. Further investigations and studies in wound healing are needed to conclude treatment recommendations.
Acknowledgments
The authors want to thank Dr. Benjamin Flickier and Dr. Gisella Herrera, the patient’s treating physicians, for their trust and their vital support during the process. They also want to thank the physiotherapist Mariela Marin Estrada for the care provided to the patient, and are grateful to Dr. Estefanía Hurtado Gómez for her work in writing the article.
Disclosure
Conflict of interest: EP has no conflict of interest to declare. JLB is an employee of the company Proteos Biotech and he receives a salary for this purpose.
Financial support: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contribution: EP contributed to the management and treatment of the patient, and the writing of the article. JLB contributed by providing the enzyme protocol and advising on the indications for the treatment and supervising the manuscript.
References
- 1. Fournier JA. Jean-Alfred Fournier 1832-1914. Gangrène foudroyante de la verge [overwhelming gangrene]. Sem Med 1883. Dis Colon Rectum. 1988 Dec;31(12):984-8. CrossRef PubMed
- 2. Hernández EH, Mosquera CG, De la Rosa V. Necrotizing fasciitis. Rev. Arch Méd Camagüey. 2015;19(6):654-664.
- 3. Laucks SS II. Fournier’s gangrene. Surg Clin North Am. 1994;74(6):1339-1352. CrossRef PubMed
- 4. Eke N. Fournier’s gangrene: a review of 1726 cases. Br J Surg. 2000;87(6):718-728. CrossRef PubMed
- 5. Sorensen MD, Krieger JN, Rivara FP, et al. Fournier’s Gangrene: population based epidemiology and outcomes. J Urol. 2009;181(5):2120-2126. CrossRef PubMed
- 6. Sparenborg JD, Brems JA, Wood AM, Hwang JJ, Venkatesan K. Fournier’s gangrene: a modern analysis of predictors of outcomes. Transl Androl Urol. 2019;8(4):374-378. CrossRef PubMed
- 7. Safioleas M, Stamatakos M, Mouzopoulos G, Diab A, Kontzoglou K, Papachristodoulou A. Fournier’s gangrene: exists and it is still lethal. Int Urol Nephrol. 2006;38(3-4):653-657. CrossRef PubMed
- 8. Saijo S, Kuramoto Y, Yoshinari M, Tagami H. Extremely extended Fournier’s gangrene. Dermatologica. 1990;181(3):228-232. CrossRef PubMed
- 9. Xue M, Le NT, Jackson CJ. Targeting matrix metalloproteases to improve cutaneous wound healing. Expert Opin Ther Targets. 2006;10(1):143-155. CrossRef PubMed
- 10. Gutiérrez-Fernández A, Inada M, Balbín M, et al. Increased inflammation delays wound healing in mice deficient in collagenase-2 (MMP-8). FASEB J. 2007;21(10):2580-2591. CrossRef PubMed
- 11. Riley KN, Herman IM. Collagenase promotes the cellular responses to injury and wound healing in vivo. J Burns Wounds. 2005;4(4):e8. PubMed
- 12. De Castro García MP, Muñoz Montaño JR. Multicenter clinical study to evaluate the efficacy and safety of hyaluronic acid and enzyme cocktail in scars. Dermatología CMQ. 2020;18(2):84-92. Online