 |
AboutOpen | 2023; 10: 119-123 ISSN 2465-2628 | DOI: 10.33393/ao.2023.2633 BRIEF REPORT |
 |
Vulvodynia: when a training program to increase muscle mass in the lower limbs does some good!
ABSTRACT
Vulvodynia is a chronic pain condition, without clearly identifiable and visible causes, associated with disability, sexual disfunction, and impaired quality of life. It is frequently under-reported and under-diagnosed, resulting in significant emotional burden. The pathophysiology of vulvodynia is complex and multidimensional. According to the integrated biopsychosocial model, main triggers of vulvodynia may be biological (infectious or inflammatory conditions inducing severe or prolonged nociceptive or neuropathic pain, genetic predisposition, hormonal imbalance), psychological (depression, anxiety), sexual (traumatic experiences, unhealthy intimate relationship), and social (adverse childhood experiences). The diagnostic approach is based on accurate medical history exploring the characteristics and timing of vulvar pain, as well as the presence of other chronic pain conditions that are often comorbid. Pelvic examination (vulvar and vaginal appearance, cotton swab test for vulvar sensitivity, pelvic floor evaluation) supports the diagnosis and excludes secondary vulvar pain disorders. Considering that pain is a complex human experience within a multidimensional frame, the best therapeutic strategy should be multidisciplinary encompassing different therapeutic targets. Pharmacological therapies have anti-nociceptive, neuromodulating, and anti-inflammatory purposes and include both topical and systemic treatments (antidepressants, anticonvulsants, hormonal creams). Physical therapy consists of pelvic floor physiotherapy, electrostimulation, and neuromodulation techniques, while cognitive behavioral therapy, psychosexual intervention, and neurobiological education address the psychosocial dimension of vulvodynia. If results are insufficient, a surgical approach is allowed. We present a clinical case linking amelioration of vulvodynia to a training program to increase muscle mass, especially in the lower limbs, in a girl reporting an eating disorder.
Keywords: Biopsychosocial factors, Central sensitization, Chronic pain, Muscle mass, Pelvic floor dysfunction, Training program, Vulvar pain, Vulvodynia
Received: July 10, 2023
Accepted: October 3, 2023
Published online: October 30, 2023
AboutOpen - ISSN 2465-2628 - www.aboutscience.eu/aboutopen
© 2023 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Vulvodynia is a chronic pain condition affecting women’s quality of life and sexual well-being. It is the most common cause of pain during sexual intercourse in premenopausal women (1).
Definition
The term vulvodynia was first employed in 2003 by the International Society for the Study of Vulvovaginal Disease, replacing the terms vestibulitis and vulvar dysesthesia. In 2015, a consensus meeting differentiated vulvodynia from vulvar pain secondary to specific diseases, such as infections, inflammatory conditions, cancer, trauma, neurological diseases, and genitourinary syndrome of menopause (2). According to this new terminology, vulvodynia is currently defined as vulvar pain lasting at least 3 months, without a clear identifiable cause, potentially presenting some associated factors (2). Therefore, even if vulvodynia is now considered a pain disease without clearly identifiable and visible causes, some of the following factors and conditions might be involved in its development, suggesting a shared pathophysiological process: comorbid pain syndromes, for instance, endometriosis, fibromyalgia, etc. (3) (Tab. I), psychosocial factors (4), genetics, inflammation, hormonal imbalances, and musculoskeletal and neurologic conditions (5).
| Chronic overlapping pain conditions: |
|---|
|
• Chronic fatigue syndrome • Chronic low back pain • Chronic migraine • Chronic tension-type headaches • Endometriosis • Fibromyalgia • Interstitial cystitis/painful bladder syndrome • Irritable bowel syndrome • Temporomandibular disorders |
Classification
Vulvodynia is described according to the distribution, onset, and timing of vulvar pain (6). Vulvodynia is localized when pain is limited to the vestibule and/or clitoris, while it is generalized if pain extends beyond the vestibule to the labia minora or majora, the upper legs, or the lower abdomen. Vulvodynia is provoked when pain is elicited by touch, such as during intercourse, tampon use, or tight clothing, while it is spontaneous if pain occurs without any provocation; a mixed condition is a combination of the two descriptors. The onset of vulvodynia is primary if pain occurs at the first provoking physical contact (i.e., first intercourse or tampon use), while secondary vulvodynia starts after a period without pain or painful activities. The temporal pattern of vulvodynia is described as persistent when pain is present in every situation since its onset, while it is intermittent when pain is not present at all times or every time provoked. Vulvodynia is immediate when pain starts instantly when provoked, otherwise it is delayed when pain starts after provocation or persists for minutes, hours, or days. The most common subtype of vulvodynia is localized provoked vestibulodynia (6).
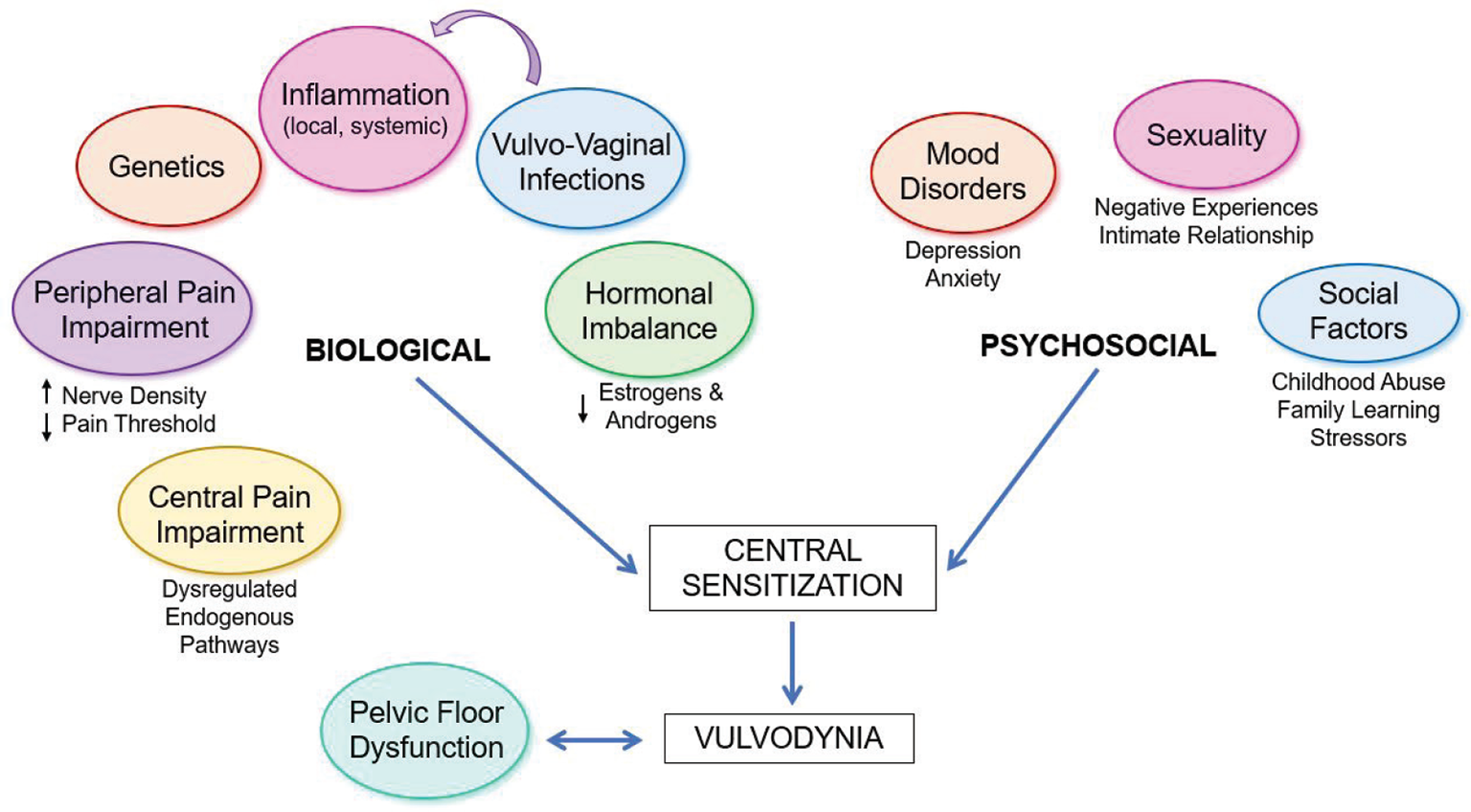
Fig. 1 - Pathophysiology of vulvodynia.
Epidemiology
Vulvodynia is an under-reported and under-diagnosed condition. Women face barriers to consult for help and report feeling stigmatized by health-care professionals (7). Indeed, only 60% of women with chronic vulvar pain ask for a treatment and approximately half of them never receive a diagnosis (8), confirming vulvodynia as a neglected condition whose prevalence is difficult to establish (5). Global epidemiological studies are lacking, nonetheless results from national studies report a lifetime prevalence of vulvodynia of 16% in the United States (9) and Portugal (10), 13% in Spain (11), 9%-10% in the United Kingdom (12), and less than 1% in Nepal (13). Vulvodynia characterizes women of all ages, including postmenopausal women, but the incidence is highest among younger women (5).
Pathophysiology
The pathophysiology of vulvodynia is multifaceted and currently attributed to an integrated model of biopsychosocial factors promoting a central sensitization process (1) (Fig. 1). History of dyspareunia or other urogenital symptoms, often without a documented etiology, is considered a risk factor that may anticipate the subsequent development of vulvodynia (14).
Neurobiological studies report an increased nerve fiber density in the vulvar vestibule (15), a lower pain threshold in the urogenital area (5), an increased central pain sensitivity (16), and a dysregulation of endogenous central pain modulatory systems (17) in women suffering from vulvodynia. A genetic predisposition to vulvodynia is suggested, involving gene polymorphisms that could promote an exaggerated inflammatory response, increase the risk of vulvar infections, modify hormonal susceptibility to contraceptives, and alter the endogenous modulation of pain (1,18). Even if literature is controversial, inflammatory mechanisms such as increased vestibular mast cells and reduced systemic natural killer cells may cause a central sensitization that persists after the resolution of acute vulvar infections or trauma (19). Hormonal imbalances, namely low estrogenic and androgenic levels due to reproductive conditions (lactation, hypothalamic amenorrhea, postmenopause) or hormonal contraceptives may alter urogenital innervation and vestibular trophism (20). Pelvic floor muscle dysfunctions, including hypertonicity, poor muscle control, hypersensitivity, and altered contractility (21), are associated with vulvodynia, but whether they are related to the pathogenesis of vulvodynia or are the result of pain remains unclear (5).
As pain is a complex experience, the psychosocial dimension is involved alongside the biological factors in determining the sensitivity to pain (1). Studies show that mood disorders, such as depression, anxiety, pain catastrophizing, and posttraumatic stress disorder, are associated with vulvodynia (4). Childhood maltreatment (22), stressors, and traumatic sexual experiences are other risk factors, while positive relationship factors such as intimacy, sexual communication, and affection have a protective effect (5).
Diagnosis
The diagnostic approach to vulvodynia requires a detailed medical history, exploring the characteristics and timing of pain, as well as previous urogynecological diagnosis and treatments (5). Women should be asked not only for vulvar pain but also for other symptom descriptors such as discomfort, irritation, itching, stabbing, and even sharp or pin sensations (5). The diagnosis is supported by the presence of comorbid chronic overlapping pain conditions (Tab. I), psychological symptoms, and relationship factors (3,4,5). Even the emotional and sexual burden should be discussed (5).
Pelvic examination is fundamental to support the diagnosis and differentiate vulvodynia from other vulvar conditions such as vulvovaginal infections, inflammatory dermatological disorders, vulvar cancer, and genitourinary syndrome of menopause (2,5). The appearance of external genitalia is first evaluated, followed by the cotton swab test to assess sensitivity at the vestibule, labia, and hymenal remnants (23). If possible, gentle vaginal examinations with a speculum allow the assessment of vaginal wall and vaginal secretions, collecting specimens of any vaginal discharges if needed (23). Pelvic floor muscle tenderness should be evaluated as well (24).
Management
The treatment of vulvodynia requires a multidimensional and tailored approach (1,25). According to some authors, a three-step treatment may be considered (26). The first step includes topical and oral medications, vulvar care recommendations, adequate diet, pelvic floor physiotherapy, and cognitive behavioral and psychosexual therapy. The second step includes radiofrequency, neuromodulation, and neurostimulation techniques. The third step is the surgical approach, such as vestibulectomy. However, evidence on the efficacy of these treatments is insufficient, and placebo has been proven as being effective as any medication for vulvodynia (27). According to numerous evidence-based guidelines, patients’ education in neurobiology is an emerging strategy in the management of chronic pain, since a better understanding of their condition allows them to change their maladaptive perception of pain (1,28). Table II summarizes the main evidence-based treatments for vulvodynia.
| Class of treatment | |
|---|---|
| Education | Avoiding irritants, promoting urogynecological health, neurobiological knowledge |
| Pharmacologic therapy
(anti-nociceptive, neuromodulating, anti-inflammatory purposes) |
Topical creams: • Lidocaine 2-5% • Amitriptyline 2% (vaginal) • Gabapentin • Diazepam (vaginal) • Corticosteroids • Estrogen • Combined estrogen and testosterone Injectables: • Botulinum toxin A • Enoxaparin (future studies needed) • Anesthetic agents for multilevel nerve blockade Tricyclic antidepressants: • Amitriptyline Anticonvulsants: • Gabapentin • Pregabalin • Lamotrigine Future immune-targeting therapies |
| Physical therapy | Pelvic floor physical therapy (manual, dilators, and insertion techniques)
Transcutaneous electrical nerve stimulation (TENS) Transcranial direct-current stimulation Electromyographic (EMG) biofeedback Radiofrequency |
| Psychosocial interventions | Cognitive behavioral therapy
Pain management Sex therapy and psychoeducation |
| Surgery | Vestibulectomy (full or posterior) |
Clinical case
A training program was designed for a 24-year-old girl, who carried it out for a period of 16 weeks between September 2022 and December 2022.
The subject reported her clinical history, specifying that she had already begun to feel “abnormal down there” at the age of 18, but she has been formally diagnosed with vulvodynia only at the age of 22. This girl could not afford specific advised treatments such as transcutaneous electrical nerve stimulation (TENS) due to time constraints and economic difficulties during COVID pandemic and waited for seeking other professional help. Her personal history was characterized by suffering from an eating disorder. Although in September 2022 the situation was not as critical as it was when she was 18, the girl still reported some dysfunctional habits. She was aware that having excessive control over food quantity and quality was an unfair behavior leading to some episodes of binge eating, immediately followed by fasting. Indeed, guilt and fear of gaining excess weight were constant companions of this girl. In 2021, she followed a well-balanced diet with nutritional supervision and was able to gain a little weight; however, she then lost weight again. Before starting the training program, she weighed 43.5 kg and had a body mass index (BMI) of 16.5 kg/m2 (severely underweight).
The main goal of the training program was to increase muscle mass, especially in the lower limbs. For this reason, the weekly program included three individual sessions per week of about 60-75 minutes, two mainly for lower limbs and the third one for the upper body, with a work for the abdominals at the end of the session in each workout. The choice of the exercises and the methodology were crucial. The decision was made to avoid exercises with few repetitions and high intensity, but it was proposed to remain always in a range of repetitions between 8 and 15. In addition, in the warm-up (treadmill for 15 minutes), the girl was told to maintain a speed that allowed her to walk. As for the abdominals, she exercised always in isometry (plank and side plank) to avoid more risky contraction movements.
This training program had a true positive emotional impact. The girl showed resourcefulness and was highly motivated to carry out the various sessions from the start, and especially after the first physical changes that significantly improved her self-esteem.
The program was positive for the girl in several aspects. First, she gained weight from a starting value of 43.5 kg to a final value of 48 kg (BMI 18.4 kg/m2). In addition, she improved her psychological well-being, food habits, and general physical wellness. Lastly, her ob/gyn confirmed a significant improvement of vulvodynia symptoms and less pelvic floor abnormalities (trigger points and contraction) in subsequent follow-up.
In conclusion, the present clinical case suggests that a gap should be filled in the literature about the relationship between vulvodynia and physical activity, especially when eating disorders and other body image issues can be documented. However, our experience is limited to the outcome of only one patient following a specific training program. Taking into account that vulvodynia is the result of various trigger factors potentially overlapping with weight and lifestyle habits according to an individual variance, further clinical observations are needed.
Disclosures
Conflict of interest: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contribution: All authors contributed equally to this manuscript.
References
- 1. Torres-Cueco R, Nohales-Alfonso F. Vulvodynia—it is time to accept a new understanding from a neurobiological perspective. Int J Environ Res Public Health. 2021;18(12):6639. CrossRef PubMed
- 2. Bornstein J, Goldstein AT, Stockdale CK, et al; Consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal Disease (ISSVD), the International Society for the Study of Women’s Sexual Health (ISSWSH), and the International Pelvic Pain Society (IPPS). 2015 ISSVD, ISSWSH and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. Obstet Gynecol. 2016;127(4):745-751. CrossRef PubMed
- 3. Reed BD, Harlow SD, Sen A, Edwards RM, Chen D, Haefner HK. Relationship between vulvodynia and chronic comorbid pain conditions. Obstet Gynecol. 2012;120(1):145-151. CrossRef PubMed
- 4. Khandker M, Brady SS, Vitonis AF, Maclehose RF, Stewart EG, Harlow BL. The influence of depression and anxiety on risk of adult onset vulvodynia. J Womens Health (Larchmt). 2011;20(10):1445-1451. CrossRef PubMed
- 5. Bergeron S, Reed BD, Wesselmann U, Bohm-Starke N. Vulvodynia. Nat Rev Dis Primers. 2020;6(1):36. CrossRef PubMed
- 6. Bornstein J, Preti M, Simon JA, et al; International Society for the Study of Vulvovaginal Disease (ISSVD), the International Society for the Study of Womenʼs Sexual Health (ISSWSH), and the International Pelvic Pain Society (IPPS). Descriptors of vulvodynia: a multisocietal definition consensus (International Society for the Study of Vulvovaginal Disease, the International Society for the Study of Women Sexual Health, and the International Pelvic Pain Society). J Low Genit Tract Dis. 2019;23(2):161-163. CrossRef PubMed
- 7. Nguyen RH, Turner RM, Rydell SA, Maclehose RF, Harlow BL. Perceived stereotyping and seeking care for chronic vulvar pain. Pain Med. 2013;14(10):1461-1467. CrossRef PubMed
- 8. Harlow BL, Kunitz CG, Nguyen RH, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014;210(1):40.e1-40.e8. CrossRef PubMed
- 9. Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc (1972). 2003;58(2):82-88. PubMed
- 10. Vieira-Baptista P, Lima-Silva J, Cavaco-Gomes J, Beires J. Prevalence of vulvodynia and risk factors for the condition in Portugal. Int J Gynaecol Obstet. 2014;127(3):283-287. CrossRef PubMed
- 11. Gómez I, Coronado PJ, Martín CM, Alonso R, Guisasola-Campa FJ. Study on the prevalence and factors associated to vulvodynia in Spain. Eur J Obstet Gynecol Reprod Biol. 2019;240:121-124. CrossRef PubMed
- 12. Mitchell KR, Mercer CH, Ploubidis GB, et al. Sexual function in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet. 2013;382(9907):1817-1829. CrossRef PubMed
- 13. Pathak D, Agrawal S, Dhali TK. Prevalences of and risk factors for vulvar diseases in Nepal: a hospital-based study. Int J Dermatol. 2011;50(2):161-167. CrossRef PubMed
- 14. Reed BD, Payne CM, Harlow SD, Legocki LJ, Haefner HK, Sen A. Urogenital symptoms and pain history as precursors of vulvodynia: a longitudinal study. J Womens Health (Larchmt). 2012;21(11):1139-1143. CrossRef PubMed
- 15. Tympanidis P, Terenghi G, Dowd P. Increased innervation of the vulval vestibule in patients with vulvodynia. Br J Dermatol. 2003;148(5):1021-1027. CrossRef PubMed
- 16. Giesecke J, Reed BD, Haefner HK, Giesecke T, Clauw DJ, Gracely RH. Quantitative sensory testing in vulvodynia patients and increased peripheral pressure pain sensitivity. Obstet Gynecol. 2004;104(1):126-133. CrossRef PubMed
- 17. Hampson JP, Reed BD, Clauw DJ, et al. Augmented central pain processing in vulvodynia. J Pain. 2013;14(6):579-589. CrossRef PubMed
- 18. Lev-Sagie A, Prus D, Linhares IM, Lavy Y, Ledger WJ, Witkin SS. Polymorphism in a gene coding for the inflammasome component NALP3 and recurrent vulvovaginal candidiasis in women with vulvar vestibulitis syndrome. Am J Obstet Gynecol. 2009;200(3):303.e1-303.e6. CrossRef PubMed
- 19. Chalmers KJ, Madden VJ, Hutchinson MR, Moseley GL. Local and systemic inflammation in localized, provoked vestibulodynia: a systematic review. Obstet Gynecol. 2016;128(2):337-347. CrossRef PubMed
- 20. Ting AY, Blacklock AD, Smith PG. Estrogen regulates vaginal sensory and autonomic nerve density in the rat. Biol Reprod. 2004;71(4):1397-1404. CrossRef PubMed
- 21. Morin M, Binik YM, Bourbonnais D, Khalifé S, Ouellet S, Bergeron S. Heightened pelvic floor muscle tone and altered contractility in women with provoked vestibulodynia. J Sex Med. 2017;14(4):592-600. CrossRef PubMed
- 22. Khandker M, Brady SS, Stewart EG, Harlow BL. Is chronic stress during childhood associated with adult-onset vulvodynia? J Womens Health (Larchmt). 2014;23(8):649-656. CrossRef PubMed
- 23. Stenson AL. Vulvodynia: diagnosis and management. Obstet Gynecol Clin North Am. 2017;44(3):493-508. CrossRef PubMed
- 24. Meister MR, Sutcliffe S, Ghetti C, et al. Development of a standardized, reproducible screening examination for assessment of pelvic floor myofascial pain. Am J Obstet Gynecol. 2019;220(3):255.e1-255.e9. CrossRef PubMed
- 25. Santangelo G, Ruggiero G, Murina F, et al. Vulvodynia: a practical guide in treatment strategies. Int J Gynaecol Obstet. 2023;ijgo.14815. CrossRef PubMed
- 26. De Andres J, Sanchis-Lopez N, Asensio-Samper JM, et al. Vulvodynia—an evidence-based literature review and proposed treatment algorithm. Pain Pract. 2016;16(2):204-236. CrossRef PubMed
- 27. Miranda Varella Pereira G, Soriano Marcolino M, Silveira Nogueira Reis Z, Vale de Castro Monteiro M. A systematic review of drug treatment of vulvodynia: evidence of a strong placebo effect. BJOG. 2018;125(10):1216-1224. CrossRef PubMed
- 28. Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):1140.e1-1140.e22. CrossRef PubMed