 |
AboutOpen | 2024; 11: 1-3 ISSN 2465-2628 | DOI: 10.33393/ao.2024.2611 CASE REPORT |
 |
A case of exaggerated placental site treated with hysteroscopy
Abstract
Exaggerated placental site (EPS) is a benign lesion that can occur in association with term pregnancy, ectopic pregnancy, molar pregnancy, intrauterine fetal death or miscarriage. The characteristics of EPS are described in several case reports and have been reported after major surgery such as hysterectomy. We describe the hysteroscopic characteristic of EPS associated with a spontaneous miscarriage. Hysteroscopic inspection of the uterine cavity revealed copious tissue with increased vascularization without signs of invasion. No cleavage was visualized between material and myometrium could be established during the resection procedure. 40 days after hysteroscopy the patient became pregnant. The pregnancy proceeded without complications and during the cesarean section no residual placenta-related abnormal site appearance was noted on inspection of the uterine wall. The hysteroscopic treatment could be considered feasible to preserve future fertility in young women in cases of suspect non-malignant trophoblastic disease.
Keywords: Fertility, Hysteroscopy, Miscarriage, Trophoblast
Received: May 30, 2023
Accepted: December 13, 2023
Published online: January 11, 2024
AboutOpen - ISSN 2465-2628 - www.aboutscience.eu/aboutopen
© 2024 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Introduction
Gestational trophoblastic disease (GTD) includes a heterogeneous group of lesions arising from an abnormal proliferation of the placental trophoblast neoplasm. It is divided into benign non-neoplastic trophoblastic lesions and gestational trophoblastic neoplasms. Exaggerated placental site (EPS) is a benign lesion characterized by exuberant infiltration of the myometrium by intermediate trophoblasts at the implantation site. EPS can occur in association with term pregnancy, ectopic pregnancy, molar pregnancy, intrauterine fetal death or miscarriage (1). The surgical treatment of miscarriage is prevalently dilation and curettage (D&C) but, in selected cases, hysteroscopic uterine evacuation of early pregnancy loss using tissue removal devices seems to be a safe and feasible procedure (2).
There have been only case report describing the presence of EPS but the use of hysteroscopic approach and characteristics has not yet been reported. We present a case of incidentally observed EPS in association with spontaneous miscarriage, accidentally discovered and subsequently treated with hysteroscopy.
Case report description
A 38-year-old woman, in good health, with a previous elective cesarean section for breech presentation, presented to our department in September 2020 with a diagnosis of miscarriage of 9 weeks gestation. Transvaginal ultrasound showed an intrauterine gestational sac with a visible embryo without cardiac activity (crown rump length [CRL] corresponding to 9 weeks of pregnancy). In consideration of the patient’s request for cytogenic examination we decided to employ the use of the hysteroscope to enhance visualization for sampling after informed counselling. After 10 days of ultrasound diagnosis the patient underwent the hysteroscopic procedure in an inpatient setting under conscious sedation (Fig. 1). Hysteroscopy was performed with a 26 Fr resectoscope supplied with a 4 mm bipolar loop electrode connected to Olympus Versapoint Generator. Saline solution was used as distension medium. Surgery was completed in 60 minutes. Hysteroscopic inspection confirmed copious intracavitary material and no cleavage could be established between the material and myometrium. At the end of the procedure, the subendometrial glands were left intact to preserve the integrity of endometrium and the pregnancy rate. At the end of surgery, antiadhesive gel was applied to prevent adhesions; 120 g of endocavity tissue was collected. The estimated blood loss was 500 mL and the hysteroscopic fluid deficit was negative (1,400 mL). The patient was discharged on the first postoperative day.
The removed tissue was sent for histopathological examination. The histopathological exam described placental villi with cytotrophoblastic coating, and the presence of syncytial trophoblastic penetration into the myometrium suggested diagnosis of EPS. The pathologist suggests monitoring of human chorionic gonadotropin (hCG) due to suspected trophoblastic disease. The cytogenetic exam showed a trisomy 15.
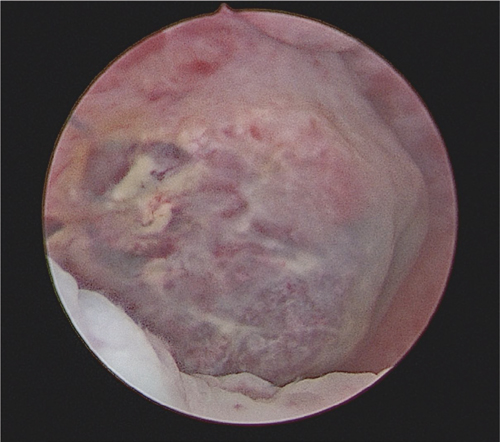
Fig. 1 - Hysteroscopic view of EPS. EPS = exaggerated placental site.
Forty days after hysteroscopy, the patient had an hCG blood level of 1,258 mU/mL. In transvaginal ultrasound we found an intrauterine gestational sac with an embryo with cardiac activity; CRL measurement was 3.1 mm. The pregnancy proceeded regularly. The patient underwent an elective cesarean section 39 weeks due to the history of previous cesarean section. The baby was appropriate for gestational age with a normal pH after delivery. No placental afterbirth complications were noted. The histopathologic exam of placenta was normal.
Conclusion
EPS is a non-neoplastic trophoblastic lesion characterized by exuberant infiltration of the myometrium by trophoblasts at the implantation site. This lesion was first defined as syncytial endometritis, but the term ‘Exaggerated Placental Site’ is now commonly used. EPS may develop secondary to a normal pregnancy, miscarriage, cervical pregnancy or hydatidiform mole (1). The several reports describe the clinical course of EPS, including ultrasound and magnetic resonance imaging (MRI) findings or histopathological characteristics (3), but this case report is the first description of hysteroscopic findings of EPS.
In the present case we performed hysteroscopic surgery after miscarriage with detection of an unusual intracavitary topography and presentation of significant amount of gestational tissue. It has been shown that hysteroscopic approach is an effective routine and safe procedure based on the tissue removal inside the uterus; Cholkeri-Singh et al (4) have shown that the detection of fetal chromosomes obtained from direct hysteroembryoscopic biopsies resulted in more accurate karyotyping with lower maternal cell contamination than those obtained from curettage material. Hysteroscopic evacuation of the uterine cavity may reduce the D&C complication such as uterine perforation and endometrial damage in order to preserve future fertility.
By performing the procedure under direct visualization focusing on the implantation site, we can obtain precise sampling of trophoblastic tissue. On hysteroscopic view the uterine wall demonstrates trophoblastic tissue present in all uterine wall with increased vascularization. No invasive signs were noted and during the hysteroscopic resection no cleavage was found between the material and myometrium. During surgery there was plentiful bleeding but without the need for further intervention of drugs. In order to preserve fertility, the subendometrial glands were left intact. We use hyaluronic acid gel to prevent intrauterine adhesion formation after complete evacuation of the uterine cavity. In the case report the presence of hCG 40 days after hysteroscopy alerted us to the possible presence of a malignant trophoblastic lesion as placental site trophoblastic tumors (PSTT) but elevated hCG was due to an early gestation.
Cytogenetic analysis showed trisomy 15. In literature we found other reports where GTD was associated with alteration of number of chromosomes. Trisomy 8, 13 or 21 was described with GTD (5,6). In our case the pregnancy occurred after the hysteroscopy treatment and had a regular course. We were on alert for the possibility of bleeding after placenta delivery according to reports in literature. In fact EPS could lead to severe postpartum hemorrhage also with necessity of hysterectomy (1,7). The cesarean section of our patient occurred without complications, confirming a complete removal of EPS with previous hysteroscopic treatment.
EPS is a rare trophoblastic lesion but in the suspicion of non-malignant trophoblastic disease, hysteroscopic treatment should be considered.
Hysteroscopy seems to be a safe and feasible procedure and could be considered in selected cases, such as in young women with desire of fertility preservation.
Disclosure
Conflict of interest: The authors have no financial or proprietary interest in the subject matter of this article.
Financial support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Takebayashi A, Kimura F, Yamanaka A, et al. Exaggerated placental site, consisting of implantation site intermediate trophoblasts, causes massive postpartum uterine hemorrhage: case report and literature review. Tohoku J Exp Med. 2014 Sep;234(1):77-82. CrossRef PubMed
- 2. Catena U, D’Ippolito S, Campolo F, Dinoi G, Lanzone A, Scambia G. Hysteroembryoscopy and hysteroscopic uterine evacuation of early pregnancy loss: a feasible procedure in selected cases. Facts Views Vis ObGyn. 2022;14(2):193-197. CrossRef PubMed
- 3. Hasegawa T, Matsui K, Yamakawa Y, Ota S, Tateno M, Saito S. Exaggerated placental site reaction following an elective abortion. J Obstet Gynaecol Res. 2008;34(4 Pt 2):609-612. CrossRef PubMed
- 4. Cholkeri-Singh A, Zamfirova I, Miller CE. Increased fetal chromosome detection with the use of operative hysteroscopy during evacuation of products of conception for diagnosed miscarriage. J Minim Invasive Gynecol. 2020;27(1):160-165. CrossRef PubMed
- 5. Jauniaux E, Halder A, Partington C. A case of partial mole associated with trisomy 13. Ultrasound Obstet Gynecol. 1998 Jan;11(1):62-64. CrossRef PubMed
- 6. Geisler JP, Mernitz CS, Hiett AK, Geisler HE, Cudahy TJ. Trisomy 21 fetus co-existent with a partial molar pregnancy: case report. Clin Exp Obstet Gynecol. 1999;26(3-4):149-150. PubMed
- 7. Liu G, Yuan B, Wang Y. Exaggerated placental site leading to postpartum hemorrhage: a case report. J Reprod Med. 2013 Sep-Oct;58(9-10):448-450. PubMed