 |
AboutOpen | 2022; 9: 11-14 ISSN 2465-2628 | DOI: 10.33393/ao.2022.2360 REVIEW |
 |
How to insert a PICC: practical tips for the intensive care physician
ABSTRACT
Peripherally inserted central catheters (PICCs) are central vascular access devices inserted via deep veins of the arm, also useful in critical care settings. The purpose of this article is to offer to a critical care clinician with good skills in central venous catheterization, but who has limited experience on PICC catheters, the basic information on how the procedure is performed and how to minimize the risks of complications or failure of the maneuver.
The main technical steps and the main precautions to be taken during PICC placement will be analyzed, with reference to the differences compared to central catheterization. Specifically, the pre-procedural phase and the intraprocedural main steps of the maneuver will be analyzed.
A dedicated Vascular Access Team is considered useful and desirable by the current literature, but when the use of the PICC proves useful or even mandatory, the intensive care physician skilled in central venous catheters can transfer skills from central to peripheral catheterization.
Keywords: CICC, Intensive care, Occasional, PICC
Received: December 4, 2021
Accepted: March 21, 2022
Published online: April 11, 2022
Indirizzo per la corrispondenza:
Stefano Elli
PICC Team, Emergency Department
ASST Monza, San Gerardo Hospital
Via Pergolesi 33, Monza (MB) - Italy
s.elli@asst-monza.it
AboutOpen - ISSN 2465-2628 - www.aboutscience.eu/aboutopen
© 2022 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Background
Peripherally inserted central catheters (PICCs) are central vascular access devices inserted via deep veins of the arm. These are playing an increasing role not only in hospital and home care but also in critical care settings (1).
PICCs represent an attractive alternative to centrally inserted central catheters (CICCs) due to the lower incidence of intraprocedural complications and the lower risk of infection (2). In critical care setting the PICC offers, compared to the CICC with exit site at the neck, several advantages, without risk of pneumothorax during insertion and a greater distance between the exit site and oropharyngeal secretions or tracheostomy. It can also represent an interesting option in the management of patients undergoing noninvasive ventilation with mask or continuous positive airway pressure helmet, due to the possibility of insertion in a semi-seated or prone patient (3).
In most institutions PICCs are inserted by dedicated teams, including physicians and nurses with specific skills, and the procedure is considered nonurgent and elective (1,4-6). Still a critical care clinician may be faced with the need to position a PICC, without the possibility to rely on the dedicated team, due to the lack of time or unavailability of the dedicated team.
The purpose of this review is offering to a critical care clinician with good skills in central venous catheterization, as “PICC occasional inserter”, the basic informations necessary on how the procedure is performed, minimizing the risks of complications or failure of the maneuver.
Description of the procedure
The main technical steps and the main precautions to be taken during PICC placement will be analyzed, with reference to the differences compared to CICC placement. Specifically, the main pre-procedural phase and the intraprocedural steps of the maneuver will be described.
Choice of the vein and the exit site
The critical care clinician skilled in CICC insertion, who usually works on the internal jugular or subclavian veins, is familiar with the risks and issues due to the puncture of a vein which, despite being of medium-large caliber and with significant blood flow, is very close to noble structures such as pleura or carotid and subclavian artery. The choice of the catheter’s caliber depends on clinical needs and the central vein is usually able to accommodate catheters of large calibers, at least in the short/medium term.
On the contrary, the veins of the arm used for PICCs (basilic, brachial or cephalic veins) do not present important risks during the puncture maneuver but are much more sensitive to trauma of the vascular wall and to the presence of the catheter itself. Compliance with certain precautions is therefore necessary to reduce the risk of complications (7).
The path of the PICC in the venous system presents several convolutions and potential obstacles to the correct advancement of the catheter. The dimensions of the vessels involved are not always constant and any narrowing, upstream of the puncture, could represent an additional source of risk.
A systematic ultrasound evaluation of the vessels, in the arm and thorax, should be performed to identify those that may be appropriate for the procedure (8). The technique most often used is called Rapid Peripheral Vein Assessment (RaPeVA), which allows the clinician to quickly and completely assess the available peripheral vascular system and identify the position of the median nerve (7).
The puncture site is usually chosen according to the ZIM™ method (9), in which the arm is divided into three portions of equal size and the exit site must be located in the central portion, called the Green Zone. The distal portion (Red Zone) is more subject to forearm movements causing trauma, while the proximal portion, near the axillary cavity (Yellow Zone), is more exposed to infectious risk due to the greater physiological bacterial colonization and the difficulty to manage the catheter.
During RaPeVA, once the target vein has been identified, it is advisable to measure its diameter at its smallest point, starting from the puncture site and along the entire visualizable proximal portion. The caliber of the catheter must occupy at a maximum one-third of the caliber of the vein (7): although some literature reports a catheter/vein ratio of 45% (1,10), a ratio of 33% still appears safer. For example, in a 4 mm vein it is advisable to insert a catheter equal to or smaller than 4 French; in a 5 mm vein it is advisable to insert a catheter equal to or smaller than 5 French and so on.
Catheter length assessment
Due to the interindividual patient variability, it is useful to assess the length of the PICC prior to insertion, to optimize the out-of-skin tract and simplify the management. A simple method, based on surface landmarks, consists in measuring the distance from the exit site to the ipsilateral clavicle–sternal articulation, adding to this distance 10 cm if the access is from the right arm or 15 cm if the access is from the left arm. This technique slightly overestimates the correct distance but it allows to adjust the length of the PICC with some precision (11).
Maximum sterile barrier precautions
For PICC insertion, as for all vascular access devices with an expected indwelling time of more than 48/72 hours, maximum sterile barrier precautions are mandatory (1,5). Emergency conditions do not justify the avoidance of such measures and in emergency conditions other types of vascular access devices are more suitable.
Ultrasound-guided venipuncture
Compared to CICC insertion with the direct Seldinger technique, PICC requires the critical care clinician to change the approach to ultrasound-guided venipuncture.
The modern micro-introduction systems, contained in the PICC kits, are based on a 23G needle and 0.018 nitinol guide wire. Such a fine needle is more prone to accidental and involuntary movements during the syringe disconnection maneuver after puncture.
For this reason, a viable option is to prick with the needle without a syringe connected and primarily use ultrasound vision instead of looking for blood reflux (Fig. 1).
PICC insertion
PICC insertion is based on the modified Seldinger technique. The catheter is inserted into the vein through a peel-away micro-introducer and not, as it happens during CICC insertion, over the guide wire.
During PICC insertion it is recommended to follow the progression of the catheter through the axillary vein in its thoracic portion by ultrasound and to rule out, again by ultrasound, the catheter migration in the internal jugular vein. The rotation of the patient’s head toward the operator helps the correct progression of the catheter: this position partially occludes the internal jugular vein and facilitates the advancement toward the anonymous vein. For the same purpose, alternatively, it is also possible to manually compress the internal jugular vein with the ultrasound probe (7). In case of difficulty, it may be useful to extend the patient’s arm cranially, to render more linear the vessel portion of interest.
The use of the micro-introducer, during PICC insertion, offers a sensitivity to the operator entirely different from the one which is well known to those skilled in CICC insertion. While to advance the CICC a fair amount of force is necessary to overcome the resistance of the catheter on the skin and subcutaneous tissues, the sliding of the PICC through the introducer is, instead, totally free of friction between the micro-introducer and catheter. In order to detect and manage any resistance to PICC advancement, transmitted from the tip of the catheter to the operator’s hand, it is therefore important to advance the catheter slowly and regularly, holding it very gently between the thumb and forefinger of the dominant hand. This allows to perceive the presence of any anatomical obstacle in the vascular system and overcome these by tactile sensations.
Tip location
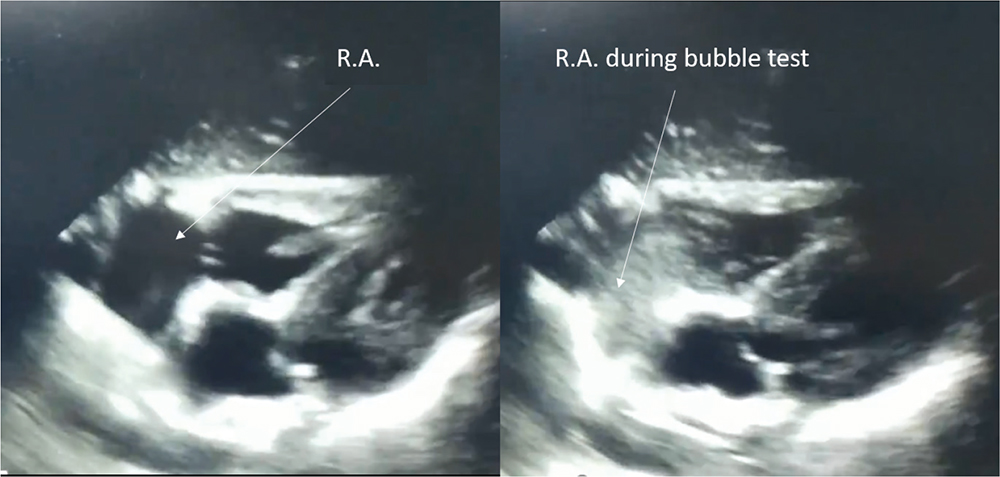
The technique still considered the most reliable and cost-effective for verifying the position of the PICC tip (tip location) at the cavoatrial junction is the intracavitary electrocardiogram (1,7,8,12). For the critical care physician, generally well skilled in ultrasound diagnostics, the use of transthoracic echocardioscopy for the PICC tip location may be faster and easier (1,8). A four-chamber cardiac scan allows to visualize the right atrium, the infusion via PICC of a few milliliters of normal saline mixed with a small amount of air allows to measure the delay between injection and visualization of the fluid in the right atrium (bubble test). Although in the literature a maximum time of up to 2 seconds is reported, a delay of 1 second or less is considered a reliable indicator of the correct positioning of the tip (8,13) (Fig. 2).

The intraprocedural tip location, thanks to the almost total absence of risks for major complications associated with venipuncture, makes the use of radiological diagnostics unnecessary, allowing immediate use of the catheter (1,14).
Catheter securement
One of the main aspects of PICC placement is correct catheter securement. As recommended in the literature for the last 20 years, a sutureless device has to be used for infection risk reduction (1,5,7). In the last decade, a new device has shown remarkable effectiveness in anchoring the catheter to the skin. It is the subcutaneous anchoring system (SAS), particularly also suitable for difficult to manage exit sites, such as the neck, and in patients with high risk of accidental dislodgement (15,16).
At the end of the procedure, the application of cyanoacrylate glue to the exit site is recommended prior to the application of the dressing. Cyanoacrylate glue is useful for: hemostasis in the exit site, stabilization of the catheter and protection against bacterial migration through the exit site (17).
The limit of this work is that it is not exhaustive of all the good practices necessary for PICC insertion, but limits itself to providing some ideas on the most important topics about the maneuver, which can help in preventing or reducing the event of failure or the onset of complications.
Conclusion
A dedicated Vascular Access Team is considered useful and desirable by the current literature (1,4-6). However, in some situations this cannot be guaranteed or immediately available. For this reason, a critical care physician may need to insert a PICC occasionally, to meet therapeutic needs that cannot be foreseen and cannot be postponed. When the use of the PICC proves useful or even mandatory, the critical care physician, skilled in central venous catheters, can transfer skills from central to peripheral catheterization.
Disclosures
Conflict of interest statement: The authors declare no conflict of interest.
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1. Gorski LA, Hadaway L, Hagle ME, et al. Infusion therapy standards of practice. 8th ed. J Infus Nurs. 2021 Jan-Feb 01;44(1S Suppl 1):S1-S224. CrossRef PubMed
- 2. Chopra V, O’Horo JC, Rogers MA, Maki DG, Safdar N. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2013;34(9):908-918. CrossRef PubMed
- 3. Pittiruti M, Pinelli F; GAVeCeLT Working Group for Vascular Access in COVID-19. Recommendations for the use of vascular access in the COVID-19 patients: an Italian perspective. Crit Care. 2020;24(1):269. CrossRef PubMed
- 4. Marschall J, Mermel LA, Fakih M, et al; Society for Healthcare Epidemiology of America. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(7):753-771. CrossRef PubMed
- 5. O’Grady NP, Alexander M, Burns LA, et al; Healthcare Infection Control Practices Advisory Committee (HICPAC). Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162-e193. CrossRef PubMed
- 6. Chun TT, Judelson DR, Rigberg D, et al. Managing central venous access during a health care crisis. J Vasc Surg. 2020;72(4):1184-1195.e3. CrossRef PubMed
- 7. Emoli A, Cappuccio S, Marche B, Musarò A, Scoppettuolo G, Pittiruti M; Gruppo Aperto di Studio sugli Accessi Venosi Centrali a Lungo Termine. The ISP (Safe Insertion of PICCs) protocol: a bundle of 8 recommendations to minimize the complications related to the peripherally inserted central venous catheters (PICC). Assist Inferm Ric. 2014;33(2):82-89. PubMed
- 8. Lamperti M, Biasucci DG, Disma N, et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur J Anaesthesiol. 2020;37(5):344-376. CrossRef PubMed
- 9. Dawson R. PICC Zone Insertion Method™ (ZIM™): a systematic approach to determine the ideal insertion site for PICCs in the upper arm. J Assoc Vasc Access. 2011;16(3):156-165. CrossRef
- 10. Sharp R, Cummings M, Fielder A, Mikocka-Walus A, Grech C, Esterman A. The catheter to vein ratio and rates of symptomatic venous thromboembolism in patients with a peripherally inserted central catheter (PICC): a prospective cohort study. Int J Nurs Stud. 2015;52(3):677-685. CrossRef PubMed
- 11. Elli S, Bellani G, Cannizzo L, et al. Reliability of cutaneous landmarks for the catheter length assessment during peripherally inserted central catheter insertion: A retrospective observational study. J Vasc Access. 2020;21(6):917-922. CrossRef PubMed
- 12. Elli S, Cannizzo L, Marini A, et al. Evaluation of tip location reliability of intraprocedural ECG vs. chest Xrays in PICC placement. Assist Inferm Ric. 2016 Oct-Dec;35(4):174-179. CrossRef PubMed
- 13. Greca A, Iacobone E, Elisei D, et al. ECHOTIP: A structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in adult patients. J Vasc Access. 2021. CrossRef PubMed
- 14. Chopra V, Flanders SA, Saint S, et al; Michigan Appropriateness Guide for Intravenous Catheters (MAGIC) Panel. The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): Results from a Multispecialty Panel Using the RAND/UCLA Appropriateness Method. Ann Intern Med. 2015;163(6)(suppl):S1-S40. CrossRef PubMed
- 15. Pinelli F, Pittiruti M, Van Boxtel T, et al. GAVeCeLT-WoCoVA Consensus on subcutaneously anchored securement devices for the securement of venous catheters: current evidence and recommendations for future research. J Vasc Access. 2021;22(5):716-725. CrossRef PubMed
- 16. Zerla PA, Canelli A, Cerne L, et al. Evaluating safety, efficacy, and cost-effectiveness of PICC securement by subcutaneously anchored stabilization device. J Vasc Access. 2017;18(3):238-242. CrossRef PubMed
- 17. Scoppettuolo G, Dolcetti L, Emoli A, La Greca A, Biasucci DG, Pittiruti M. Further benefits of cyanoacrylate glue for central venous catheterisation. Anaesthesia. 2015;70(6):758. CrossRef PubMed