 |
AboutOpen | 2021; 8: 88-91 ISSN 2465-2628 | DOI: 10.33393/ao.2021.2284 BRIEF REPORT |
 |
A novel Venturi system to generate high flow with titratable FiO2
ABSTRACT
Venturi-based flow generators are commonly used for noninvasive continuous positive airway pressure (CPAP) of high-flow nasal oxygen (HFNO). The system is simple and allows to increase the total flow while decreasing the FiO2 starting from a single oxygen source.
In this report we describe the characteristics and performance of a novel Venturi system (EasyVEE, Levate, BG, Italy), which allows to vary the size of the port through which ambient air is entrained, hence allowing a continuous modulation of FiO2.
The system allowed to modify FiO2 continuously between 35% and 80% and, consequently, a 1.5- to 4.5-fold increase of the total flow rate. A minimal decrease in entrainment performance was observed for positive end-expiratory pressure levels above 12.5 cmH2O.
EasyVEE system appears to be a simple, flexible, and reliable solution to generate continuous flow for noninvasive respiratory support interfaces.
Keywords: CPAP, Noninvasive ventilation, Acute Respiratory Failure, Oxygen
Received: May 31, 2021
Accepted: September 7, 2021
Published online: October 13, 2021
AboutOpen - ISSN 2465-2628 - www.aboutscience.eu/aboutopen
© 2021 The Authors. This article is published by AboutScience and licensed under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). Commercial use is not permitted and is subject to Publisher’s permissions. Full information is available at www.aboutscience.eu
Background and rationale
Noninvasive ventilatory support, based on free-flow continuous positive airway pressure (CPAP) delivered by helmet or face mask or high-flow nasal oxygen (HFNO), is increasingly used to treat patients with acute respiratory failure (1). During the recent Coronavirus-2019 (COVID-19) pandemic, the use of free-flow system massively spread also outside the intensive care units (2-5). The main advantage of free-flow systems is that an active mechanical ventilator is not required; a flow generator connected to the oxygen pipe or tank can feed a helmet or a face mask to provide CPAP through a positive end-expiratory pressure (PEEP) valve (6), or to nasal cannulas to provide HFNO (7). Flow generators can be either turbine-based or Venturi-based systems.
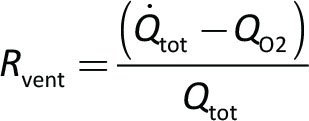
Venturi systems are based on the principle that a high-pressure gas (typically oxygen at 4 atm) is delivered through a small-bore nozzle, reaching a very high speed. Due to Bernoulli’s law, once the high-speed gas moves into a larger conduit, it generates a decrease of the lateral pressure, which becomes subatmospheric and entrains another gas (air) from the external atmosphere. In this way, starting from a pure flow of oxygen (QO2), it is possible to achieve a much higher flow of a mixture of gas (Qtot), at a variable FiO2. For each Venturi system, it is hence possible to calculate the flow of gas entrained (Qentr) for a given QO2, where the ratio 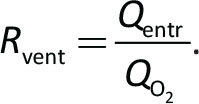 . For example, Rvent = 3 indicates that for each 1 L/min of oxygen flowing through the nozzle, three additional liters/minute of gas is entrained, resulting in a total flow of 4 L/min. The final flow (Qtot) depends on QO2 and Rvent according to the following formula:
. For example, Rvent = 3 indicates that for each 1 L/min of oxygen flowing through the nozzle, three additional liters/minute of gas is entrained, resulting in a total flow of 4 L/min. The final flow (Qtot) depends on QO2 and Rvent according to the following formula:
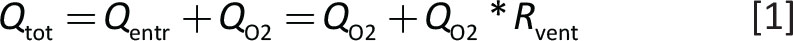
The FiO2 of Qtot (if the gas entrained is air) equals
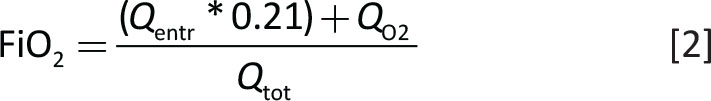
which, combined with Equation [1] and simplified becomes:
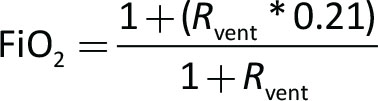
Hence, if Rvent does not change, varying QO2 to the nozzle will not vary the FiO2 of Qtot, but only Qtot itself.
Rvent depends mainly not only on the diameter and shape of the nozzle orifice but also on the pressure downstream, as positive pressure decreases the entrainment ability of Venturi.
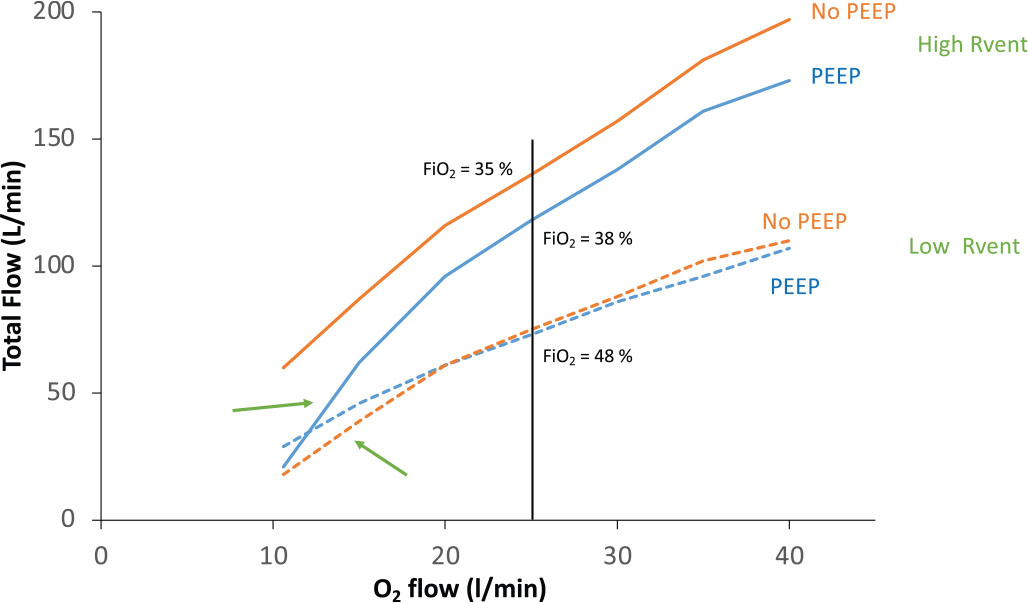
From a clinical standpoint, this is relevant, since when delivering free-flow CPAP using a Venturi system to generate the flow, any PEEP increase will cause an FiO2 increase, which might be misinterpreted as a patient’s response to PEEP. Finally Rvent tends to decrease for low QO2, due to the loss of entrainment at lower gas speeds. A typical behavior of a Venturi system is displayed in Figure 1.
Description of the system
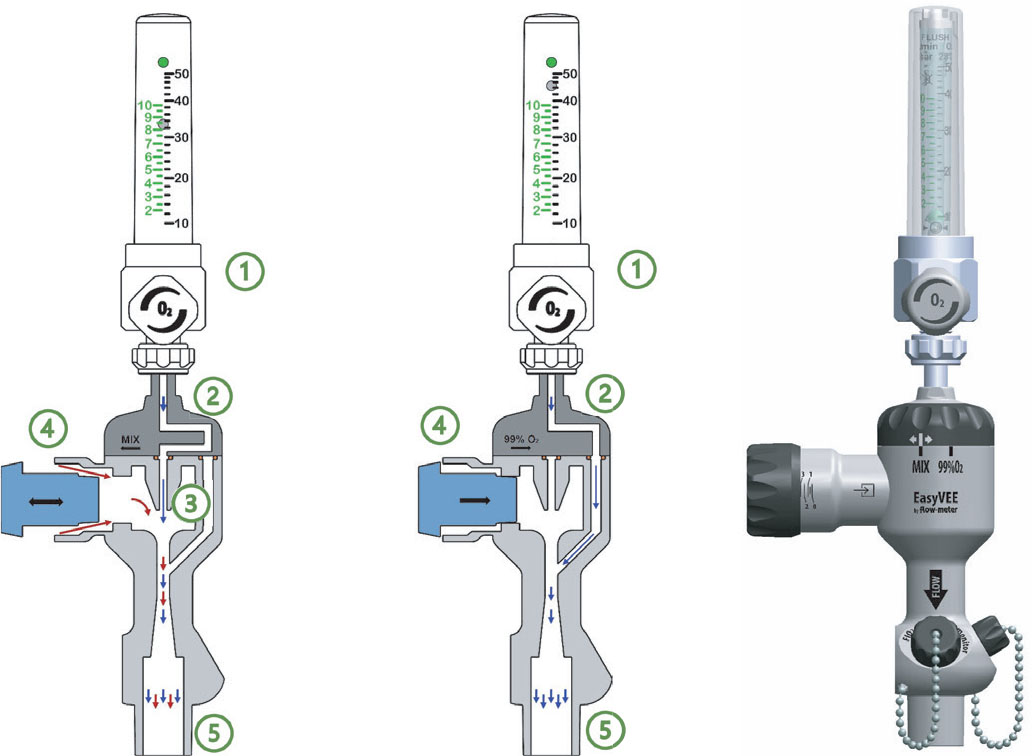
We herein describe and characterize a novel Venturi system (EasyVee flowmeter, Levate, Bergamo, Italy), coupled with a variable area oxygen flowmeter, connected to a high-pressure (4 bar) O2 source. The Venturi nozzle (with a diameter of 1.1 mm) is characterized by a nominal Rvent of approximately 4.5 when operating without downstream pressure. A novel solution is that the size of the aspiration port (open to ambient air) can be modulated, by means of a nonius, from full opening to complete closure (Fig. 2). The excursion progresses continuously, but six precalibrated marks are put in order to facilitate Qentr (and hence FiO2) titration with the use of a table or an app.
Because of the size of the nozzle, the maximum achievable flow from a standard 4-bar oxygen wall port equals 38-40 L/min, even if the flow meter is opened to full scale. Therefore, when the nonius is completely closed to deliver pure oxygen (FiO2 100%), the total flow might be inadequate to provide noninvasive CPAP support; a novel solution is the presence of a switch to bypass the Venturi nozzle, achieving up to 70 L/min oxygen flows.
Methods
In this bench study we evaluated the performance of the novel Venturi system, in terms of total flow generated and FiO2 for different QO2, nonius position, and PEEP loads, to simulate different clinical scenarios. Total flow and FiO2 were measured by VT Plus HF (Fluke Biomedical, USA). FiO2 was measured additionally by PICK-O2 (Medizintechnik Juergen K. Kranz GmbH) and values were averaged to obtain the measured FiO2 (FiO2,meas). Theoretical FiO2 (FiO2,th) was calculated as:
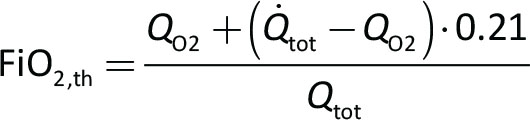
and compared with FiO2,meas to verify internal data consistency.
For each condition Rvent was calculated as:
Results
As expected FiO2,meas and FiO2,th were tightly correlated (Fig. 3).
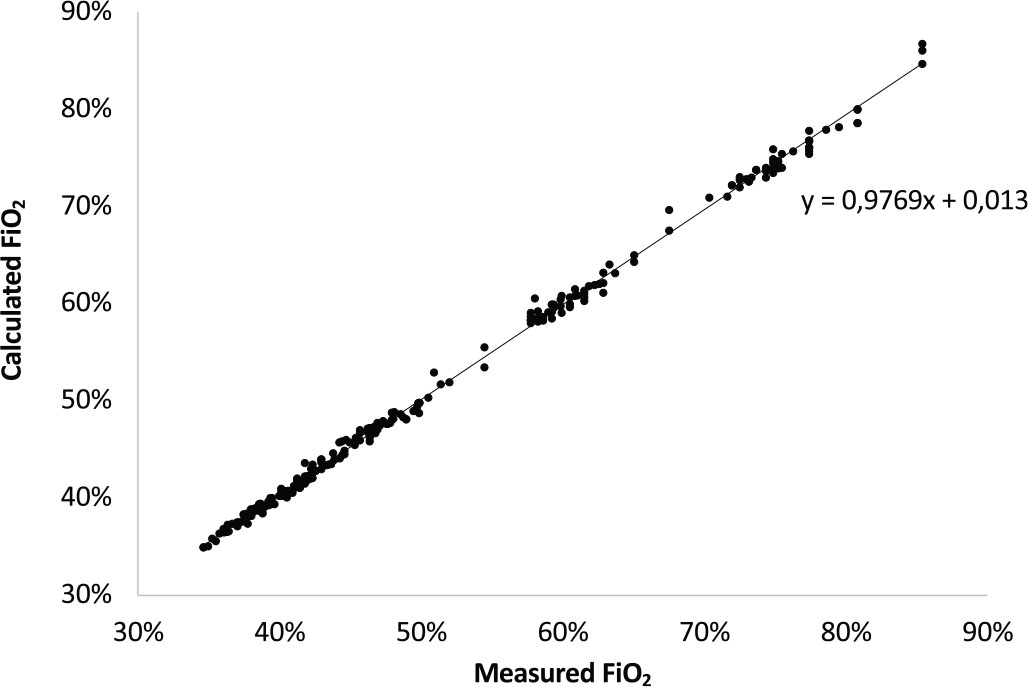
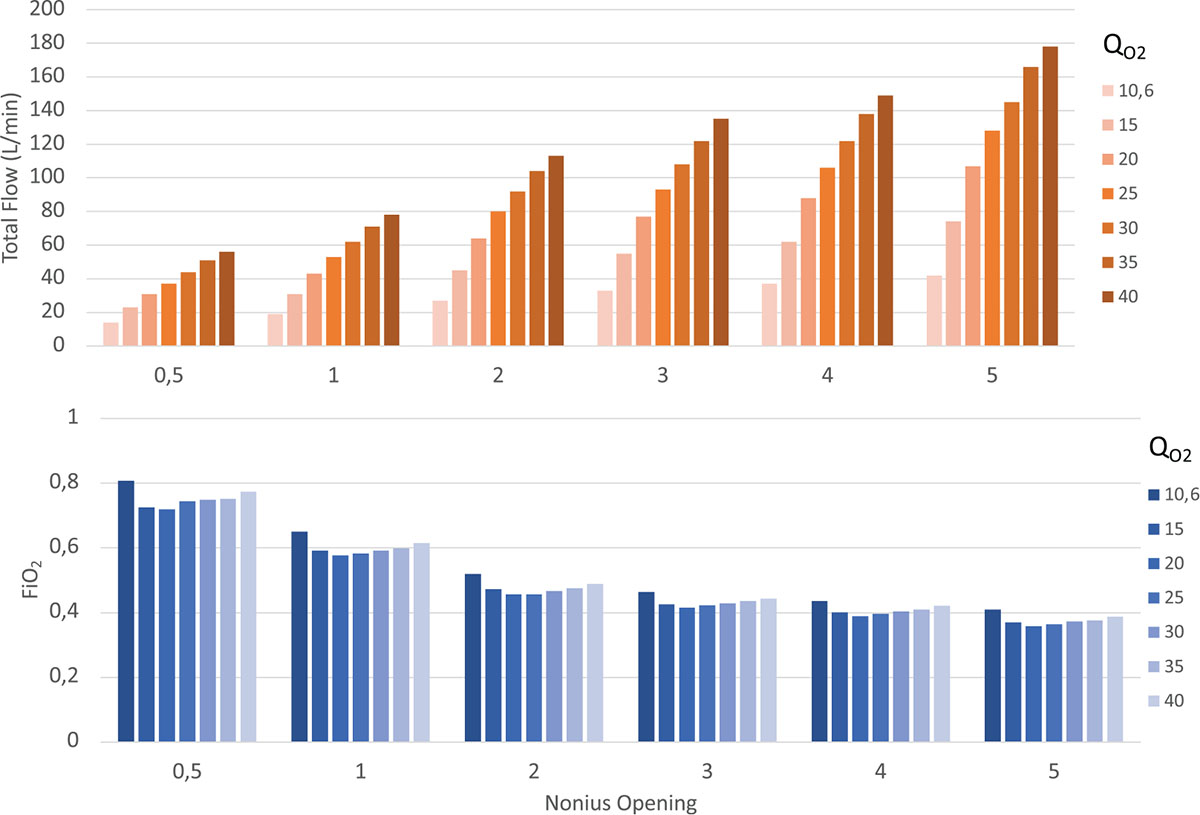
Figure 4 shows the performance of the novel Venturi system for different QO2 and position of the nonius, for a PEEP value of 7.5 cmH2O. As expected, progressively closing the nonius leads to a decrease of the air entrained by the Venturi (decreasing Rvent) and hence Qtot (upper panel), allowing to achieve higher FiO2 (lower panel), in the range between 35% and 80%.
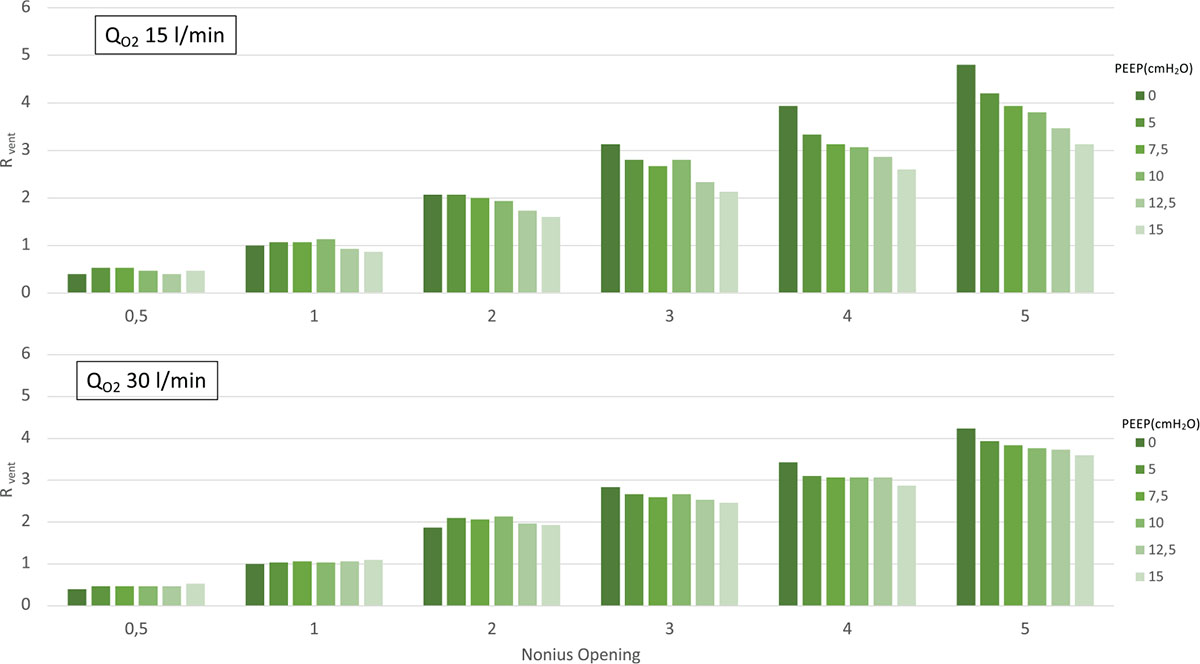
As shown in Figure 5, the performance of the novel Venturi system, measured as capacity to entrain air (Rvent), remained rather stable over a wide range of PEEP, showing a sensible impact only for PEEP levels above 12.5 cmH2O, particularly if a low QO2 is used (upper panel).
Discussion
In this report we described the pneumatic performance of the EasyVEE system, a Venturi flow generator equipped with an adjustable air entraining port and a single extended-range flowmeter. The novel system was very flexible, in generating high-flow gas mixture, with a simple control to titrate FiO2 and a constant performance over a wide range of PEEP and QO2.
As mentioned, an adequate flow of fresh gas is necessary in order to efficiently deliver CPAP or HFNO. This is often achieved by Venturi systems, which drop the FiO2 proportionally to their efficiency in gas entrainment. Standard Venturi systems are typically built with a fixed (not adjustable) port for air entrainment; therefore, a second flowmeter is needed to increase FiO2 by addition of oxygen to the gas mixture generated by the Venturi. At variance from these, the EasyVEE foresees a progressive reduction of the air opening, so that the net result is an adjustable Rvent and an increase in FiO2.
Another crucial point of the Venturi systems is the loss of performance for increasing back pressures, typically due to PEEP increase. In this respect, the Easy-VEE maintains a relatively constant performance over a wide range of PEEP levels, albeit the use of a direct FiO2 measure or custom tables for the device is recommended to determine the exact FiO2 after any therapeutic adjustment.
In conclusion the EasyVEE system appears to be a simple, flexible, and reliable solution to generate continuous flow for noninvasive respiratory support interfaces.
Disclosures
Conflict of interest: Both authors are coinventors on patents and receive consultancy fees from Flow-Meter SPA (Levate, BG, Italy) for a matter related to the topic of the article.
Financial support: None.
References
- 1. Ferreyro BL, Angriman F, Munshi L, et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure: a systematic review and meta-analysis. JAMA. 2020;324(1):57-67. CrossRef PubMed
- 2. Bellani G, Grasselli G, Cecconi M, et al. Noninvasive ventilatory support of patients with COVID-19 outside the intensive care units (WARd-COVID). Ann Am Thorac Soc. 2021;18(6):1020-1026. CrossRef PubMed
- 3. Coppadoro A, Zago E, Pavan F, et al. The use of head helmets to deliver noninvasive ventilatory support: a comprehensive review of technical aspects and clinical findings. Crit Care. 2021;25(1):327. CrossRef PubMed
- 4. Alharthy A, Faqihi F, Noor A, et al. Helmet continuous positive airway pressure in the treatment of COVID-19 patients with acute respiratory failure could be an effective strategy: a feasibility study. J Epidemiol Glob Health. 2020;10(3):201-203. CrossRef PubMed
- 5. Aliberti S, Radovanovic D, Billi F, et al. Helmet CPAP treatment in patients with COVID-19 pneumonia: a multicentre cohort study. Eur Respir J. 2020;56(4):56. CrossRef PubMed
- 6. Brusasco C, Corradi F, De Ferrari A, Ball L, Kacmarek RM, Pelosi P. CPAP devices for emergency prehospital use: a bench study. Respir Care. 2015;60(12):1777-1785. CrossRef PubMed
- 7. Garofalo E, Bruni A, Pelaia C, et al. Evaluation of a new interface combining high-flow nasal cannula and CPAP. Respir Care. 2019;64(10):1231-1239. CrossRef PubMed